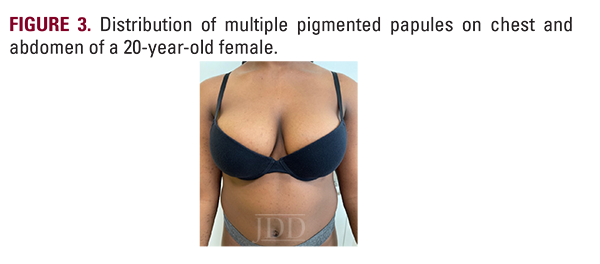
Syringomas are benign neoplasms derived from eccrine sweat glands. Eruptive syringomas are a subtype of syringomas and are typically located on the chest, neck, and abdomen during puberty or childhood. Herein, JDD authors Jennifer Wang BA, Nyousha Yousefi MD, Edward Heilman MD FAAD FCAP, and Jared Jagdeo MD MS present a 20-year-old African American female with an atypical case of eruptive syringomas, characterized by an unusual distribution on her chest, abdomen, and anterior and posterior bilateral extremities. This case underscores the importance of recognizing diverse presentations of skin conditions in patients with skin of color and adds to the limited reports of eruptive syringoma in these populations. The authors present and emphasize this atypical manifestation of eruptive syringomas in an individual with darker skin to promote awareness and improve diagnosis and patient outcomes.
INTRODUCTION
CASE DESCRIPTION


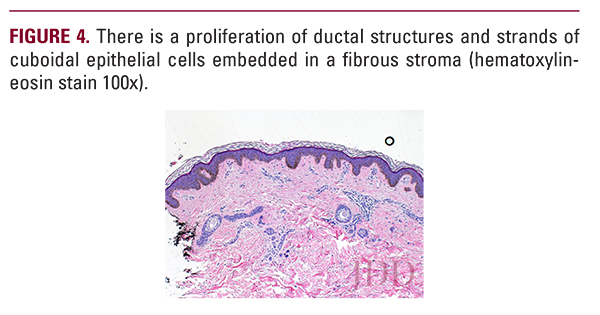
 A 4 mm skin punch biopsy from the left upper thigh was taken. There was a subtle proliferation of ductal epithelial elements and thin cords composed of cuboidal epithelial cells embedded in a perfectly normal stroma. The ductal elements exhibited an outer layer of cuboidal epithelial cells and a luminal layer containing pale staining cytoplasm. The ducts contained eosinophilic secretion-like material. These findings are diagnostic of a syringoma (Figures 4 and 5).
A 4 mm skin punch biopsy from the left upper thigh was taken. There was a subtle proliferation of ductal epithelial elements and thin cords composed of cuboidal epithelial cells embedded in a perfectly normal stroma. The ductal elements exhibited an outer layer of cuboidal epithelial cells and a luminal layer containing pale staining cytoplasm. The ducts contained eosinophilic secretion-like material. These findings are diagnostic of a syringoma (Figures 4 and 5).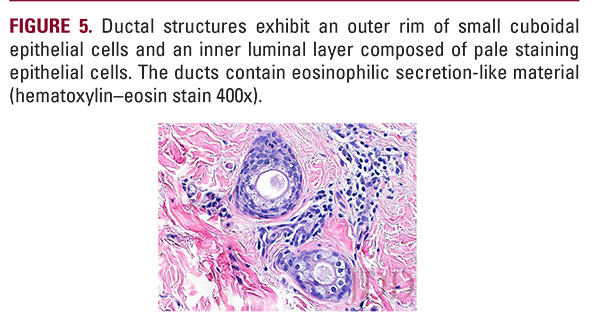
DISCUSSION
Herein, the authors present an atypical case of eruptive syringoma in an African American patient. Eruptive syringomas are a rare subtype of syringomas, with a higher incidence in women and African American and Asian patients.1,5,6 Eruptive syringomas typically present as multiple 2 to 5 mm yellow or brown, non-scaly, flat-topped papules.1,5,7 Dermoscopy may reveal fine reticulate brown lines on a light brown background.8 Histopathologically, eruptive syringomas consist of a distinctive pattern of small, “comma” or “tadpole-like””sweat ducts within a fibrotic stroma in the dermis, without extension into the subcutaneous layer.1,5,7 Histological evaluation is required for the diagnosis of eruptive syringoma.3
DISCLOSURES
REFERENCES
-
- Lei H, Wang Z, Ma X, et al. Eruptive syringomas: summary of ninety cases and a brief literature review. J Cosmet Dermatol. 2023;22(3):1128-1133.
- Friedman SJ, Butler DF. Syringoma presenting as milia. J Am Acad Dermatol. 1987;16(2 Pt 1):310-314.
- Jamalipour M, Heidarpour M, Rajabi P. Generalized eruptive syringomas. Indian J Dermatol. 2009;54(1):65-67.
- Teixeira M, Ferreira M, Machado S, et al. Eruptive syringomas. Dermatol Online J. 2005;11(3):34.
- Huang A, Taylor G, Liebman TN. Generalized eruptive syringomas. Dermatol Online J. 2017;23(9).
- Medscape. Syringoma. Available at: https://emedicine.medscape.com/ article/1059871-overview#a7. Accessed November 2, 2023.
- Avhad G, Ghuge P, Jerajani HR. Generalized eruptive syringoma. Indian J Dermatol. 2015;60(2):214.
- Aleissa M, Aljarbou O, AlJasser MI. Dermoscopy of eruptive syringoma. Skin Appendage Disord. 2021;7(5):401-403.
- Lee AY, Kawashima M, Nakagawa H, et al. Generalized eruptive syringoma. J Am Acad Dermatol. 1991;25(3):570-1.
- Guitart J, Rosenbaum MM, Requena L. ‘Eruptive syringoma’: a misnomer for a reactive eccrine gland ductal proliferation? J Cutan Pathol. 2003;30(3):202-205.
- Hassab-El-Naby HMM, Nouh AH. Syringomatous dermatitis: a myth or an existing entity? Arch Dermatol Res. 2023;315(6):1649-1654.
- Husein-El Ahmed H, Aneiros-Fernandez J, Aneiros-Cachaza J. “Eruptive” facial syringomas: an inflammatory skin reaction? Skinmed. 2012;10(3):186-187.
- Wallace ML, Smoller BR. Progesterone receptor positivity supports hormonal control of syringomas. J Cutan Pathol. 1995;22(5):442-445.
- Maeda T, Natsuga K, Nishie W, et al. Extensive eruptive syringoma after liver transplantation. Acta Derm Venereol. 2018;98(1):119-120.
- Gómez MI, Perez B, Azana JM, et al. Eruptive syringoma: treatment with topical tretinoin. Dermatology. 1994;189(1):105-106.
- Frazier CC, Camacho AP, Cockerell CJ. The treatment of eruptive syringomas in an African American patient with a combination of trichloroacetic acid and CO2 laser destruction. Dermatol Surg. 2001;27(5):489-492.
- Zaldivar-Fujigaki JL, Achell Nava L. Botulinum toxin A as monotherapy for syringoma. J Cosmet Dermatol. 2021;20(5):1393-1395.
- Markiewicz E, Karaman-Jurukovska N, Mammone T, et al. Post-inflammatory hyperpigmentation in dark skin: molecular mechanism and skincare implications. Clin Cosmet Investig Dermatol. 2022;15:2555-2565.
- Lyman M, Mills JO, Shipman AR. A dermatological questionnaire for general practitioners in England with a focus on melanoma; misdiagnosis in Black patients compared to White patients. J Eur Acad Dermatol Venereol. 2017;31(4):625-628.
- Diao JA, Adamson AS. Representation and misdiagnosis of dark skin in a large-scale visual diagnostic challenge. J Am Acad Dermatol. 2022;86(4):950-951.
SOURCE
Wang, Jennifer, et al. “Inverse Eruptive Syringoma in a Skin of Color Patient.” Journal of Drugs in Dermatology: JDD 23.7 (2024): 564-566.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.