Fluconazole is a synthetic triazole with a broader antifungal spectrum than the imidazole class. Resistance to first-pass metabolism and consistent oral absorption are advantages over agents like ketoconazole in the antifungal armamentarium, particularly in the context of the United States Food and Drug Administration’s reinforced warning against oral ketoconazole for skin and nail infections, due to liver and adrenal toxicity and drug interactions. We continue our series, Therapeutic Cheat Sheet, with a closer look at fluconazole, which is FDA-approved for candidiasis of various mucosal sites, systemic Candida infections, cryptococcal meningitis, and prophylaxis against candidiasis in patients undergoing bone marrow transplant. Fluconazole is also used off-label for dermatologic conditions ranging from dermatophytosis to cutaneous manifestations of endemic mycoses.
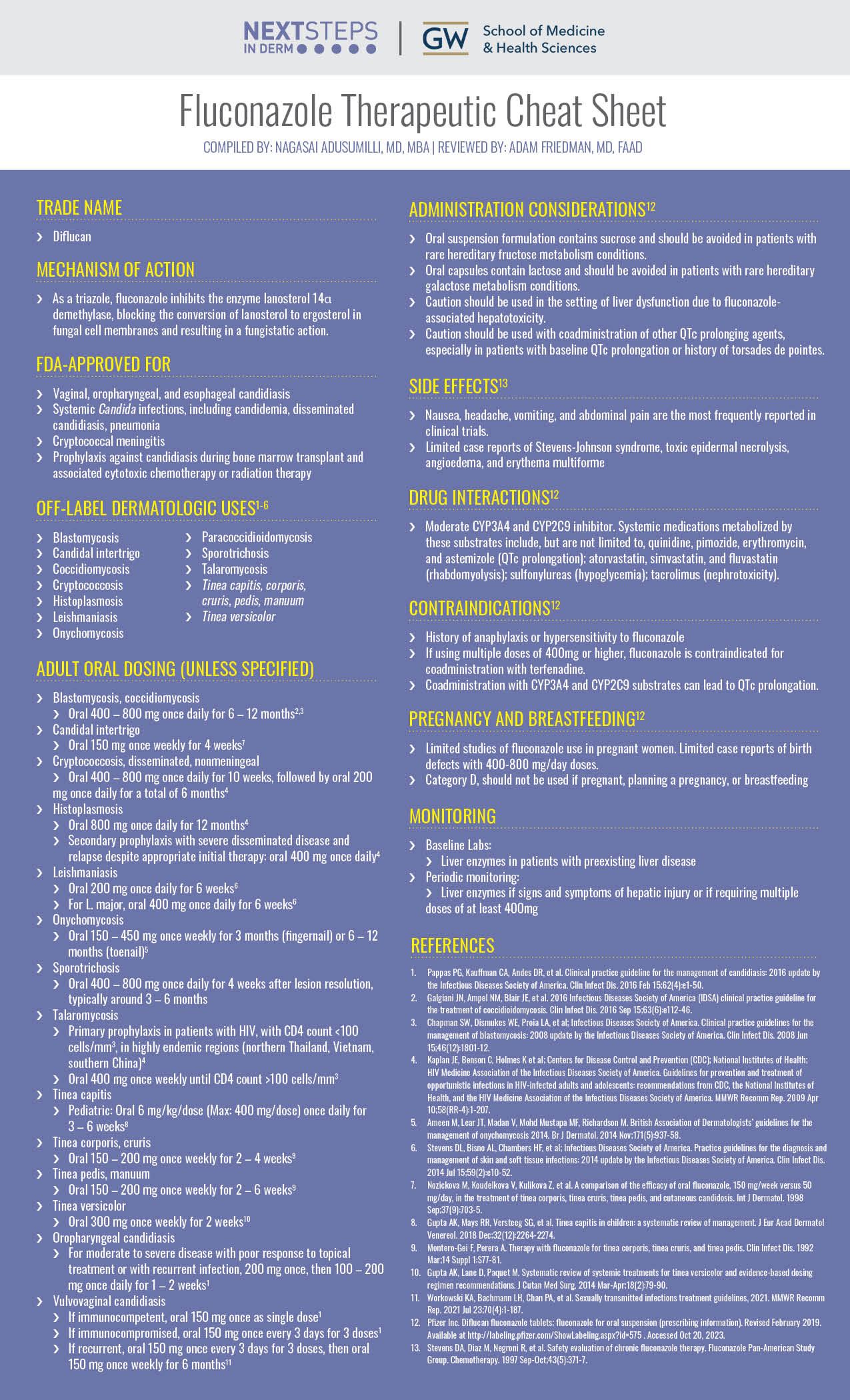
Fluconazole Therapeutic Cheat Sheet
Compiled by: Nagasai Adusumilli, MD, MBA | Reviewed by: Adam Friedman, MD, FAAD
TRADE NAME
-
- Diflucan
MECHANISM OF ACTION
-
- As a triazole, fluconazole inhibits the enzyme lanosterol 14α demethylase, blocking the conversion of lanosterol to ergosterol in fungal cell membranes and resulting in a fungistatic action.
FDA-APPROVED FOR
-
- Vaginal, oropharyngeal, and esophageal candidiasis
- Systemic Candida infections, including candidemia, disseminated candidiasis, pneumonia
- Cryptococcal meningitis
- Prophylaxis against candidiasis during bone marrow transplant and associated cytotoxic chemotherapy or radiation therapy
OFF-LABEL DERMATOLOGIC USES1-6
-
- Blastomycosis
- Candidal intertrigo
- Coccidiomycosis
- Cryptococcosis
- Histoplasmosis
- Leishmaniasis
- Onychomycosis
- Paracoccidioidomycosis
- Sporotrichosis
- Talaromycosis
- Tinea capitis, corporis, cruris, pedis, manuum
- Tinea versicolor
ADULT ORAL DOSING (UNLESS SPECIFIED)
-
- Blastomycosis, coccidiomycosis
- Oral 400 – 800 mg once daily for 6 – 12 months2,3
- Candidal intertrigo
- Oral 150 mg once weekly for 4 weeks7
- Cryptococcosis, disseminated, nonmeningeal
- Oral 400 – 800 mg once daily for 10 weeks, followed by oral 200 mg once daily for a total of 6 months4
- Histoplasmosis
- Oral 800 mg once daily for 12 months4
- Secondary prophylaxis with severe disseminated disease and relapse despite appropriate initial therapy: oral 400 mg once daily4
- Leishmaniasis
- Oral 200 mg once daily for 6 weeks6
- For major, oral 400 mg once daily for 6 weeks6
- Onychomycosis
- Oral 150 – 450 mg once weekly for 3 months (fingernail) or 6 – 12 months (toenail)5
- Sporotrichosis
- Oral 400 – 800 mg once daily for 4 weeks after lesion resolution, typically around 3 – 6 months
- Talaromycosis
- Primary prophylaxis in patients with HIV, with CD4 count <100 cells/mm3, in highly endemic regions (northern Thailand, Vietnam, southern China)4
- Oral 400 mg once weekly until CD4 count >100 cells/mm3
- Tinea capitis
- Pediatric: Oral 6 mg/kg/dose (Max: 400 mg/dose) once daily for 3 – 6 weeks8
- Tinea corporis, cruris
- Oral 150 – 200 mg once weekly for 2 – 4 weeks9
- Tinea pedis, manuum
- Oral 150 – 200 mg once weekly for 2 – 6 weeks9
- Tinea versicolor
- Oral 300 mg once weekly for 2 weeks10
- Oropharyngeal candidiasis
- For moderate to severe disease with poor response to topical treatment or with recurrent infection, 200 mg once, then 100 – 200 mg once daily for 1 – 2 weeks1
- Vulvovaginal candidiasis
- If immunocompetent, oral 150 mg once as single dose1
- If immunocompromised, oral 150 mg once every 3 days for 3 doses1
- If recurrent, oral 150 mg once every 3 days for 3 doses, then oral 150 mg once weekly for 6 months11
- Blastomycosis, coccidiomycosis
ADMINISTRATION CONSIDERATIONS12
-
- Oral suspension formulation contains sucrose and should be avoided in patients with rare hereditary fructose metabolism conditions.
- Oral capsules contain lactose and should be avoided in patients with rare hereditary galactose metabolism conditions.
- Caution should be used in the setting of liver dysfunction due to fluconazole-associated hepatotoxicity.
- Caution should be used with coadministration of other QTc prolonging agents, especially in patients with baseline QTc prolongation or history of torsades de pointes.
SIDE EFFECTS13
-
- Nausea, headache, vomiting, and abdominal pain are the most frequently reported in clinical trials.
- Limited case reports of Stevens-Johnson syndrome, toxic epidermal necrolysis, angioedema, and erythema multiforme
DRUG INTERACTIONS12
-
- Moderate CYP3A4 and CYP2C9 inhibitor. Systemic medications metabolized by these substrates include, but are not limited to, quinidine, pimozide, erythromycin, and astemizole (QTc prolongation); atorvastatin, simvastatin, and fluvastatin (rhabdomyolysis); sulfonylureas (hypoglycemia); tacrolimus (nephrotoxicity).
CONTRAINDICATIONS12
-
- History of anaphylaxis or hypersensitivity to fluconazole
- If using multiple doses of 400mg or higher, fluconazole is contraindicated for coadministration with terfenadine.
- Coadministration with CYP3A4 and CYP2C9 substrates can lead to QTc prolongation.
PREGNANCY AND BREASTFEEDING12
-
- Limited studies of fluconazole use in pregnant women. Limited case reports of birth defects with 400-800 mg/day doses.
- Category D, should not be used if pregnant, planning a pregnancy, or breastfeeding
MONITORING
-
- Baseline Labs:
- Liver enzymes in patients with preexisting liver disease
- Periodic monitoring:
- Liver enzymes if signs and symptoms of hepatic injury or if requiring multiple doses of at least 400mg
- Baseline Labs:
FURTHER READING
If you would like to learn more about fluconazole, check out the following articles in the Journal of Drugs in Dermatology:
Combination of Fluconazole and Alpha-tocopherol in the Treatment of Yellow Nail Syndrome
Baran and L. Thomas
Abstract
Yellow nail syndrome (YNS) is an uncommon disorder that is characterized by the slow nail growth, marked thickening, and yellow to yellow-green discoloration of the fingernails or toenails. Although the etiology of YNS is unknown, a diagnosis is indicated by the concurrent presentation of the nail changes, with lymphedema and respiratory manifestations. Although lymphedema and respiratory manifestations are sometimes manageable with regimens of medical and surgical treatments, YNS treatment options are limited and often unsuccessful. For the patient, YNS can also be cosmetically unacceptable and concealment with nail polish may not always be possible. However, it is now widely accepted that the azole class of antifungals can stimulate linear nail growth. In addition, vitamin E has also been reported in the treatment of YNS with positive results. Herein, the authors report on a promising combination treatment of oral fluconazole pulse therapy and oral alpha-tocopherol (vitamin E) in 13 patients with YNS with clinical successes observed in 2 individuals and clinical cures observed in 11 subjects.
J Drugs Dermatol. 2009;8(3):276.
Fluconazole-associated Stevens-Johnson Syndrome
Thiyanaratnam, P. Cohen, and S. Powell
Abstract
Fluconazole uncommonly causes Stevens-Johnson syndrome. A young Indian man who developed this adverse effect after his second dose of fluconazole is described. The characteristics of previously reported individuals with fluconazole-associated Stevens-Johnson syndrome and toxic epidermal necrolysis are also summarized: three out of five of the patients were immunocompromised, five out of five were hospitalized, and all had complete resolution of this drug-induced condition.
J Drugs Dermatol. 2010;9(10):1272.
REFERENCES
-
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016 Feb 15;62(4):e1-50.
- Galgiani JN, Ampel NM, Blair JE, et al. 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016 Sep 15;63(6):e112-46.
- Chapman SW, Dismukes WE, Proia LA, et al; Infectious Diseases Society of America. Clinical practice guidelines for the management of blastomycosis: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2008 Jun 15;46(12):1801-12.
- Kaplan JE, Benson C, Holmes K et al; Centers for Disease Control and Prevention (CDC); National Institutes of Health; HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009 Apr 10;58(RR-4):1-207.
- Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists’ guidelines for the management of onychomycosis 2014. Br J Dermatol. 2014 Nov;171(5):937-58.
- Stevens DL, Bisno AL, Chambers HF, et al; Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014 Jul 15;59(2):e10-52.
- Nozickova M, Koudelkova V, Kulikova Z, et al. A comparison of the efficacy of oral fluconazole, 150 mg/week versus 50 mg/day, in the treatment of tinea corporis, tinea cruris, tinea pedis, and cutaneous candidosis. Int J Dermatol. 1998 Sep;37(9):703-5.
- Gupta AK, Mays RR, Versteeg SG, et al. Tinea capitis in children: a systematic review of management. J Eur Acad Dermatol Venereol. 2018 Dec;32(12):2264-2274.
- Montero-Gei F, Perera A. Therapy with fluconazole for tinea corporis, tinea cruris, and tinea pedis. Clin Infect Dis. 1992 Mar;14 Suppl 1:S77-81.
- Gupta AK, Lane D, Paquet M. Systematic review of systemic treatments for tinea versicolor and evidence-based dosing regimen recommendations. J Cutan Med Surg. 2014 Mar-Apr;18(2):79-90.
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.
- Pfizer Inc. Diflucan fluconazole tablets; fluconazole for oral suspension (prescribing information). Revised February 2019. Available at http://labeling.pfizer.com/ShowLabeling.aspx?id=575 . Accessed Oct 20, 2023.
- Stevens DA, Diaz M, Negroni R, et al. Safety evaluation of chronic fluconazole therapy. Fluconazole Pan-American Study Group. Chemotherapy. 1997 Sep-Oct;43(5):371-7.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.

