Chronic idiopathic urticaria is urticaria for greater than 6 weeks without an identifiable trigger. Cases relapse in 20% of patients for more than 5 years and be difficult to manage; however, omalizumab is a recently approved option for treatment of chronic idiopathic urticaria showing beneficial outcomes.1 Omalizumab is an injectable monoclonal antibody that has been FDA approved not just for chronic idiopathic urticaria, but also for moderate to severe asthma and nasal polyps. In recent years, practitioners have been expanding the number of off-label uses of this medication to treat multiple dermatologic conditions given its efficacious mechanism of action of inhibiting IgE-mediated inflammation.2,3 In this edition of our series, Therapeutic Cheat Sheet, we will focus on omalizumab and its increased off-label use for several dermatologic conditions, including chronic idiopathic urticaria and bullous pemphigoid.
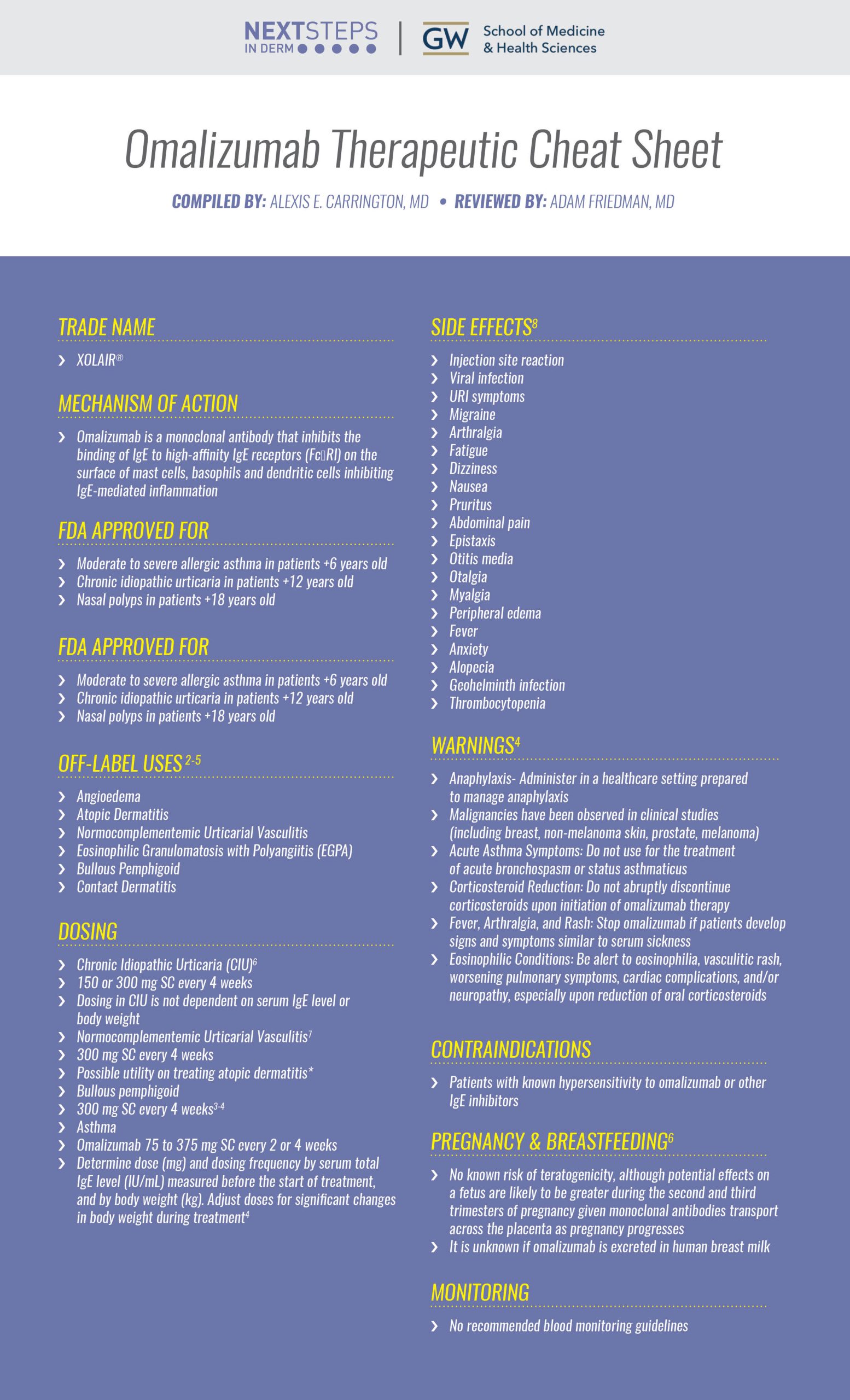
Omalizumab Therapeutic Cheat Sheet
Compiled by: Alexis E. Carrington, MD, Reviewed by: Adam Friedman, MD
OMALIZUMAB TRADE NAME
-
- XOLAIR®
MECHANISM OF ACTION
-
- Omalizumab is a monoclonal antibody that inhibits the binding of IgE to high-affinity IgE receptors (FcɛRI) on the surface of mast cells, basophils and dendritic cells inhibiting IgE-mediated inflammation
FDA APPROVED FOR
-
- Moderate to severe allergic asthma in patients +6 years old
- Chronic idiopathic urticaria in patients +12 years old
- Nasal polyps in patients +18 years old
OFF-LABEL USES OF OMALIZUMAB2-5
-
- Angioedema
- Atopic Dermatitis
- Normocomplementemic Urticarial Vasculitis
- Eosinophilic Granulomatosis with Polyangiitis (EGPA)
- Bullous Pemphigoid
- Contact Dermatitis
OMALIZUMAB DOSING
-
- Chronic Idiopathic Urticaria (CIU)6
- 150 or 300 mg SC every 4 weeks
- Dosing in CIU is not dependent on serum IgE level or body weight
- Normocomplementemic Urticarial Vasculitis7
- 300 mg SC every 4 weeks
- Possible utility on treating atopic dermatitis*
- Bullous pemphigoid
- 300 mg SC every 4 weeks3-4
- Asthma
-
- Omalizumab 75 to 375 mg SC every 2 or 4 weeks
- Determine dose (mg) and dosing frequency by serum total IgE level (IU/mL) measured before the start of treatment, and by body weight (kg). Adjust doses for significant changes in body weight during treatment4
- Omalizumab 75 to 375 mg SC every 2 or 4 weeks
-
- 150 or 300 mg SC every 4 weeks
- Chronic Idiopathic Urticaria (CIU)6
*Current literature shows administration of omalizumab to treat AD is still subject to debate, some studies showing conflicting results in effectiveness
OMALIZUMAB SIDE EFFECTS 8
-
- Injection site reaction
- Viral infection
- URI symptoms
- Migraine
- Arthralgia
- Fatigue
- Dizziness
- Nausea
- Pruritus
- Abdominal pain
- Epistaxis
- Otitis media
- Otalgia
- Myalgia
- Peripheral edema
- Fever
- Anxiety
- Alopecia
- Geohelminth infection
- Thrombocytopenia
OMALIZUMAB WARNINGS4
-
- Anaphylaxis- Administer in a healthcare setting prepared to manage anaphylaxis
- Malignancies have been observed in clinical studies (including breast, non-melanoma skin, prostate, melanoma)
- Acute Asthma Symptoms: Do not use for the treatment of acute bronchospasm or status asthmaticus
- Corticosteroid Reduction: Do not abruptly discontinue corticosteroids upon initiation of omalizumab therapy
- Fever, Arthralgia, and Rash: Stop omalizumab if patients develop signs and symptoms similar to serum sickness
- Eosinophilic Conditions: Be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy, especially upon reduction of oral corticosteroids
OMALIZUMAB CONTRAINDICATIONS
-
- Patients with known hypersensitivity to omalizumab or other IgE inhibitors
PREGNANCY & BREASTFEEDING6
-
- No known risk of teratogenicity, although potential effects on a fetus are likely to be greater during the second and third trimesters of pregnancy given monoclonal antibodies transport across the placenta as pregnancy progresses
- It is unknown if omalizumab is excreted in human breast milk
MONITORING
-
- No recommended blood monitoring guidelines
Omalizumab is being used by dermatologists more in recent years given its off- label use in treating IgE-mediated skin disease including chronic idiopathic urticaria. The list of these conditions continue to grow and include bullous pemphigoid, atopic dermatitis and angioedema. Practitioners should continue to follow newly published reports studies focusing on the off-label uses of this medication.
Further Reading
If you would like to learn more about omalizumab, check out the following two articles recently published in the Journal of Drugs in Dermatology:
Mohamed Abuzakouk MD, Omar Ghorab MB Bch BAO, Rajaie Namas MD, Marcus Maurer MD
Abstract:
Normocomplementemic urticarial vasculitis is a rare autoimmune disorder characterized by leukocytoclasia, fibrin deposits, and extravasated erythrocytes affecting multiple organ systems. Current treatment modalities, including corticosteroids and immunosuppressive agents, are of limited efficacy and an expansive side effect profile. Omalizumab has been reported to be effective in urticarial vasculitis, but its long-term effectiveness and tolerability have not yet been evaluated. We report a case of long-standing normocomplementemic urticarial vasculitis treated with omalizumab only, for almost 3 years. The patient reported a significant improvement in quality of life after the first few doses with a significant improvement in the urticaria control test. The treatment was well tolerated and no adverse events were reported after 3 years. Our patient was treated with 300 mg of omalizumab, as it was previously linked with a better improvement in quality of life. We were able to extend our patient’s treatment intervals, suggesting that this is feasible in patients treated with omalizumab who achieve a complete response. We recommend that larger and long-term studies are conducted to assess the efficacy and effectiveness of omalizumab in patients with urticarial vasculitis. Read the full article here.
An Updated Therapeutic Strategy for Chronic Idiopathic Urticaria
Nagasai C. Adusumilli MBA and Adam J. Friedman MD FAAD
References
-
- Adusumilli NC, Friedman AJ. An Updated Therapeutic Strategy for Chronic Idiopathic Urticaria. J Drugs Dermatol. 2021 Mar 1;20(3):354-355. doi: 10.36849/JDD.0421. PMID: 33683088.
- El-Qutob D. Off-Label Uses of Omalizumab. Clin Rev Allergy Immunol. 2016 Feb;50(1):84-96. doi: 10.1007/s12016-015-8490-y. PMID: 26048266.
- Liu J, Xiang T, Wang W, Bu Z. Case Report: Omalizumab Successfully Treated Recalcitrant Bullous Pemphigoid in an Elderly Patient with Multiple Comorbidities. Clin Cosmet Investig Dermatol. 2022 Jul 21;15:1391-1396. doi: 10.2147/CCID.S373682. PMID: 35903519; PMCID: PMC9314756.
- Lonowski S, Sachsman S, Patel N, Truong A, Holland V. Increasing evidence for omalizumab in the treatment of bullous pemphigoid. JAAD Case Rep. 2020 Feb 26;6(3):228-233. doi: 10.1016/j.jdcr.2020.01.002. PMID: 32140524; PMCID: PMC7044652.
- Chan S, Cornelius V, Cro S, Harper JI, Lack G. Treatment Effect of Omalizumab on Severe Pediatric Atopic Dermatitis: The ADAPT Randomized Clinical Trial. JAMA Pediatr. 2020;174(1):29–37. doi:10.1001/jamapediatrics.2019.4476
- XOLAIR [prescribing information]. Genentech USA, Inc. and Novartis Pharmaceuticals Corporation; 2021.
- Abuzakouk M, Ghorab O, Namas R, Maurer M. Long-Term Efficacy and Safety of Omalizumab Monotherapy in a Patient With Normocomplementemic Urticarial Vasculitis. J Drugs Dermatol. 2022 Oct 1;21(10):1124-1126. doi: 10.36849/JDD.6739. PMID: 36219045.
- Xolair. (2019). Epocrates medical references. https://online.epocrates.com/drugs/350810/Xolair/Monograph
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.