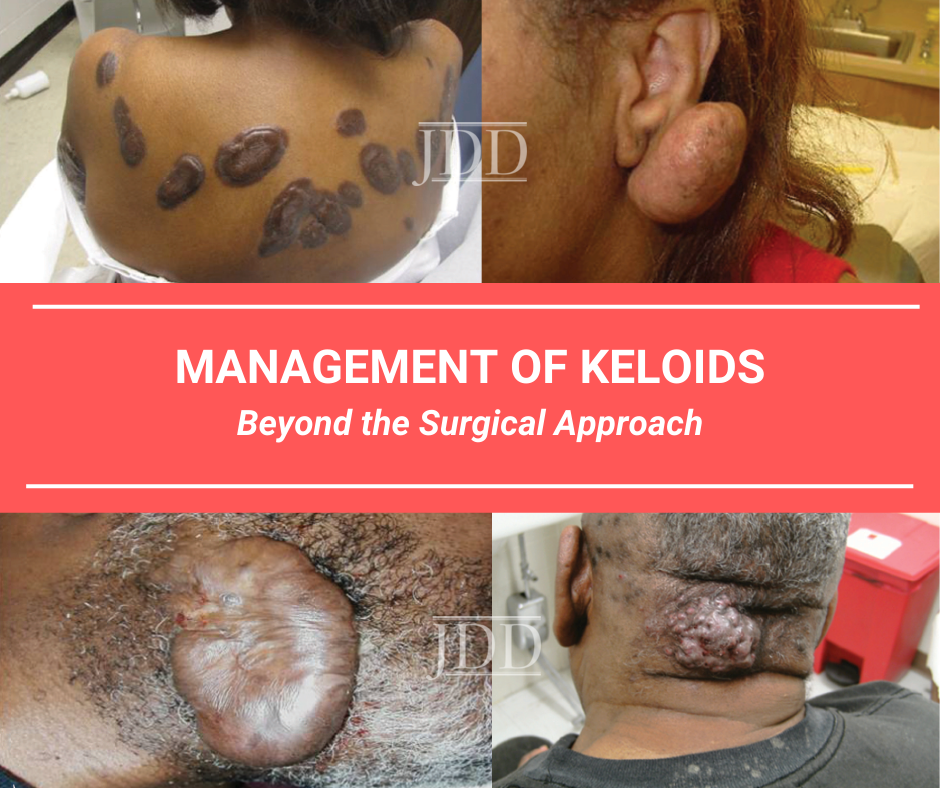
Although this may be a big assumption, I would venture to guess that training in the management of keloids has, for many residents, consisted primarily of topical and intralesional therapies—namely steroids and silicone. While steroids and silicone may be a fantastic name for a reality television show about the exciting lives of female bodybuilders, in real life it can be a pretty unimaginative way to approach the management of certain keloids, especially given all of the options that exist to treat them. Thankfully, after Dr. Maritza Perez delivered her lecture: “Management of Keloids: Beyond the Surgical Approach” at the 2019 Skin of Color Update in New York City, I feel like I am more prepared to flex on these keloids. While the management of keloids can be complicated, I hope that after reading this post, you will consider tabling that referral to plastic surgery in favor of implementing one (or several) of the many great pearls that Dr. Perez shared during her lecture. Her lecture not only broadened my knowledge of what I can be treating keloids with, it also provided essential how’s and when’s that can be used to enhance our offerings and outcomes for patients who suffer from these uncomfortable and disfiguring lesions.
This post will provide an overview of the following:
-
- Topical and intralesional therapies for keloids
- Procedural interventions for keloids—lasers and surgery
- Multi-modal approaches to keloid treatment
But first, let me share a few of the “A-ha” moments that I experienced during Dr. Perez’s lecture, in the hope that they will entice you to read on…
-
- Do you know what is lurking at your local drugstore that might help your patients treat their keloids? Well, I do thanks to Dr. Perez’s lecture. Read on to learn about this special over the counter ingredient!
- Does one of your patients have a rubbery keloid on their helical rim that you are dying to lop off? Read on for a step-by-step approach to how you can minimize the chances of it coming back to avenge itself!
- Have a long-pulsed 1064-nm Nd:YAG sitting around? Fire it up because I have the settings and the protocol that will help you remodel that keloid into oblivion!
Topical therapies for keloids
While we have likely all prescribed topical steroids to patients suffering from keloids and have steered patients in the direction of over-the-counter silicone sheeting, we need not stop here. There are yet additional options, available by prescription or over-the-counter, which patients can use in the comfort of their own homes to treat their keloids. Imiquimod 5% cream, which is frequently used to treat actinic keratoses, stubborn warts, and certain superficial non-melanoma skin cancers, can also be incorporated into a treatment regimen for keloids—keep reading for the details on how. And while imiquimod is available by prescription only, you might also suggest that patients peruse the “scar” section of the drugstore for over-the-counter topicals that contain flavonoids. These compounds have been found to inhibit SMAD protein signaling that keloid fibroblasts rely upon for extracellular matrix deposition.
Intralesional therapies for keloids
The workhorse for treating keloids intralesionally is triamcinolone acetonide (TAC), and I will discuss its place in a multi-modal approach to keloids further in this post. Workhorse though it may be, intralesional TAC is a far cry from a gentle barnyard companion. There are few among us who have not observed the hypopigmentation, atrophy, and vascular dilation that it is capable of causing. For this reason, it can (and often should) be used in combination with 5-flurouracil (for a more detailed discussion on how to treat scars with 5-FU, please find my previous post “An Update on Laser and Device Based Treatment of Scars” with Dr. Paul Friedman. Additional intralesional therapies for keloids include bleomycin, interferon -2b, and recombinant TGF-3. And if you are encountering a lot of resistance from the plunger of the syringe while trying to inject any of the aforementioned into a keloid, try a spritz of liquid nitrogen first. This can cause edema that can help facilitate entry of your solution into your target lesion.
Surgical interventions for keloids
Whether you are dealing with a firm, rubbery, pencil eraser-like keloid at the site of a former ear piercing that appears to be a perfect candidate for being sliced off at its little round base or a more extensive and geometrically complicated keloid, surgical intervention may be an approach to consider. If you are going to proceed with this route, however, know that you must commit to a pre- and post-surgery treatment regimen, as well as close follow up of the patient for at least one year after your end-point has been achieved. One sample surgical approach involves the following:
-
- Prep the keloid with intralesional TAC 40 mg/mL at Day 0, month 1, and month 2.
- At month 3, plan to excise the lesion, treating with TAC 10 mg/mL at the time of surgery.
- For extensive, severe keloids, consider sending the patient for radiation therapy at a dose of 6-8 Gy within 2 days post-op.
- At suture removal one week after surgery, initiate silicone gel sheeting to the treated area. Anticipate tapering this at 12 weeks post-op, though some patients should be advised to continue it for up to 6 months or more.
- Be advised that excision with secondary intention can often yield very good results, as this mode of healing entails a muted inflammatory proliferative phase as compared with primary intention. The choice to proceed with secondary intention healing is contingent upon a number of factors, however, such as the size and anatomic location of the keloid, as well as the patient’s ability to complete necessary wound care for a prolonged period of time.
- Starting at 2 weeks post-op (1 week after suture removal), being applying imiquimod 5% cream twice weekly for 4-6 weeks.
- At 4, 8, and 12-weeks post-op, treat the area with TAC 10 mg/mL.
Once the patient has completed the aforementioned, they should be seen monthly for the next year to ensure that the surgical site remains keloid-free. Intralesional TAC (or some of the other intralesional therapies that have been discussed) can be continued during this time on an as-needed bases to address signs of recurrence. It may be prudent to continue seeing some patients on a quarterly to biannual basis for up to several years, depending on the anatomic location of the treated area, as well as a patient’s known propensity to form keloids.
Treating keloids with lasers
While there are many lasers that can be utilized to improve the appearance of keloids (again, please circle back to my post “An Update on Laser and Device Based Treatment of Scars” with Dr. Paul Friedman, Dr. Perez specifically discussed how to employ the long-pulsed 1064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser for this indication. As is the case with surgical intervention, laser treatment of keloids can and should be combined with intralesional therapy, as the combination is more effective than either modality in isolation. Although specific settings and number of treatments will be dictated by the patient’s degree of baseline pigmentation, the texture, extent, and location of the keloid, as well as the evolution of the keloid as it is treated, a general set of treatment parameters may include the following:
-
- 13-18 J/cm2
- 3 ms pulse duration
- 500-2000 pulses per treatment at 1-6 week intervals
- 2-7 total treatments
Know that new surgical scars, relatively new keloids, or keloids that have been present for decades may be improved (albeit to varying degrees) with laser treatment. The key is to go after these lesions, when possible before they have become very disfiguring.
How do you approach the management of keloids in your own practice? What multi-modal treatments have you had particular success with? How soon after cutaneous surgery do you like to initiate treatment for keloids in a patient with a known history?
Please share your comments at the end of this post, and on Instagram @nextstepsinderm!
This information was presented by Dr. Maritza Perez at the 2019 Skin of Color Update held September 7-8 in New York City. The above highlights from her lecture were written and compiled by Dr Kimberly Huerth, Chief dermatology resident at Howard University in Washington DC.
Dr. Maritza Perez is Director of Mohs Surgery Uconn Health, Visiting Professor at Uconn Health and Clinical Professor of Dermatology at Mount Sinai Icahn School of Medicine. She also sees patients in her private practice, Advanced Aesthetics, in New Canaan, CT.
Image Credits:
All images are courtesy of the Journal of Drugs in Dermatology
https://jddonline.com/articles/dermatology/S1545961610P1249X/1/
Did you enjoy this post? Find more on Medical Derm Topics here.
Next Steps in Derm is brought to you by SanovaWorks.