JDD authors Amelia M. Abbott-Frey BA, Alexandra J. Coromilas MD, George W. Niedt MD, and Jesse M. Lewin MD report a case of linear porokeratosis with recurrent malignant degeneration to squamous cell carcinoma (SCC) recurring six years after excision of initial SCC.
Case Report
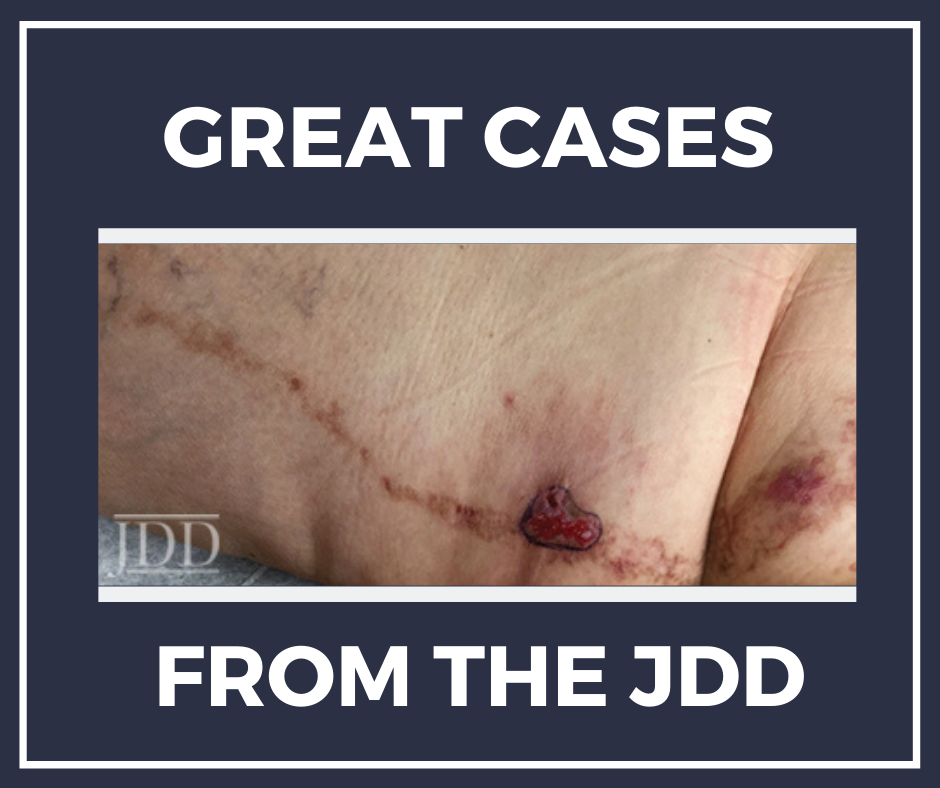
A 79-year-old woman with a history of hypertension and hypothyroidism presented with a friable tumor within a lesion on the left buttock and posterior thigh which has been present for her entire life. She was diagnosed with squamous cell carcinoma (SCC) arising within the linear plaque six years prior, which was surgically excised with negative margins. Physical examination revealed a hyperpigmented and erythematous scaly linear plaque within a line of Blaschko, extending from the left buttock to the left distal posterior thigh (Figure 1). There was a 3.5 x 2.7 cm friable tumor on the proximal posterior thigh within the linear plaque.

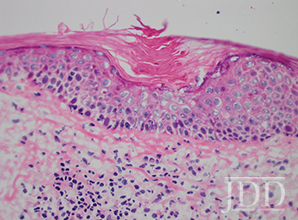
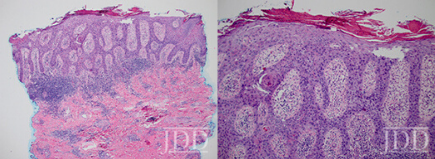
Two 4 mm punch biopsies were performed: one of the erythematous plaque on the left buttock and one from the friable tumor on the left posteromedial thigh. Histology revealed a cornoid lamella consistent with porokeratosis on the left buttock (Figure 2) along with SCC in situ (Figures 3 and 4) on the posteromedial thigh. The patient subsequently underwent 1 stage of Mohs micrographic surgery with complete tumor extirpation, followed by a linear repair.
Discussion
Porokeratosis is a disorder of epidermal keratinization. There are several clinical variants of porokeratosis including porokeratosis of Mibelli, punctate porokeratosis, disseminated superficial porokeratosis, disseminated superficial actinic porokeratosis, porokeratosis plantaris palmaris et disseminate, and linear porokeratosis. Histologically these lesions are characterized by a cornoid lamella, which is a compact column of parakeratosis. Although porokeratosis has historically been viewed as a benign lesion, there is evidence that these lesions may demonstrate malignant transformation. Research suggests that malignant degeneration occurs in about 7.5-11% of porokeratoses, commonly presenting as Bowen’s disease, SCC, or basal cell carcinoma.1,2 The risk of malignancy is hypothesized to be related to abnormal DNA ploidy in cells of the cornoid lamella as well as aberration of the p53 protein.3
Linear porokeratosis (LP) is an uncommon form of porokeratosis that is typically congenital, though lesions may arise in adulthood. LP’s follow Blaschko lines and are most often unilateral; however, they can rarely be generalized.3 Of all variants of porokeratosis, LP carries the highest risk for malignant transformation, estimated to occur in up to 19% of cases.11Our patient’s lesion was clinically consistent with LP, which was confirmed histologically. She had multiple risk factors for malignant transformation including a large, long-standing lesion, and location on the extremity.3-4 Other known risk factors for malignant transformation include sun exposure, immunosuppression, and ionizing radiation.1,2,4,5While there are a few cases in the literature of multiple squamous cell carcinomas arising within linear porokeratosis, to our knowledge this is the first case to present with recurrence of a malignancy treated six years prior. This case highlights the importance of regular monitoring and surveillance for malignant degeneration in patients with large and long-standing linear porokeratosis.
References
1. Sasson, M, Krain, A. Porokeratosis and cutaneous malignancy: a review. Dermatol Surg. 1996;22:339-42. 2. Maubec E, Duvilard P, Margulis A. Common skin cancers in porokeratosis. Br J Dermatol. 2005;152:1389–91.
3. Sertznig P, von Felbert V, Megahed M. Porokeratosis: present concepts. JEADV. 2012;26:404-412.
4. Otsuka F, Umebayashi Y, Watanabe S, Kawashima M, et al.Porokeratosis large skin lesions are susceptible to skin cancer development: histological and cytological explanation for the susceptibility. J Cancer Res Clin Oncol. 1993;119:295–400.
5. Bencini PL, Tarantino A, Grimalt R, Ponticelli C, et al. Porokeratosis and immunosuppression. Br J Dermatol. 1995;132:74–8.
Source:
Amelia M. Abbott-Frey BA, Alexandra J. Coromilas MD, George W. Niedt MD, Jesse M. Lewin MD (2020). Recurrent Squamous Cell Carcinoma Arising Within a Linear Porokeratosis. Journal of Drugs in Dermatology, 19 (2). https://jddonline.com/articles/dermatology/S1545961620P0005X/1
This JDD article is early online, a new feature of the JDD continue publishing model.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.
Next Steps in Derm is brought to you by SanovaWorks.