At the 2023 ODAC Dermatology, Aesthetic & Surgical Conference, we were lucky to learn about the management of vitiligo from the renowned researcher and clinician, Dr. John Harris, Professor and Chair of Dermatology at the University of Massachusetts. When a new patient with vitiligo presents to my clinic, I always pull out my phone to consult Dr. Harris’ treatment protocol – I am sure I am not alone in this practice! In this article, we will review Dr. Harris’ treatment algorithm, clinical pearls for tough cases, and new research in the field of depigmentation. These topics are critical to care for patients with vitiligo, a disease that can be widespread and psychologically devastating.
Vitiligo statistics
Vitiligo has a prevalence of 1.4%. It often starts early, with half of patients developing disease before age 20, and persists for a patient’s lifetime. Vitiligo can be also associated with other autoimmune diseases, including type 1 diabetes, Hashimoto thyroiditis, and pernicious anemia.
Presentation
Vitiligo can affect any area of the body and can be extremely widespread. Vitiligo can also progress to involve hair follicles (called poliosis or leukotrichia), at which point, the possibility of re-pigmentation is low. When assessing patients, there are two important presentations to recognize:
-
- Segmental vitiligo – patients have involvement of one part of the body that does not cross the midline. This subtype tends to involve the hair follicles early, so it is very difficult to treat.
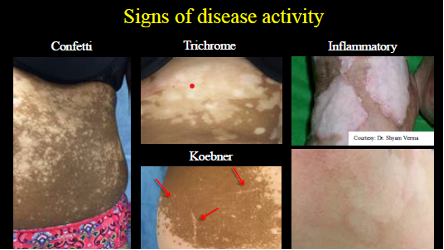
- Vitiligo with signs of rapid progression – active and progressive vitiligo requires more aggressive treatment. Signs of active disease include (Figure 1):
- Tiny macules of “confetti” depigmentation.
- Trichrome vitiligo, with areas of normal skin, hypopigmented skin, and depigmented skin.
- Presence of koebnerization, with linear macules of depigmentation.
- Inflammatory disease, where you see a subtle erythematous rim around depigmented skin that can be scaly or pruritic.
Vitiligo work up
The diagnosis of vitiligo is made clinically, with the help of a wood’s lamp, which will only enhance depigmented skin. A review of systems (ROS) is critical to screen for associated autoimmune diseases or syndromes, such as Vogt-Koyanagi-Harada, where you can have meningitis, uveitis, or tinnitus. If you have concerns for thyroid disease based on the ROS, you should check a TSH. Dr. Harris admits that this is a debated point – given the prevalence of thyroid disease increases to 20% with vitiligo, many dermatologists check TSH in all patients.
Differential Diagnosis of Vitiligo
Given vitiligo is a clinical diagnosis, it is critical to consider and rule out other disorders of hypopigmentation and depigmentation, including nevus depigmentosus, piebaldism, Waardenburg syndrome, albinism, idiopathic guttae hypomelanosis, sarcoidosis, and lichen sclerosus.
Treatment
Before determining a treatment approach, expectations must be reviewed. Repigmentation comes from follicles, so if hair follicles are already depigmented or the disease is only present on glabrous skin without follicles, repigmentation is not possible. On glabrous skin, you can get “marginal repigmentation” from the edge, but this will only be 1 to 2 millimeters in total.
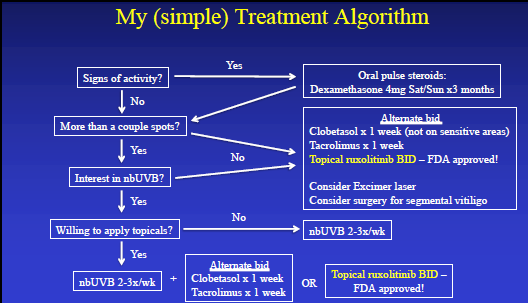
Dr. Harris’ treatment algorithm (Figure 2) begins with whether you see signs of active disease on physical exam (Figure 1); if you do, you should start oral pulsed dose steroids with dexamethasone 4 milligrams on Saturday and Sunday for 3 months. Then, you will consider the amount of disease. If the disease is limited, you can use topical treatment alone, alternating clobetasol for 1 week with tacrolimus for 1 week on the body or tacrolimus alone on the face. If you are able to obtain approval of topical ruxolitinib cream, you can use this alone as it tends to work faster and better than the alternative regimen. With limited disease, in addition to topical treatment, you can also consider excimer laser or surgery, which we will discuss later. For more extensive disease, narrowband UVB (nbUVB) therapy 2 to 3 times per week should be your go to treatment. If patients are willing, you can ideally combine nbUVB with one of the above topical regimens.
If patients still have follicular pigment present on non-glabrous skin, this algorithm should work for most patients. For unusual patients who do not respond, you can consider oral tofacitinib, or for those interested in vacation in addition to treatment, you can also send patients to bathe in the Dead Sea Spa in Jordan or Israel! Dr. Harris thinks this treatment works due to the combination of sea salt, elevation of the area (below sea level), and sun exposure given dead sea salts alone are not efficacious.
As for the surgical treatment mentioned, a specialized surgical procedure called melanocyte keratinocyte transplant can also be done. Essentially, a thin skin graft is taken from the patient’s thigh or buttocks. The sample is disassociated with trypsin, re-suspended, and then transplanted to the depigmented area that has been prepared with dermabrasion or laser ablation. While this procedure is not widely available, Dr. Harris and colleagues are helping to test a kit that could make this technique accessible for all dermatologists.
Depigmentation As “Treatment”
Prior to ruxolitinib cream, the only FDA-approved treatment of vitiligo was monobenzyl ether of hydroquinone, which is a cream used once or twice a day for 1 to 2 years that results in complete depigmentation. This treatment will cause remote depigmentation as well, so application to the hands alone can depigment the entire body. Additionally, 20% of patients develop contact dermatitis that can be treatment limiting. You should counsel patients to “consider this permanent,” per Dr. Harris. In reality, though, repigmentation is possible, for which monobenzyl ether of hydroquinone can be used again.
Future Treatment: Targeted Immunotherapy
Based on translational research by Dr. Harris, his team found that an interferon gamma signature exists in both human and mouse models, which differs from the Type 2 signal in atopic dermatitis and Type 17 signal in psoriasis. JAK inhibitors (JAKi) inhibit this interferon gamma signal and thus can treat vitiligo. We already have topical ruxolitinib cream, as discussed above, but clinical trials are also being done on oral therapies. For ruxolitinib cream, the clinical trial demonstrated that 30% patients achieved 75% improvement on the face within 6 months, with only minimal side effects of acne and application site pruritus1. In another trial, an oral JAKi, ritlecitinib, only resulted in 75% facial improvement in 12% of patients.2 However, the trial only included patients with active disease, which is a high bar. Many side effects were also reported in both the treatment and placebo groups, so more research is needed to understand the efficacy and risks of ritlecitinib.
In conclusion, while there are finally new treatments for vitiligo other than monobenzyl ether of hydroquinone, nbUVB or the excimer laser should still be the main treatments in your repertoire for vitiligo along with topical regimens. It is critical to recognize signs of actively spreading vitiligo, which requires oral pulse dosed steroids, in addition to other maintenance treatments.
Figures
References
-
- Rosmarin D, Passeron T, Pandya AG, et al. Two Phase 3, Randomized, Controlled Trials of Ruxolitinib Cream for Vitiligo. N Engl J Med. 2022;387(16):1445-1455. doi:10.1056/NEJMoa2118828
- Ezzedine K, Peeva E, Yamaguchi Y, et al. Efficacy and safety of oral ritlecitinib for the treatment of active nonsegmental vitiligo: A randomized phase 2b clinical trial. J Am Acad Dermatol. 2023;88(2):395-403. doi:10.1016/j.jaad.2022.11.005
This information was presented by Dr. John Harris at the 2023 ODAC Dermatology, Aesthetic and Surgical Conference held January 12-15, 2023. The above highlights from his lecture were written and compiled by Dr. Emily Murphy.
Did you enjoy this post? Find more on pigmentary disorders here.

