Patients with darker skin types are susceptible to developing other pigmentary disorders besides melasma. At SOCU 2022, Dr. Heather Woolery-Lloyd, Director of the Skin of Color Division at the University of Miami Miller School of Medicine, gave a fascinating overview of various pigmentary disorders that can affect patients with skin of color and provided clinical pearls immediately useful in our practice.
Post-Inflammatory Pigment Alteration
Post-inflammatory pigment alteration (PIPA) is the most common pigmentary disorder in skin of color due to increased reactivity of melanocytes. This can occur in response to a wide variety of triggers, including acne, bug bites, burns, injuries, eczema, etc. Patients are often more concerned with the hyperpigmentation than the acne, as a hyperpigmented macule can take up to four months to fade. Hypopigmentation is more difficult to treat than hyperpigmentation. Prevention is key in both hyper- and hypopigmentation.
Failing that, hydroquinone (HQ) and hydroquinone-free skin brighteners can be used to treat hyperpigmentation, while bimatoprost and self-tanner can be tried for hypopigmentation. To avoid HQ halo (lightening around dark spots), patients should apply HQ to dark spots using a cotton-tipped applicator—not their fingers—prior to applying retinoid to the full face. HQ sensitivity can occur in a subset of patients due to the HQ itself or to sodium metabisulfite (a common preservative in HQ preparations). Dr. Woolery-Lloyd reminded us that continued use of HQ preparations despite irritation can cause PIPA. For darker skin eczema patients, a compounding pharmacy can add hydroquinone (HQ) to steroids like clobetasol during treatment and azelaic acid to triamcinolone after skin clearance to help maintain clearance and ward off PIPA.
Clinical Pearl: Treat underlying causes of inflammation aggressively to prevent post-inflammatory hyperpigmentation.
Lichen Planus Pigmentosus
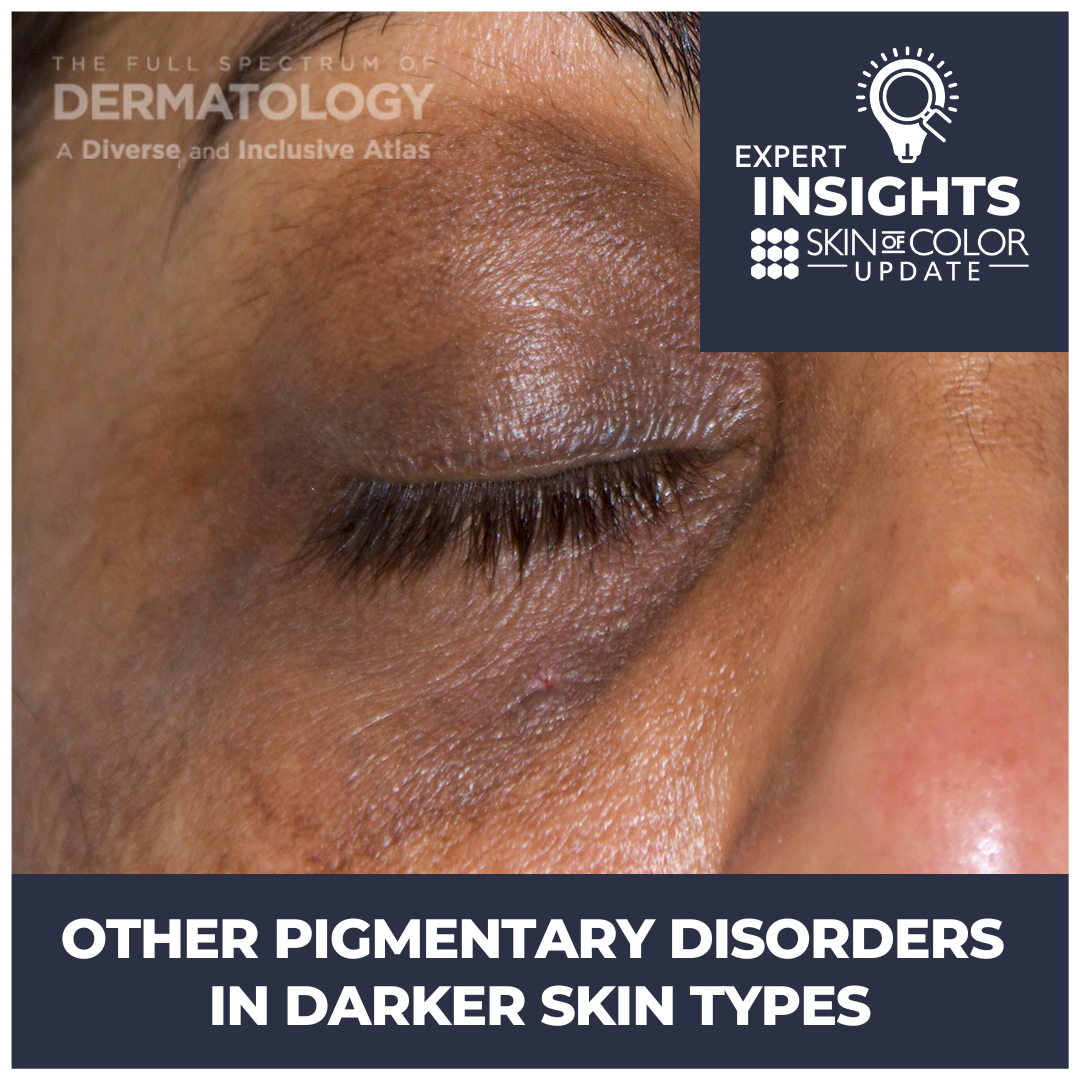
Lichen planus pigmentosus (LPP) is a challenging pigmentary disorder to treat. It starts in the third or fourth decade of life, and is more common in females. Lesions initially appear as small, ill-defined oval to round macules, often on the face and neck, which later become confluent to form large areas of pigmentation. Pigmentation in different patients varies from slate grey to brownish-black. Dr. Woolery-Lloyd recounted the case of a patient who had good response to six months of azelaic acid 20% mixed with hydrocortisone 2.5%.
LPP is often confused with ashy dermatosis and erythema dyschromicum perstans (EDP). All of these entities are lichenoid reactions associated with pigment incontinence. However, LPP is usually found on the face and neck and less commonly on the forearms, while ashy dermatosis is seen more often on the trunk and extremities. EDP classically presents with a preceding ring of erythema, and the term is favored over ashy dermatosis in North America.
Ochronosis
Ochronosis is a paradoxical darkening of the skin that occurs with long-term HQ use (usually over-the-counter 2% used for years). Presentation typically begins with redness followed by blue-black patches on the face where HQ is applied, and can progress to blue-black papules and nodules in severe cases. Histology shows banana-shaped ochronotic pigment in the dermis (there is no melanin). Treatments include convincing the patient to stop HQ, anti-inflammatories such as topical steroids, azelaic acid for background hyperpigmentation, and time.
Clinical Pearl: To confirm diagnosis of ochronosis, look for photoaccentuated dark pigment on the cheeks and alar rim, obtain a thorough HQ use history, and confirm the diagnosis with a 2 mm punch biopsy from the lateral cheek.
Drug-Induced Facial Hyperpigmentation
Drug-induced facial hyperpigmentation is common in the African American population because a large fraction of the population is on antihypertensives. Clinically, drug-induced facial hyperpigmentation presents as dark brown hyperpigmentation on the face (not slate grey). The most common cause is hydrochlorothiazide. Discuss switching to a non-photosensitizing BP agent if possible with the patient’s PCP, start a hydrocortisone 2.5% cream (or a steroid-sparing topical anti-inflammatory) and an HQ-free skin brightener such as azelaic acid, and counsel the patient about strict photoprotection.
Progressive Macular Hypomelanosis
Progressive macular hypomelanosis (PMH) has been described in darkly pigmented young women and men of all races. It is characterized by asymptomatic, ill-defined, nummular, non-scaly hypopigmented spots on the trunk. These macules are usually confluent in and around the midline and rarely extend to the proximal extremities/neck/head region. There is no preceding inflammation. The disease usually progresses slowly over many decades, with spontaneous disappearance after mid-life. Differential diagnoses include pityriasis alba and tinea versicolor. PMH is thought to be caused by P. acnes production of a factor that interferes with melanogenesis. Red follicular fluorescence from P. acnes may be noted on Wood’s lamp exam, and improvement with topical antimicrobials and oral doxycycline can be seen.
Other Pigmentary Disorders
Maturational dyschromia is the darkening of malar cheeks and forehead with age. This is a diagnosis of exclusion, so rule out treatable causes first. Riehl melanosis is a likely underdiagnosed contact dermatitis that can be preceded by mild erythema and pruritus, followed by diffuse to reticulated hyperpigmentation. It is more common on sites where cosmetics are applied, and patch testing may be helpful. Pityriasis alba is a common hypopigmented dermatitis that occurs in up to 5% of preadolescent children. This self-limited disorder usually resolves by adulthood. It is more apparent in the summer. Finally, idiopathic guttate hypomelanosis correlates with age and UV exposure. Treatment includes reassurance, topical tretinoin, localized superficial dermabrasion, and self-tanner.
Patients with darker skin types can develop a variety of other pigmentary disorders besides melasma. Familiarity with these conditions is key to accurate diagnosis, appropriate workup, and timely treatment.
Did you enjoy this article? Find more here.