Primary hyperhidrosis (PHH) is a dermatologic condition characterized by overactivity of eccrine glands resulting in excessive sweating primarily affecting the palms, soles, axillae, and craniofacial area. PHH is not caused by other conditions, whereas secondary hyperhidrosis is caused by an underlying medical condition or medication side effect. Botulinum toxin injections are often used as second line therapy for PHH once a patient fails topical treatment.1-10 We continue our series, Therapeutic Cheat Sheet, with a closer look at Botulinum toxin for the treatment of axillary PHH.
OnabotulinumtoxinA for Primary Axillary Hyperhidrosis
Therapeutic Cheat Sheet
Compiled by: Kamaria Nelson, MD | Reviewed by: Adam Friedman, MD
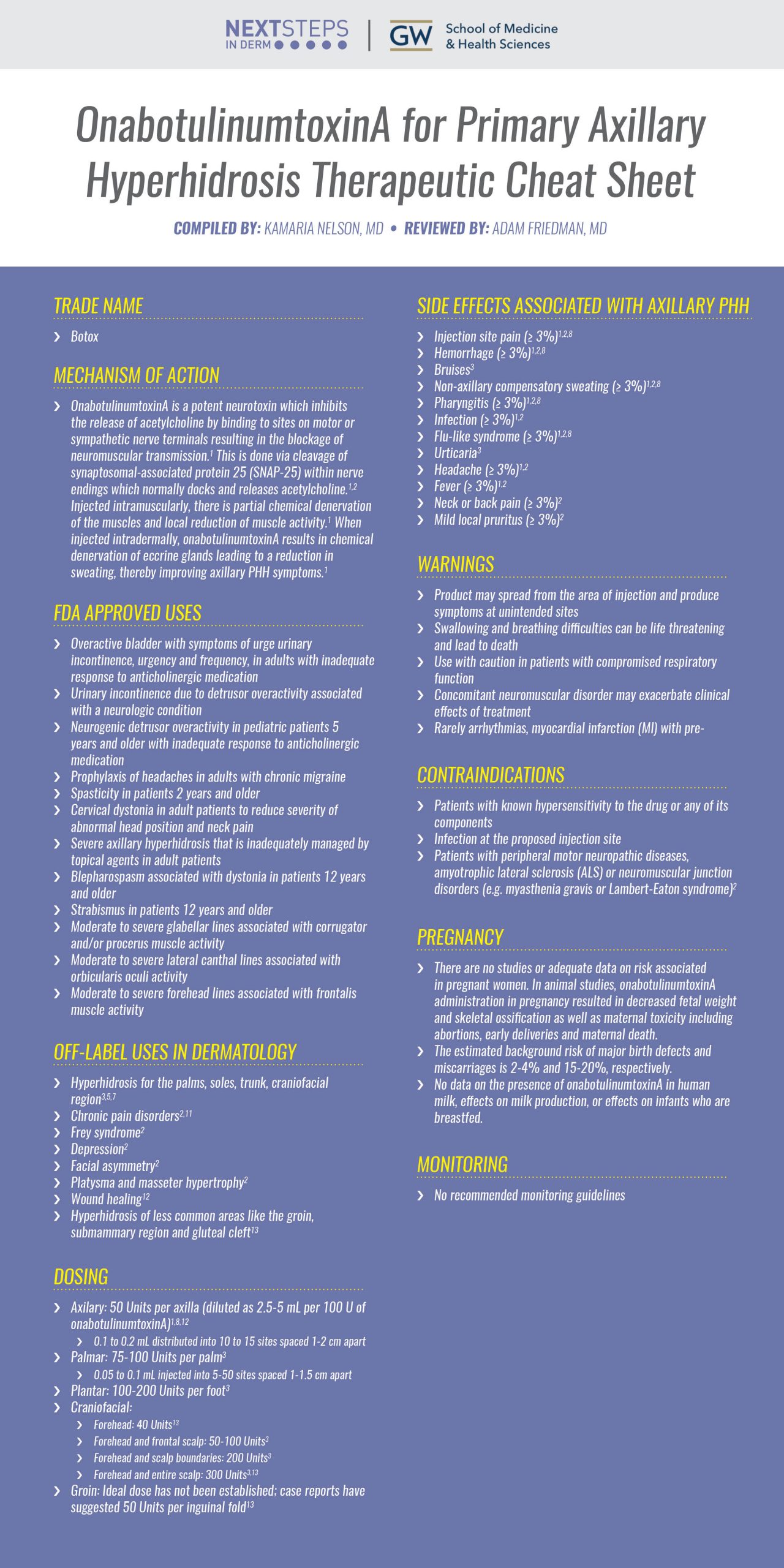
TRADE NAME
-
- Botox
ONABOTULINUMTOXINA MECHANISM OF ACTION
-
- OnabotulinumtoxinA is a potent neurotoxin which inhibits the release of acetylcholine by binding to sites on motor or sympathetic nerve terminals resulting in the blockage of neuromuscular transmission.1 This is done via cleavage of synaptosomal-associated protein 25 (SNAP-25) within nerve endings which normally docks and releases acetylcholine.1,2 Injected intramuscularly, there is partial chemical denervation of the muscles and local reduction of muscle activity.1 When injected intradermally, onabotulinumtoxinA results in chemical denervation of eccrine glands leading to a reduction in sweating, thereby improving axillary PHH symptoms.1
FDA APPROVED FOR
-
- Overactive bladder with symptoms of urge urinary incontinence, urgency and frequency, in adults with inadequate response to anticholinergic medication
- Urinary incontinence due to detrusor overactivity associated with a neurologic condition
- Neurogenic detrusor overactivity in pediatric patients 5 years and older with inadequate response to anticholinergic medication
- Prophylaxis of headaches in adults with chronic migraine
- Spasticity in patients 2 years and older
- Cervical dystonia in adult patients to reduce severity of abnormal head position and neck pain
- Severe axillary hyperhidrosis that is inadequately managed by topical agents in adult patients
- Blepharospasm associated with dystonia in patients 12 years and older
- Strabismus in patients 12 years and older
- Moderate to severe glabellar lines associated with corrugator and/or procerus muscle activity
- Moderate to severe lateral canthal lines associated with orbicularis oculi activity
- Moderate to severe forehead lines associated with frontalis muscle activity
OFF-LABEL USES OF ONABOTULINUMTOXINA
-
- Hyperhidrosis for the palms, soles, trunk, craniofacial region3,5,7
- Chronic pain disorders2,11
- Frey syndrome2
- Depression2
- Facial asymmetry2
- Platysma and masseter hypertrophy2
- Wound healing12
- Hyperhidrosis of less common areas like the groin, submammary region and gluteal cleft13
DOSING
-
- Axilary: 50 Units per axilla (diluted as 2.5-5 mL per 100 U of onabotulinumtoxinA)1,8,12
- 1 to 0.2 mL distributed into 10 to 15 sites spaced 1-2 cm apart
- Palmar: 75-100 Units per palm3
- 05 to 0.1 mL injected into 5-50 sites spaced 1-1.5 cm apart
- Plantar: 100-200 Units per foot3
- Craniofacial:
- Forehead: 40 Units13
- Forehead and frontal scalp: 50-100 Units3
- Forehead and scalp boundaries: 200 Units3
- Forehead and entire scalp: 300 Units3,13
- Groin: Ideal dose has not been established; case reports have suggested 50 Units per inguinal fold13
- Axilary: 50 Units per axilla (diluted as 2.5-5 mL per 100 U of onabotulinumtoxinA)1,8,12
SIDE EFFECTS ASSOCIATED WITH AXILLARY PHH
-
- Injection site pain (≤ 3%)1,2,8
- Hemorrhage (≤ 3%)1,2,8
- Bruises3
- Non-axillary compensatory sweating (≤ 3%)1,2,8
- Pharyngitis (≤ 3%)1,2,8
- Infection (≤ 3%)1,2
- Flu-like syndrome (≤ 3%)1,2,8
- Urticaria3
- Headache (≤ 3%)1,2
- Fever (≤ 3%)1,2
- Neck or back pain (≤ 3%)2
- Mild local pruritus (≤ 3%)2
- Anxiety (≤ 3%)2
WARNINGS
-
- Product may spread from the area of injection and produce symptoms at unintended sites
- Swallowing and breathing difficulties can be life threatening and lead to death
- Use with caution in patients with compromised respiratory function
- Concomitant neuromuscular disorder may exacerbate clinical effects of treatment
- Rarely arrhythmias, myocardial infarction (MI) with pre-existing cardiovascular disease
CONTRAINDICATIONS
-
- Patients with known hypersensitivity to the drug or any of its components
- Infection at the proposed injection site
- Patients with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis (ALS) or neuromuscular junction disorders (e.g. myasthenia gravis or Lambert-Eaton syndrome)2
PREGNANCY
-
- There are no studies or adequate data on risk associated in pregnant women. In animal studies, onabotulinumtoxinA administration in pregnancy resulted in decreased fetal weight and skeletal ossification as well as maternal toxicity including abortions, early deliveries and maternal death.
- The estimated background risk of major birth defects and miscarriages is 2-4% and 15-20%, respectively.
- No data on the presence of onabotulinumtoxinA in human milk, effects on milk production, or effects on infants who are breastfed.
MONITORING
-
- No recommended monitoring guidelines
CLICK ON THE IMAGE BELOW TO ENLARGE AND/OR DOWNLOAD YOUR THERAPEUTIC CHEAT SHEET
OnabotulinumtoxinA overall has exhibited a safe, effective and well-tolerated procedure for the treatment of axillary PHH since its initial FDA-approval in 2004. Studies also support its use in a variety of off-label applications, including PHH in other areas such as the palms, soles, trunk and craniofacial area. Practitioners should continue to take note of newly published reports concerning the safety of this therapeutic option in the diversity of clinical settings in which it is utilized.
Further Reading
If you would like to learn more about onabotulinumtoxinA and other neurotoxins for PHH in various sites, check out the following article published in the Journal of the American Academy of Dermatology. Further, the International Hyperhidrosis Society has an online platform with resources and videos demonstrations of key techniques in hyperhidrosis treatment, including off-label use of onabotulinumtoxinA. Additionally, if you would like to learn more about botulinum toxin in wound healing check out the following article published in the Journal of Drugs in Dermatology.
Botulinum toxin: Pharmacology and injectable administration for the treatment of primary hyperhidrosis, published in the Journal of the American Academy of Dermatology
Shiri Nawrocki BA, Jisun Cha MD
Botulinum neurotoxin Type A as an adjuvant to reduce scarring after dermatological surgery, published in the Journal of Drugs in Dermatology
Dinesh Maini MD
Abstract:
Botulinum neurotoxin type A (BoNTA) is thought to have biological effects beyond muscle paralysis, including direct effects on wound healing. This provides a potential rationale for adjuvant intradermal BoNTA injection in selected patients undergoing minor dermatological surgeries, such as sebaceous cyst or intradermal naevus excision, which often lead to problematic scarring. Case studies are presented showing that BoNTA treatment may be associated with more rapid post-procedural healing and less visible scarring. These case reports of adjuvant intradermal BoNTA injection could justify the initiation of prospective trials in this setting.
References
-
- Allergan: BOTOX® (onabotulinumtoxinA) for injection, for intramuscular, intradetrusor, or intradermal use. Package Insert. US Prescribing Information and Patient Information. Revised 2021 Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/103000s5318lbl.pdf
- Murray C, Sollish N. Botulinum Toxin Injections. Comprehensive Dermatologic Drug Therapy, 60, 656-664.e2.
- Nawrocki S, Cha J. Botulinum toxin: Pharmacology and injectable administration for the treatment of primary hyperhidrosis. J Am Acad Dermatol. 2020 Apr;82(4):969-979. doi: 10.1016/j.jaad.2019.11.042. Epub 2019 Dec 4. PMID: 31811879.
- McConaghy JR, Fosselman D. Hyperhidrosis: Management options. American family physician. 2018;97(11):729-734. https://www.ncbi.nlm.nih.gov/pubmed/30215934.
- Liu V, Farshchian M, Potts GA. Management of primary focal hyperhidrosis: An algorithmic approach. J Drugs Dermatol. 2021;20(5):523-528. Accessed Sep 20, 2021. doi: 10.36849/JDD.5774.
- Lowe NJ, Glaser DA, Eadie N, Daggett S, Kowalski JW, Lai P. Botulinum toxin type A in the treatment of primary axillary hyperhidrosis: A 52-week multicenter double-blind, randomized, placebo-controlled study of efficacy and safety. J Am Acad Dermatol. 2007;56(4):604-611. Accessed Sep 20, 2021. doi: 10.1016/j.jaad.2007.01.009.
- Nawrocki S, Cha J. The etiology, diagnosis, and management of hyperhidrosis: A comprehensive review: Etiology and clinical work-up. J Am Acad Dermatol. 2019;81(3):657-666. Accessed Sep 20, 2021. doi: 10.1016/j.jaad.2018.12.071.
- Coté TR, Mohan AK, Polder JA, Walton MK, Braun MM. Botulinum toxin type A injections: Adverse events reported to the US food and drug administration in therapeutic and cosmetic cases. J Am Acad Dermatol. 2005;53(3):407-415. Accessed Sep 20, 2021. doi: 10.1016/j.jaad.2005.06.011.
- Naumann M, Jankovic J. Safety of botulinum toxin type A: A systematic review and meta-analysis. Curr Med Res Opin. 2004;20(7):981-990. Accessed Sep 20, 2021. doi: 10.1185/030079904125003962.
- Nawrocki S, Cha J. Botulinum toxin: Pharmacology and injectable administration for the treatment of primary hyperhidrosis. Journal of the American Academy of Dermatology. 2020;82(4):969-979. https://www.jaad.org/article/S0190-9622(19)33134-2/abstract. Accessed Sep 20, 2021. doi: 10.1016/j.jaad.2019.11.042.
- Asad U, Austin B, Tarbox M, Paulger B. Botulinum toxin in the long-term treatment of refractory raynaud’s phenomenon. J Drugs Dermatol. 2019;18(9):943-945. Accessed Sep 20, 2021.
- Maini D. Botulinum neurotoxin type A as an adjuvant to reduce scarring after dermatological surgery. J Drugs Dermatol. 2021;20(6):677-680. Accessed Sep 20, 2021. doi: 10.36849/JDD.2021.5807.
- Glaser DA, Galperin TA. Botulinum toxin for hyperhidrosis of areas other than the axillae and palms/soles. Dermatol Clin. 2014 Oct;32(4):517-25. doi: 10.1016/j.det.2014.06.001. Epub 2014 Jul 28. PMID: 25152345.
- User S. Botox® – international hyperhidrosis society | official site.https://www.sweathelp.org/hyperhidrosis-treatments/botox.html. Accessed Sep 21, 2021.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.