Vitiligo is an autoimmune skin disease that affects >3 million individuals in the US and around 74 million worldwide. In addition to physical symptoms such as itch, it can be particularly cosmetically concerning and psychologically distressing. It mainly affects young individuals, where it is estimated that 50% of cases have onset before the age of 20. Importantly, it is associated with other autoimmune disorders like type 1 diabetes, lupus, Hashimoto thyroiditis, pernicious anemia, and Addison’s disease.
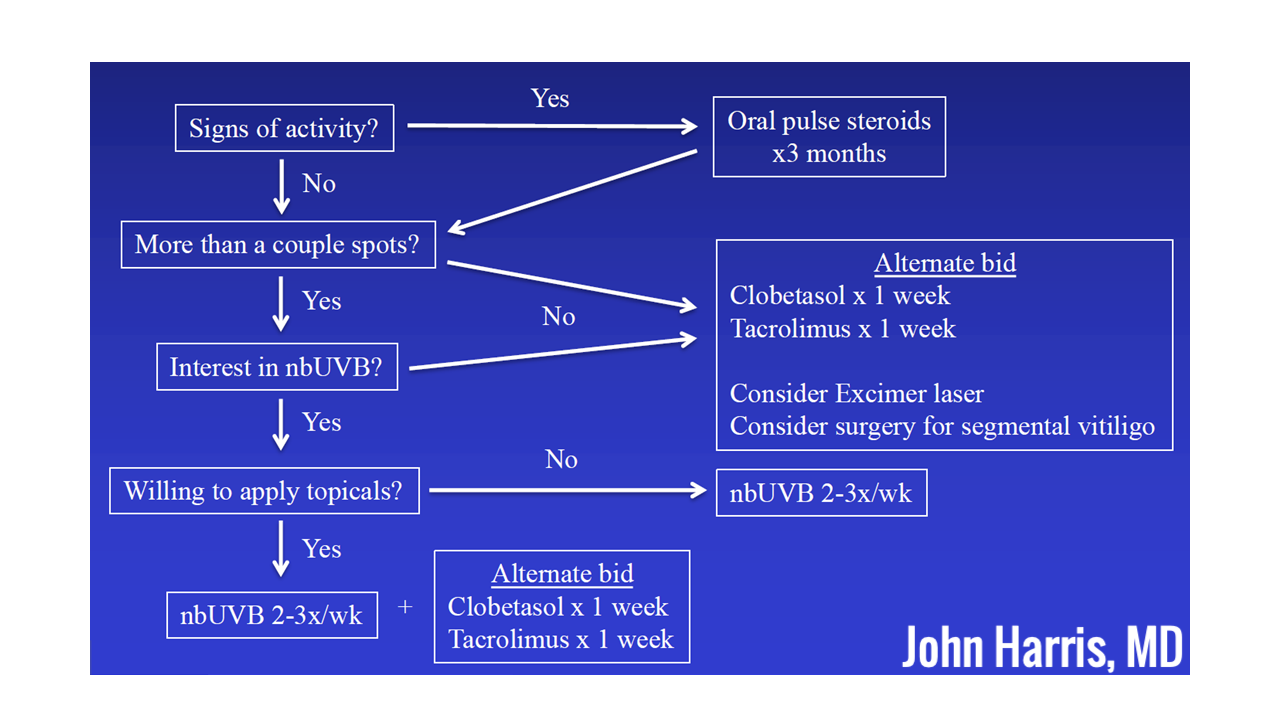
At the 2020 ODAC Dermatology, Aesthetic and Surgical Conference, Dr. John Harris, Vice-Chair of Dermatology and Director of the Vitiligo Clinic and Research Center at UMass Medical School in Worcester, Massachusetts, presented on current and emerging treatments of vitiligo, as discussed below. Briefly, the associated image highlights the treatment algorithm which relies on signs of activity, number of lesions, and patient’s interest in phototherapy and topicals:
Phototherapy
The mainstay of phototherapy is NB-UVB. The protocol can be accessed on www.umassmed.edu/vitiligo. It is crucial to ascertain that the protocol is aggressive enough to induce mild erythema lasting < 24 hours. As a rule of thumb, any lesion which includes pigmented hairs should respond, and if it does not respond after months of therapy, then the possibility of a not-aggressive-enough regimen should be entertained.
Importantly, Dr. Harris highlights the cost-effectiveness of home phototherapy in addition to its convenience for most patients: The cost of in-office therapy reaches the cost of an at home-unit after 3 months of treatment, with comparable efficacies.
Depigmentation: monobenzyl ether of hydroquinone
Surprisingly, this is the only FDA-approved treatment for vitiligo! It is administered 1-2x/day for up to 2 years. It induces remote depigmentation and patients are almost always very satisfied. Nevertheless, 20% experience treatment-limiting contact dermatitis.
Can targeted immunotherapy improve treatment responses?
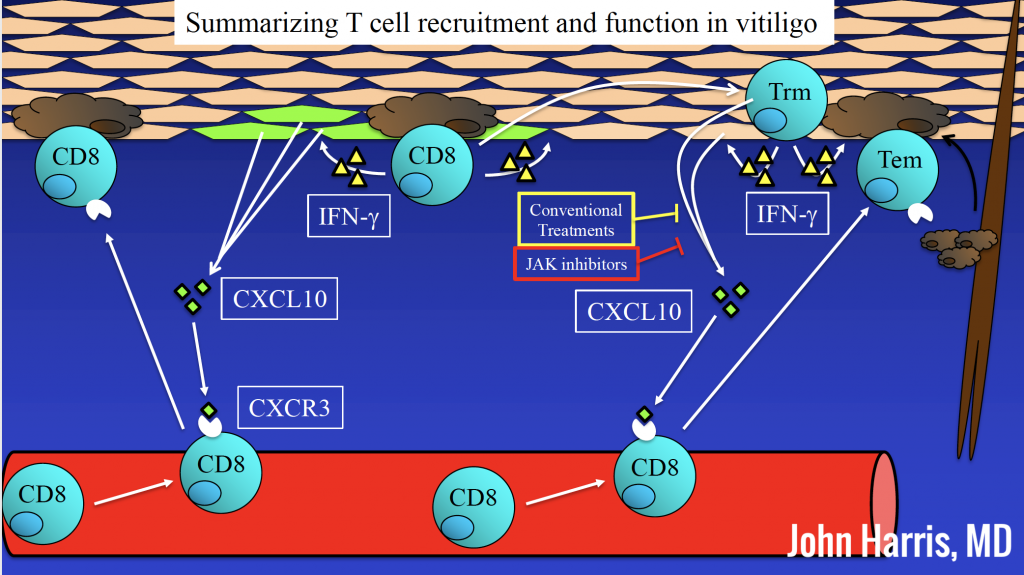
Next, Dr. Harris presented his work integrating basic, translational, and clinical research. Quantifying gene expression in vitiligo and normal skin from both humans and mice shows that vitiligo lesions display a Th1 signature profile. Expectedly, melanocyte-expressed genes were downregulated. This Th1 signature proposes new targets in the treatment of vitiligo, including the IFNγ signaling pathway, CXCR3, CXCL9, and CXCL10.
In a patient with vitiligo and alopecia areata treated with ruxolitinib, rapid skin repigmentation was observed, although this response was not durable once the patient was off treatment1. This aligns with the above and supports the notion that targeting the IFNγ pathway could be a viable option for treating vitiligo.
In a double-blind, vehicle-controlled clinical trial (NCT03099304), facial vitiligo area severity index 50 (F-VASI50) was achieved in 25.8%–50.0% (across doses) of patients receiving ruxolitinib cream vs 3.1 % receiving vehicle by week 24. At week 52, among patients receiving the highest concentration of ruxolitinib cream (1.5%), 51.5% achieved F-VASI75 and 33.3% achieved F-VASI90, compared to no patients achieving either F-VASI in the vehicle group. Acne was the most common adverse event associated with ruxolitinib use.
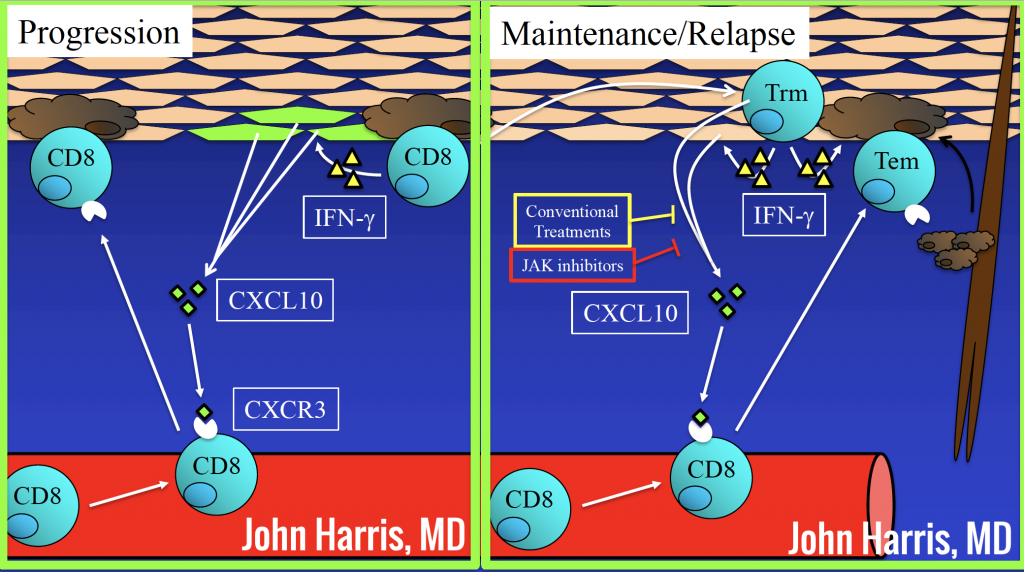
In a clinical trial using topical tacrolimus in vitiligo2, similar to the scenario seen with ruxolitinib above, relapse was seen in 40% of patients within the 1st year of stopping treatment. This calls for more durable immunological interventions for the treatment of vitiligo, as discussed below.
Can we selectively deplete resident memory T cells (Trm) to treat vitiligo?
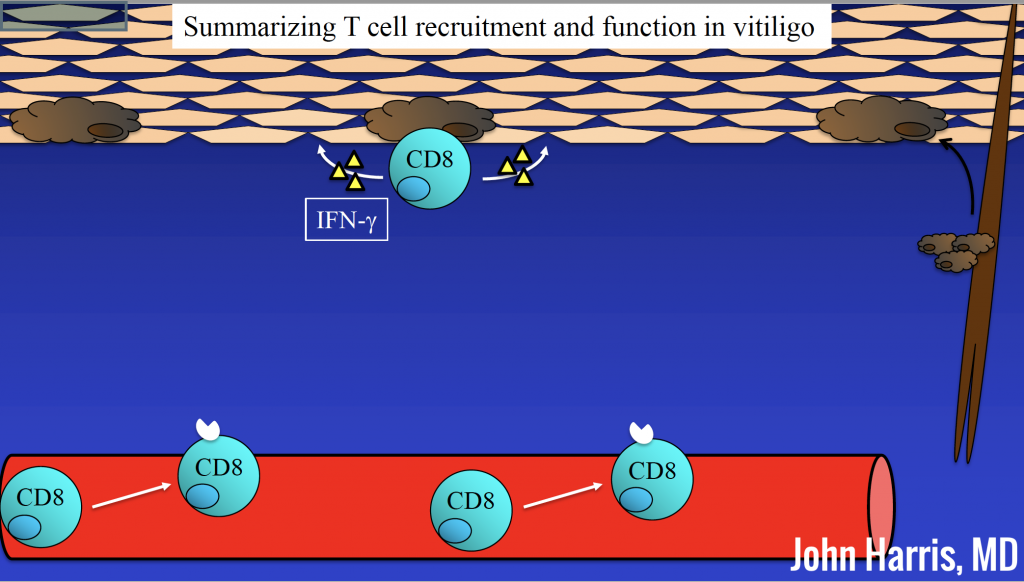
The associated figures demonstrate T cell recruitment and function in vitiligo. Since Trm cells require IL15 to survive, this provides a reasonable target to deplete those cells. In a proof of principle experiment, mice receiving anti-IL15R antibodies displayed depletion of Trm cells and repigmentation of vitiligo3. Targeting Trm cells could promise a more durable response in vitiligo by inhibiting the generation of effector T cells which ultimately attack melanocytes.
References
- Harris JE, Rashighi M, Nguyen N, et al. Rapid skin repigmentation on oral ruxolitinib in a patient with coexistent vitiligo and alopecia areata (AA). Journal of the American Academy of Dermatology. 2016;74(2):370-371.
- Cavalie M, Ezzedine K, Fontas E, et al. Maintenance therapy of adult vitiligo with 0.1% tacrolimus ointment: a randomized, double blind, placebo-controlled study. The Journal of investigative dermatology. 2015;135(4):970-974.
- Richmond JM, Strassner JP, Zapata L, Jr., et al. Antibody blockade of IL-15 signaling has the potential to durably reverse vitiligo. Science translational medicine. 2018;10(450).
Did you enjoy this article? Find more on Medical Dermatology here.

