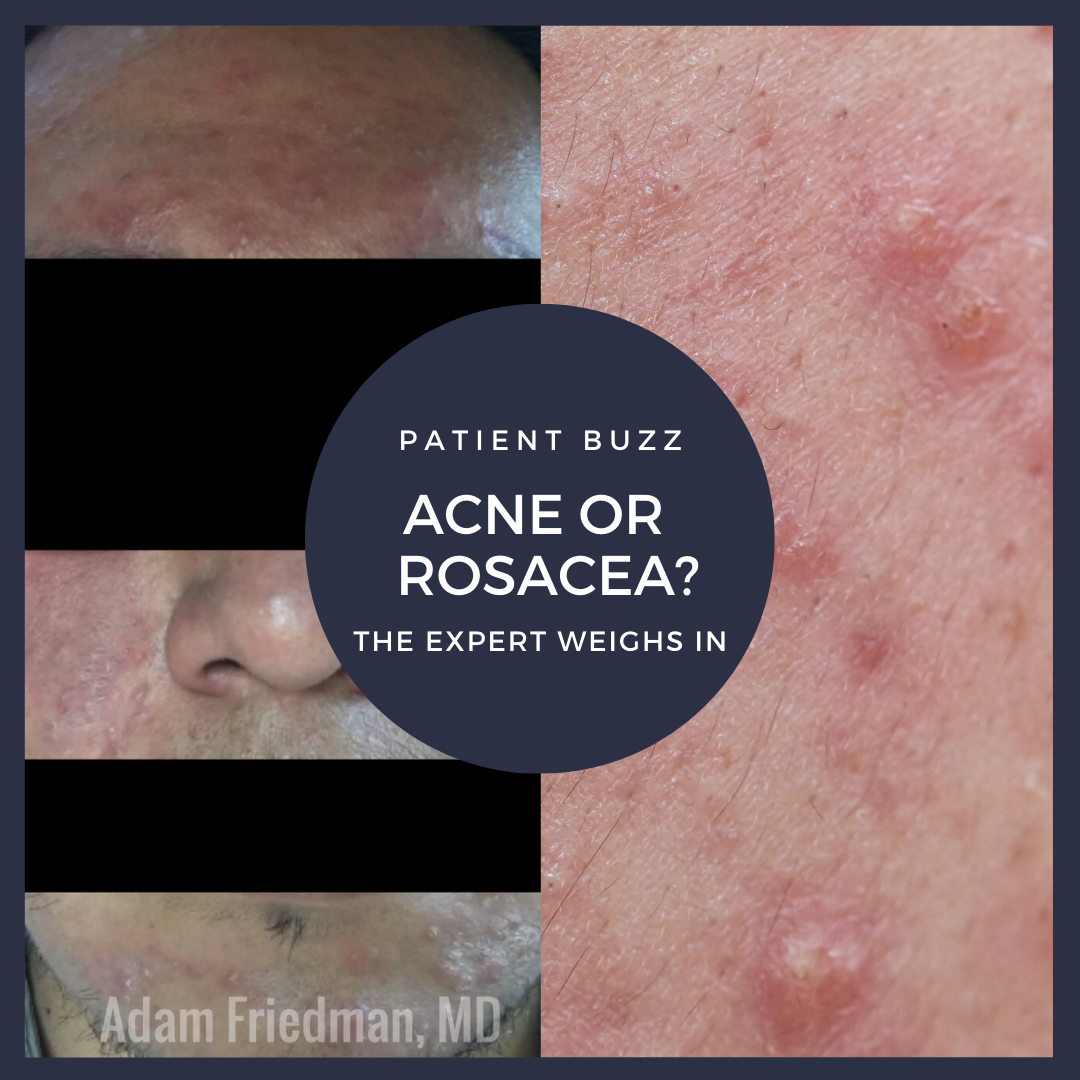
Popsugar/Yahoo! Life recently posted an article about papulopustular rosacea and how common it is misdiagnosed.
For expert advice on how to correctly diagnose papulopustular rosacea, I consulted dermatologist Linda Stein Gold, MD, director of dermatology clinical research at Henry Ford Health System in Detroit, Mich., as well as division head of dermatology at Henry Ford Health System in West Bloomfield, Mich.
What are some keys to diagnosing papulopustular rosacea?
It can be confusing to differentiate acne from rosacea. They both have papules and pustules. Rosacea generally has some background erythema and telangiectasias. In addition, comedones are seen in acne and not rosacea.
What are your pearls for treating papulopustular rosacea?
Look at the individual signs that are present. If background erythema is present, think about using an alpha-adrenergic agonist. If you see papules and pustules, consider a topical or oral anti-inflammatory agent. Always ask about symptoms of ocular rosacea.
Is there any new research of note on papulopustular rosacea, and what does the new research reveal?
We have some exciting new drugs for rosacea, including topical minocycline foam, which was recently FDA approved. A topical encapsulated benzoyl peroxide also shows promise in clinical trials as does low-dose oral minocycline.
What are the most important messages dermatologists should communicate to their patients with papulopustular rosacea?
It is important to individualize treatment based on the needs of the patient and remember to counsel on appropriate skin care: avoid harsh cleansers and toners, moisturize for barrier repair and don’t forget sunscreen.
Further Reading
If you want to correctly diagnose rosacea, check out the following articles recently published in the Journal of Drugs in Dermatology.
 Recognizing Rosacea: Tips on Differential Diagnosis
Recognizing Rosacea: Tips on Differential Diagnosis
Rosacea is a common chronic inflammatory dermatosis with a variety of clinical manifestations. Rosacea primarily affects the central face, and includes papules, pustules, erythema, telangiectasias, perilesional redness, phymatous changes, and even ocular involvement. Symptoms may vary among different patients and even vary over time in an individual patient. Central facial redness affects many adults and can be an indicator of the chronic inflammatory disease rosacea. Rosacea is a clinical diagnosis based on the patient’s history, physical examination, and exclusion of other disorders. It is under-diagnosed, particularly in individuals with skin of color. The goal of this article is to provide clinicians with the tools and understanding needed to correctly identify rosacea and differentiate it from other conditions that have overlapping signs and symptoms.
 Patient-focused Solutions in Rosacea Management: Treatment Challenges in Special Patient Groups
Patient-focused Solutions in Rosacea Management: Treatment Challenges in Special Patient Groups
Rosacea is among the most common facial skin conditions diagnosed by dermatologists. Typical clinical features include erythema, flushing, telangiectasia, papules, and pustules distributed on the central face. While the prevalence of rosacea is highest among white populations of Northern European descent, recent reports have found that rosacea frequently occurs in people from a broad range of racial/ethnic backgrounds and skin types. When rosacea presents in darker skin types, the diagnosis is often more challenging due to masking of features by increased epidermal melanin. As such, under-diagnosis and underreporting may contribute to misconceptions about the prevalence of rosacea in populations with skin of color. Recognizing the unique presentations and complications associated with darker skin types is necessary to reduce the disparities in rosacea treatment, especially as the American population continues to become increasingly heterogeneous. Although rosacea is most common in middle-aged females, patients of other demographics may have more negative impacts on quality of life due to their disease. In this article, we review rosacea management with a focus on special patient groups: people with skin of color, and less common forms of rosacea, in order to diminish the physical and psychosocial burden of rosacea in all patient groups. Due to the variability inherent to rosacea, we advocate for an individualized, patient-centered approach to disease management.
Did you enjoy this Patient Buzz Expert Commentary? You can find more here.