Raynaud’s phenomenon is an exaggerated physiological response of blood vessels in the distal extremities to emotional stress and cold. It can be idiopathic or secondary to a connective tissue disorder, such as scleroderma or systemic lupus erythematosus. Treatment for Raynaud’s phenomenon consists primarily of lifestyle modifications; if unsuccessful, pharmacotherapy with dihydropyridine calcium channel blockers can be added. Botulinum toxin (BTX-A) is a neurotoxic protein produced by Clostridium botulinum spores. While most widely known for its cosmetic use, BTX-A has many therapeutic utilities due to its ability to inhibit multiple neurotransmitters. In this report, JDD authors present a patient with Raynaud’s phenomenon refractory to standard therapies whose symptoms resolved after treatment with BTX-A. Follow-up with the patient after one and five years showed no relapse or recurrence of symptoms.
INTRODUCTION
Raynaud’s phenomenon is an exaggerated physio-logical response of blood vessels in the distal extremities, mainly in the digits, to emotional stress and cold. Raynaud’s phenomenon can be primary idiopathic or secondary to a connective tissue disorder, such as scleroderma or systemic lupus erythematosus. It can also occur secondary to a constant vibratory stimulus, notably in string musicians, construction workers, and similar occupations requiring manual dexterity and exposure to constant vibration.1 First-line treatment generally involves lifestyle modifications such as avoiding cold, minimizing stress, and smoking cessation.2,3 If unsuccessful, first-line pharmacotherapy is dihydropyridine calcium channel blockers (CCBs). Alternative therapies include phosphodiesterase-5-inhibitors, topical glyceryl trinitrate, prostacyclin analogues (iloprost), and endothelin receptor antagonists.4,5
Botulinum toxin-A (BTX-A) is a neurotoxic protein produced by Clostridium botulinum spores. While most widely known for its cosmetic applications, BTX-A also has utility in treatment of migraines, torticollis, detrusor hyperactivity, spasticity, strabismus, and blepharospasm.6 In this report, JDD authors Usman Asad BS, Brett Austin MD, Michelle Tarbox MD, and Brent Paulger MD present a patient with Raynaud’s phenomenon refractory to standard therapies whose symptoms resolved after treatment with BTX-A.
CASE REPORT
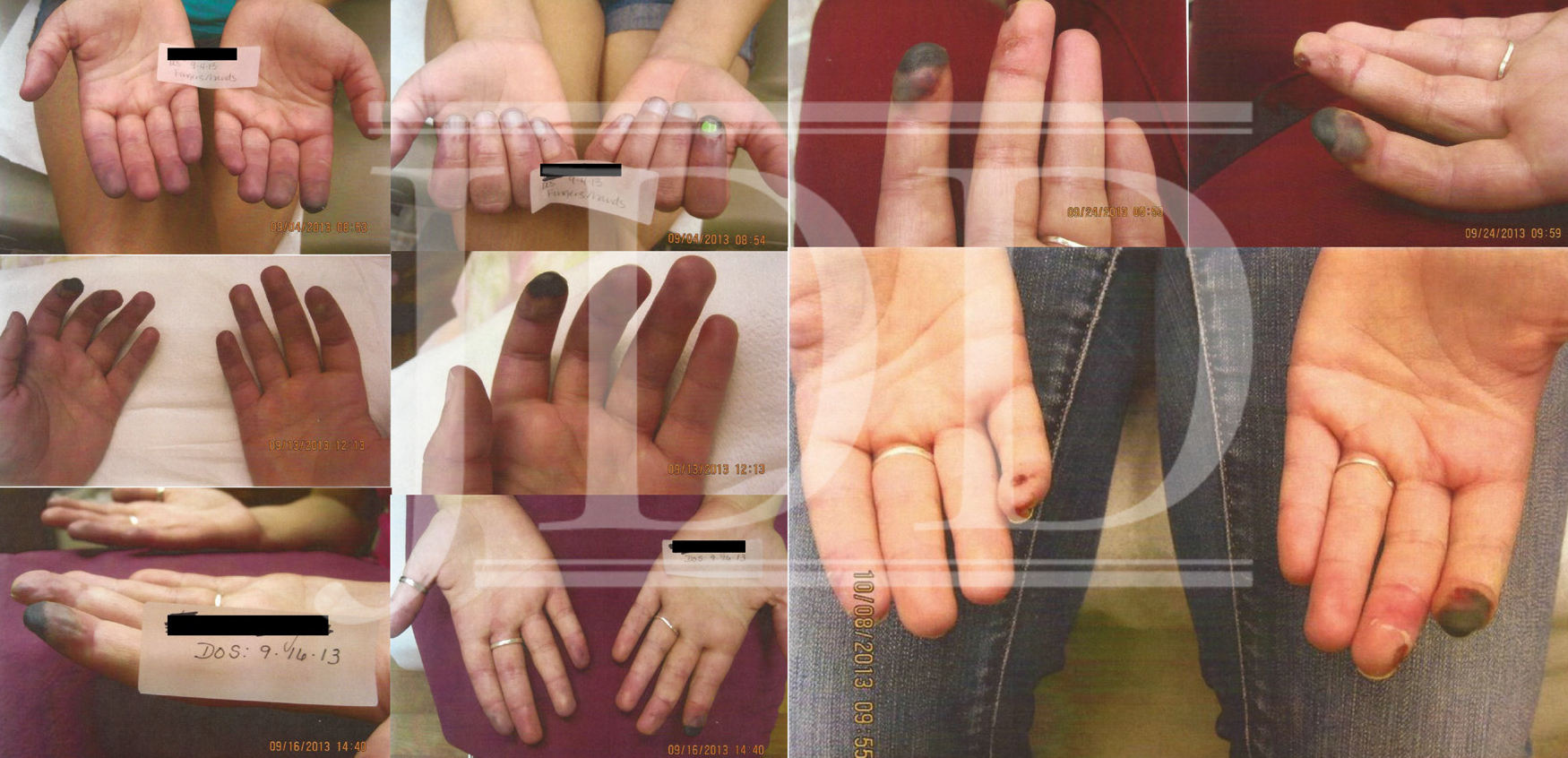

A vial of BTX-A (100MU) was diluted in preservative-free normal saline for a final concentration of 2U/0.1mL. A cumulative total dose of 94 MU of BTX-A was injected into the palmar side of the digits along the digital vessels of each finger. At her followup visit three days post-injection, the patient reported that her fingers felt warm for the first time in months. Although her left index fingertip was still in a state of necrosis, the patient was able to straighten her finger, which she had not been able to do for weeks (Figure 2). She also no longer complained of color change or vasospasms. The injections helped to save most of her fingers and stopped the spread of the infarcted areas. Follow-up with the patient one year later showed that she had had no further episodes and had not received any further treatments. At that time, her lupus was well controlled, which may have contributed to her positive response. After five years, the patient similarly reported that she had had no recurrence of symptoms or further vasospastic episodes.
DISCUSSION
We suspect that vibratory stimulus from our patient’s frequent violin rehearsal may have played a role in the severity of her symptoms, as with other causes of occupational vibratory Raynaud’s. The exact mechanism of action of BTX-A in treatment of Raynaud’s phenomenon remains unknown. A study by Stone et al. proposed one possible mechanism. In an experimental study using rodents, BTX-A was observed to block sympathetic nerve conduction, thereby causing arteriolar vasodilation and increased blood flow.7 Zhou et al. similarly showed that BTX-A could significantly inhibit electrical stimulation-induced arteriole vasoconstriction through the sympathetic pathway.8 This has been the most plausible mechanism explaining its effectiveness in Raynaud’s phenomenon. However, further studies are needed to identify its exact mode of action in alleviating pain and relieving vasospasm. According to the literature, there are several cases supporting the use of BTX-A for Raynaud’s phenomenon.9,10However, reports of long-term effects of botulinum toxin use for this condition are lacking. In our case, the patient showed no relapse of her symptoms after treatment even five years later, showing that BTX-A is a viable option for long-term resolution of symptoms of Raynaud’s phenomenon. The management of Raynaud’s phenomenon in its most severe form can be challenging. In this patient, her symptoms were serious and refractory to standard therapies. BTX-A was effective in providing quick relief of her pain and vasospasms. Without its administration, this patient may have suffered from further necrosis and possible loss of her digits. Our case highlights the importance of looking for alternative treatments when traditional therapies fail and of researching the newest developments in therapeutics.
REFERENCES
-
- Fardoun MM, Nassif J, Issa K, Baydoun E, Eid AH. Raynaud’s Phenomenon: A Brief Review of the Underlying Mechanisms. Front Pharmacol. 2016;7:438.
- Levien TL. Advances in the treatment of Raynaud’s phenomenon. Vasc Health Risk Manag. 2010;6:167–77.
- Goundry B, Bell L, Langtree M, et al. Diagnosis and management of Raynaud’s phenomenon. BMJ. 2012;344:e289.
- Landry GJ. Current medical and surgical management of Raynaud’s syndrome. J Vasc Surg. 2013;57:1710–6.
- Herrick AL. Management of Raynaud’s phenomenon and digital ischemia. Curr Rheumatol Rep. 2013;15:303.
- Cartee TV, Monheit GD. An overview of botulinum toxins: past, present, and future. Clin Plast Surg. 2011;38:409–26.
- Stone AV, Koman LA, Callahan MF, et al. The effect of botulinum neurotoxin-A on blood flow in rats: a potential mechanism for treatment of Raynaud phenomenon. J Hand Surg Am. 2012;37:795–802.
- Zhou Y, Liu Y, Hao Y, et al. The mechanism of botulinum A on Raynaud syndrome. Drug Des Devel Ther. 2018;12:1905-1915. Published 2018 Jun 26.
- Sycha T, Graninger M, Auff E, Schnider P. Botulinum toxin in the treatment of Raynaud’s phenomenon: a pilot study. Eur J Clin Invest. 2004;34:312–313. 1
- Van Beek AL, Lim PK, Gear AJ, Pritzker MR. Management of vasospastic disorders with botulinum toxin A. Plast Reconstr Surg. 2007;119:217–226.
SOURCE
Asad, U., Austin, B., Tarbox, M., & Paulger, B. (2019). Botulinum toxin in the long-term treatment of refractory Raynaud’s phenomenon. Journal of drugs in dermatology: JDD, 18(9), 943-945.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.