INTRODUCTION
Benign Familial Pemphigus, or Hailey-Hailey Disease (HHD), affects intertriginous areas of the skin causing epidermal blistering and vesicles that coalesce into weeping and crusting plaques.¹
The loss-of-function mutation of the ATP2C1 gene causes a disruption in calcium homeostasis of keratinocytes. The resulting dysfunction in desmosomes and cell-cell adhesion causes acantholysis.¹ Lesions are often found in areas such as the groin, inguinal folds, axilla, and intramammary folds, and there is an increased risk of squamous cell carcinoma arising within areas of HHD.¹ Symptoms are often remitting and relapsing with eruptions exacerbated by heat, sweat, and friction.
Only 8 cases in the literature have been published demonstrating the utility of the 595 nm pulsed-dye laser (PDL) to treat recalcitrant HHD.2,3 JDD authors Ana Duarte-Summers MS, Leena Ramani MD, and Sherry Yang MD present an additional case of recalcitrant HHD successfully treated with PDL.
CASE REPORT
A 62-year-old Asian female presented with a painful rash in the groin, inner thighs, and buttocks for 20 years. The rash flared multiple times a year and was exacerbated by heat, sweating, and walking. Physical exam revealed hyperpigmented inactive patches in bilateral axillae as well as well-defined erythematous macerated plaques with a peripheral collarette of scale on the bilateral inner thighs, vulva, perineum, and perianal skin. A 4 mm punch biopsy from the right upper inner thigh revealed an acantholytic dyskeratotic dermatosis consistent with HHD.
Over the next 6 years, she was treated with various topical regimens, including topical steroids, topical antifungals, tetracycline antibiotics, and tacrolimus ointment. While her axillary disease remained well-controlled, she required multiple courses of minocycline 100 mg bid, higher potency topical steroids (clobetasol and betamethasone), and intralesional triamcinolone injections for persistent lesions in her groin.
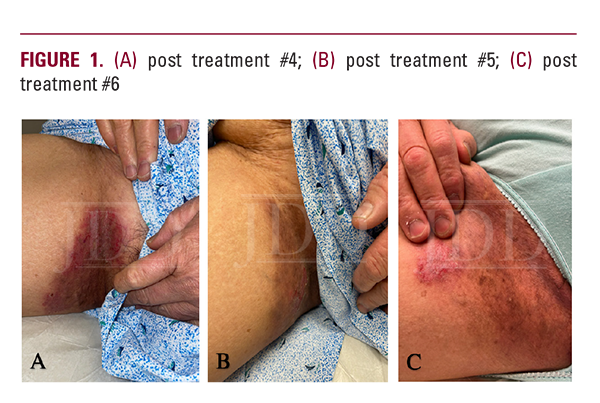
In August 2022, PDL was started to treat recalcitrant plaques on both inner thighs and vulva. Each treatment was completed using the Candela Vbeam Perfecta 595 nm laser at a setting of fluence 7 J/cm2, pulse duration of 10 msec, and spot size of 10 mm. A single pass with 10-20% overlap was performed over the entirety of each active plaque. There was marked decrease in erythema, maceration, itching, and pain after just one session. Relapse occurred after approximately 4 weeks, prompting retreatment. At the time of publication, she had received a total of 6 PDL sessions at 6-8 week intervals with significant improvement but not complete remission. Topical maintenance with triamcinolone 0.1% ointment mixed with nystatin cream Monday, Wednesday, and Friday alternating with tacrolimus 0.1% ointment was continued throughout the treatment period. There were no other changes in therapy or laser-related complications.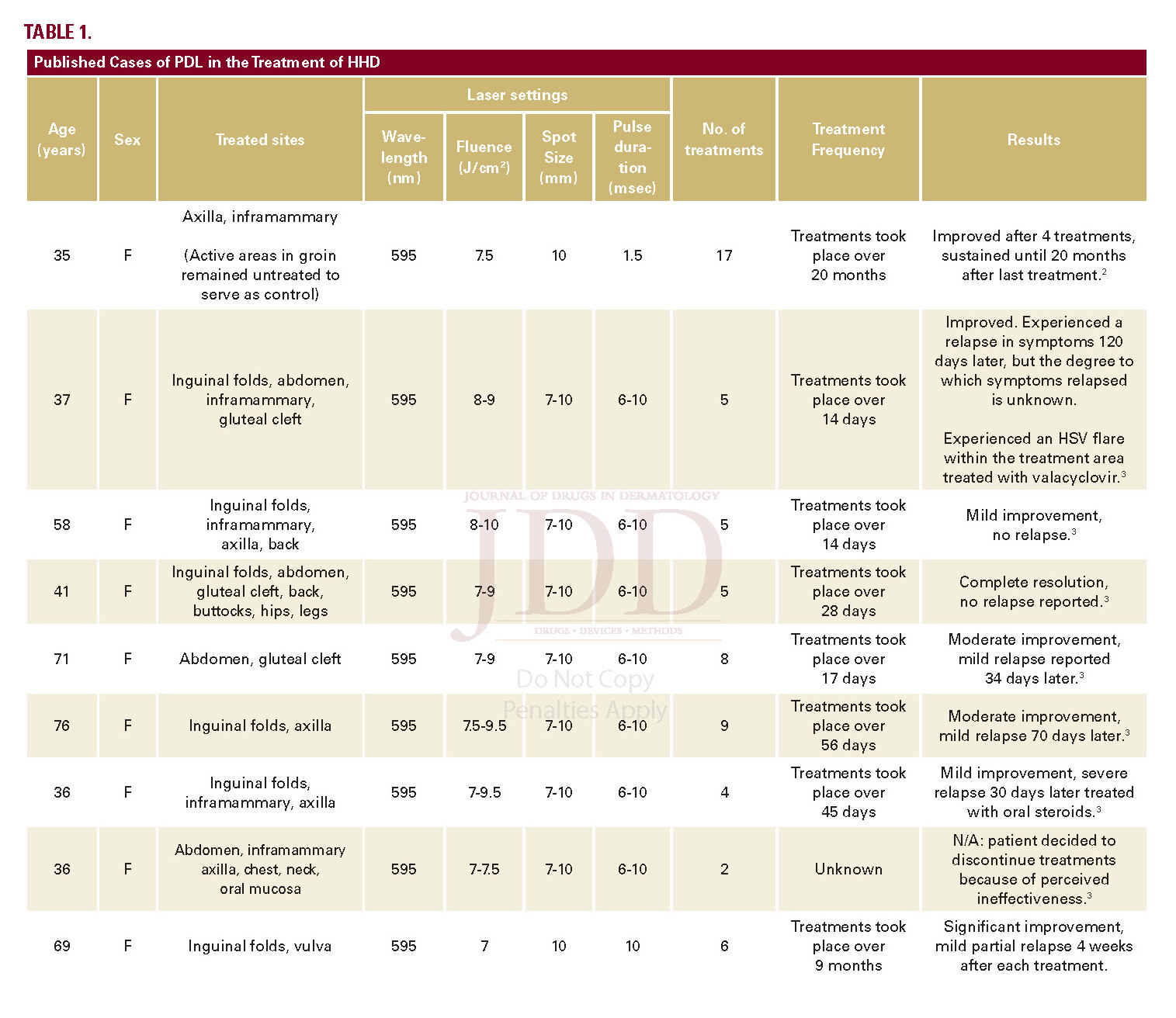
DISCUSSION
PDL was designed for the treatment of cutaneous vascular disorders including port-wine stains, hemangiomas, and telangiectasias. PDL has since been used in various non-vascular dermatologic conditions including, for example, dermatosis papulosa nigra and lentigines, similarly taking advantage of melanin’s ability to absorb the yellow light emitted by the PDL.4
While studying the use of PDL in the treatment of inflammatory acne, Seaton et al propose that short pulse duration non-ablative PDL causes hemoglobin to absorb the emitted light, causing injury to the dermis that induces wound healing without vessel rupture, increasing collagen production and inducing dermal remodeling. The authors posit that TGF-Beta is upregulated by PDL lasers and TGF-Beta in turn may upregulate collagen synthesis.5
More recent reports detail the use of PDL in blistering disorders. A 2022 case report by Garza-Mayers et al describes the successful use of PDL in the treatment of two patients with dominant dystrophic epidermolysis bullosa (DDEB), and epidermolysis bullosa pruriginosa, positing that PDL may decrease blister formation because of the stimulation of collagen remodeling.6
The first case of HHD treated with PDL was described in 2006 by Fisher et al, in which a 35-year-old female was treated with a 7.5 J/cm2 fluence for 17 treatments and experienced full remission with no lasting side effects at least 20 months after the last treatment.² An additional 7 cases of HHD treated with PDL were described in 2015, each to varying degrees of success: two experienced full remission, two experienced mild relapses, one experienced severe relapse, one discontinued treatment, and the long-term outcomes of the last patient are unknown.³ The authors’ patient represents the 9th known case in the literature, resulting in an overall response rate of 66% amongst published cases. While she has demonstrated substantial interval improvement with each treatment, the long-term efficacy remains to be determined.
JDD authors propose that PDL is a reasonable second-line treatment option for patients with recalcitrant HHD who have either failed standard topical therapy or experienced adverse side effects. Even a few weeks of transient symptomatic relief may be worthwhile to patients when other options are lacking. PDL also has several practical advantages over ablative resurfacing lasers when used for HHD, including ease of operation, minimal procedure-related discomfort not requiring the use of topical or tumescent anesthesia, low risk of procedure-related complications, and little to no recovery. Most treatments can be completed within the timeframe of a 15-minute office visit. Further research and randomized controlled trials are needed to investigate optimal treatment settings and intervals for this rare disease.
REFERENCES
-
- Arora H, Bray FN, Cervantes J, et al. Management of familial benign chronic pemphigus. Clin Cosmet Investig Dermatol. 2016;9:281-290. Published 2016 Sept 14. doi: 10.2147/CCID.S89483.
- Fisher GH, Geronemus RG.. Improvement of Familial Benign Pemphigus after Treatment with Pulsed-Dye Laser: A Case Report. Dermatol Surg. 2016; 32(7):p 966-968.
- Hunt KM, Jensen JD, Walsh SB, et al. Successful treatment of refractory Hailey-Hailey disease with a 595-nm pulsed dye laser: a series of 7 cases. J Am Acad Dermatol. 2015;72(4):735-737. doi:10.1016/j.jaad.2014.12.023.
- Liu A, Moy RL, Ross EV, et al. Pulsed dye laser and pulsed dye laser-mediated photodynamic therapy in the treatment of dermatologic disorders. Dermatol Surg. 2012;38(3):351-366. doi:10.1111/j.1524-4725.2011.02293.x.
- Seaton ED, Mouser PE, Charakida A, et al. Investigation of the mechanism of action of nonablative pulsed-dye laser therapy in photorejuvenation and inflammatory acne vulgaris [published correction appears in Br J Dermatol. 2007 Feb;156(2):409. Seldon, P E [corrected to Seldon, P M]]. Br J Dermatol. 2006;155(4):748-755. doi:10.1111/j.1365-2133.2006.07429.x.
- Garza-Mayers AC, Su KA, Wiss K. Improved erythema and decreased blister formation in dominant dystrophic epidermolysis bullosa following treatment with pulsed dye laser. Pediatr Dermatol. 2022;39(6):1005-1006. doi:10.1111/pde.15126.
SOURCE
Duarte-Summers, A., Ramani, L., & Yang, S. (2023). Utility of Pulsed-Dye Laser in the Treatment of Recalcitrant Hailey-Hailey Disease. Journal of Drugs in Dermatology: JDD, 22(11), e1-e3.
Published with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this JDD case report? You can find more here.