Hidradenitis Suppurativa (HS) is a challenging dermatological condition characterized by painful, recurrent, and often disfiguring skin lesions. In this article, we will explore the expert insights of Dr. Ginette Okoye, Professor and Chair of the Howard University Department of Dermatology, as she discussed her approach to and experience with treating patients with HS at the 2023 Skin of Color Update in New York City. Dr. Okoye emphasizes the multifactorial nature of HS, focusing on its primary inciting issue – follicular occlusion. Her approach involves a holistic perspective that includes a combination of medical, lifestyle, and surgical interventions to provide comprehensive care for HS patients.
UNDERSTANDING HIDRADENITIS SUPPURATIVA
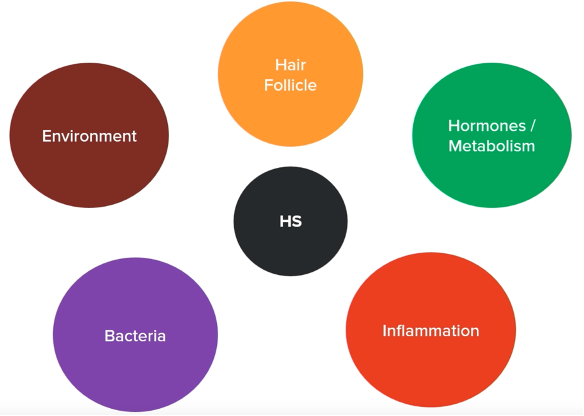
HS is a multifactorial disease with a primary inciting factor: follicular occlusion. This condition primarily involves the infundibular area of hair follicles, leading to occlusion, dilation, rupture, and inflammation of the follicle.1 HS can occur in various body areas, most commonly the underarms and inguinal folds. However, it can also affect areas like the medial thighs, posterior neck, or even behind the knees. Chronic HS often results in the formation of sinus tracts, which are debris-filled tunnels interconnecting the affected, inflamed hair follicles.1
To help patients understand this complex condition, Dr. Okoye often draws diagrams (Figure 1) highlighting the various elements involved in the disease process and the alternative treatments available for each component. This graphic diagram often serves to reassure patients that there are multiple treatment options, providing hope even for those who may feel disheartened by the disease’s challenges.
Hair Follicle
Dr. Okoye starts the discussion with an overview of the hair follicle as the primary issue.
Role Of Laser Hair Removal
One of the primary treatment options Dr. Okoye emphasizes is laser hair removal. She lauds the effectiveness of this procedure, particularly in early-stage disease. Laser hair removal is crucial because it not only addresses the inciting issue by removing hair follicles but may also have a bactericidal effect on specific microorganisms, potentially contributing to the reduction of new HS lesions.2
For patients with recurring lesions in areas like the underarms, laser hair removal remains a viable option, as it can significantly reduce the development of new HS lesions. Dr. Okoye recommends the use of the Nd:YAG laser, especially a no-contact handpiece device that is well-tolerated by patients.
Managing the Environment
Dr. Okoye emphasizes the importance of managing the environment in HS patients. Patients are encouraged to reduce friction and pressure on affected areas. Practical recommendations include wearing looser, non-rigid fabrics to minimize friction, using long boxer briefs, or rotating underwear types to avoid repetitive friction from the seams. For patients with sedentary lifestyles, incorporating sit-stand options or doughnut pillows can help relieve pressure in the buttocks and posterior thighs. Moisture-wicking undergarments (not cotton!) are recommended, as they prevent sweat-induced irritation and friction.
Dietary modifications, such as reducing carbohydrate intake or avoiding dairy, are also discussed. Dr. Okoye acknowledges that while these dietary changes are not universally effective and data is lacking, they have shown promise in some patients and are worth trying. Finally, smoking cessation is strongly encouraged, as it plays a pivotal role in HS management.
Hormones and Metabolism
Dr. Okoye delves into the role of hormones and metabolism in HS management.
Hormonal Therapy
For patients with HS flares associated with their menstrual cycle or pregnancy, hormonal treatments are considered. Spironolactone, an anti-androgen, is often prescribed at varying doses (ranging from 50 to 200 milligrams per day) based on the patient’s tolerance and response.
Progesterone-only contraceptives, such as IUDs and subcutaneous implants, are discouraged due to their androgenic properties, which can exacerbate HS. Make sure to specifically ask your patient about IUDs as this may commonly be overlooked and is not often listed on their medication lists.
Patients on oral contraceptive pills are advised to choose those with lower androgenic potential, such as drospirenone or norgestimate.
Metabolic Therapy
Metformin is recommended for patients showing signs of insulin resistance or metabolic anomalies. The extended-release version is preferred, starting at 500 milligrams with their evening meal, with gradual dose escalation to 2000 milligrams per day if tolerated.
Dr. Okoye highlights the importance of testing for insulin resistance, specifically with a fasting glucose and fasting insulin as a normal HbA1c does not mean the patient has a normal glucose metabolism. Using these two values, one can calculate the HOMA-IR (Homeostatic Model Assessment for Insulin Resistance), which approximates insulin resistance and can potentially lead to referrals to endocrinology colleagues for further evaluation and management.
She also mentions the promising effects of off-label use of Glucagon-like Peptide-1 (GLP-1) agonists in treating HS.3 This class of diabetes medication reduces insulin resistance, inhibits glucagon production, induces satiety, and leads to weight loss, all of which are outcomes that may overall result in better HS control. Nevertheless, more research is needed, and this group of medications may not always be consistently covered by insurance which would hinder its use in practice.
Bacteria
Antibacterial Interventions
While acknowledging that HS is not an infectious disease, Dr. Okoye recommends the use of antiseptic washes two to three times a week to reduce bacterial colonization on the skin. Cleansers containing benzoyl peroxide, chlorhexidine, sodium hypochlorite, or zinc pyrithione are also recommended.
Bleach baths and targeted antibiotics, such as doxycycline and clindamycin, are employed for flare control. The antibiotic ertapenem is reserved for severe cases, typically administered intravenously for six weeks. Below are the recommended regimens for these treatment options:
-
- Bleach baths: ¼ cup of regular bleach to a full tub of water (bathtub typically holds ~40 gallons)
- Doxycyline 100mg BID for 2-4 weeks
- Clindamycin 300mg TID for 2 weeks
- IV Ertapenem x 6 weeks great bridge to surgery or long-term biologic therapy
Inflammation
Addressing Inflammation with Biologics
Dr. Okoye discusses the use of biologics, including adalimumab, infliximab, secukinumab, and others for managing HS inflammation. The choice of biologic is tailored to the patient’s needs and the severity of their condition, often requiring higher or more frequent dosing for optimal results. Dosing options for a few biologics are listed below. Dr. Okoye tends to start with Adalimumab given that this biologic is FDA-approved for HS and therefore easier to obtain for patients.
-
- Adalimumab has three alternative dosing options:
- 40mg once weekly
- 80mg every other week
- 80mg weekly (off-label use) for patients with severe disease
- Adalimumab has three alternative dosing options:
-
- Infliximab dosing:
- infusion 10mg/kg (high dose) every 4-6 weeks
- Infliximab dosing:
-
- Ustekinumab dosing:
- 90mg every 4-8 weeks
- Ustekinumab dosing:
Addressing Inflammation with Steroids
Steroid injections at higher concentrations are utilized as a rapid intervention for patients with severe pain or discomfort. Dr. Okoye will use 40mg/cc of triamcinolone acetonide or 20mg/cc (diluted with lidocaine) injected around the inflamed lesion. This leads to significant improvement in 24-48 hours.
Oral prednisone is strategically employed for HS patients in three ways:
-
- As “Rescue” during severe flares
- Bridge to biologics or surgery
- High dose 80mg daily for 3 days THEN taper by 10mg every 2-3 days (Total time on prednisone is 2-3 weeks)
- As “Brakes” to preemptively mitigate flares
- Can keep patients out of the ED
- 20-40mg daily for 3 days
- As “maintenance” treatment for severe HS in conjunction with other therapies
- For patients who have maximized other therapies, are unable to tolerate other therapies, or have a steroid-responsive comorbidity (e.g., Keratitis, PG)
- Prednisone 5-10mg daily
- Make sure to monitor calcium/vitamin D, blood sugar, and blood pressure and to obtain DEXA scans with long-term use of steroids
- As “Rescue” during severe flares
Dr. Okoye’s approach to treating Hidradenitis Suppurativa encompasses a multifaceted strategy that addresses the underlying pathology, lifestyle factors, hormonal influences, and inflammation. By combining these various approaches, patients with HS can receive comprehensive care and hope for a better quality of life. It is important to remember that HS is a complex condition, and individualized treatment plans should be tailored to each patient’s unique needs and responses. Moreover, continued research is essential to further our understanding of this condition and improve treatment outcomes.
References
-
- Saunte, D. M. L., & Jemec, G. B. E. (2017). Hidradenitis Suppurativa: Advances in Diagnosis and Treatment. JAMA, 318(20), 2019–2032. https://doi.org/10.1001/jama.2017.16691
- Kranendonk, A., van der Reijden, W., van Winkelhoff, A., & van der Weijden, G. (2010). The bactericidal effect of a Genius Nd:YAG laser. International journal of dental hygiene, 8(1), 63–67. https://doi.org/10.1111/j.1601-5037.2009.00375.x
- Jennings, L., Nestor, L., Molloy, O., Hughes, R., Moriarty, B., & Kirby, B. (2017). The treatment of hidradenitis suppurativa with the glucagon-like peptide-1 agonist liraglutide. The British journal of dermatology, 177(3), 858–859. https://doi.org/10.1111/bjd.15233
This information was presented by Dr. Ginette A. Okoye during the 2023 Skin of Color Update conference. The above highlights from her lecture were written and compiled by Dr. Sarah Millan.
Did you enjoy this article? You can find more on Medical Dermatology here.

