Atopic dermatitis is a heterogeneous, chronic inflammatory disease that affects upwards of 10% of children and 7% of adults in the United States. Despite being an incredibly common skin concern among patients, AD continues to pose diagnostic and treatment challenges to dermatologists.
What are some common misconceptions about AD?
-
- AD always starts in childhood. FALSE. 25% of adults with AD develop it for the first time as an adult.
- AD is a clinically homogenous disease. FALSE. AD has a heterogenous presentation that includes a spectrum of clinical impressions.
- AD only affects the skin. FALSE. There are numerous associated co-morbidities associated with the chronic inflammation burden.
- Assessing clinical severity is straightforward. FALSE. Validated research tools can be helpful, but it is challenging to document the patient’s disease burden in clinical care.
- AD diagnosis is determined by skin biopsy or blood test. FALSE. AD is a clinical diagnosis.
During the 2022 ODAC meeting in Orlando, Dr. Adam Friedman did a rapid-fire review of the state of atopic dermatitis with high yield updates in the diagnosis and management of this common inflammatory disease.
Diagnosing Atopic Dermatitis
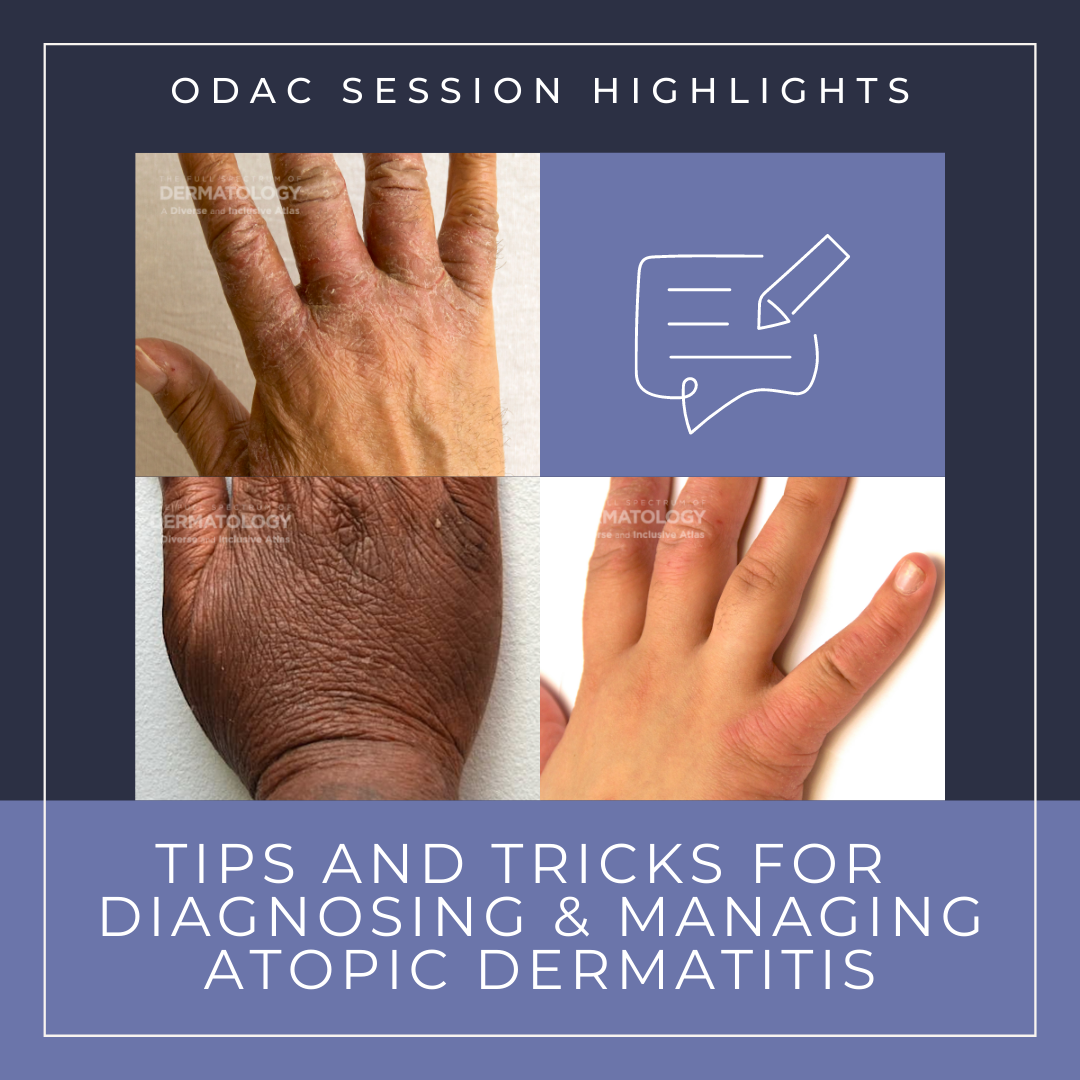
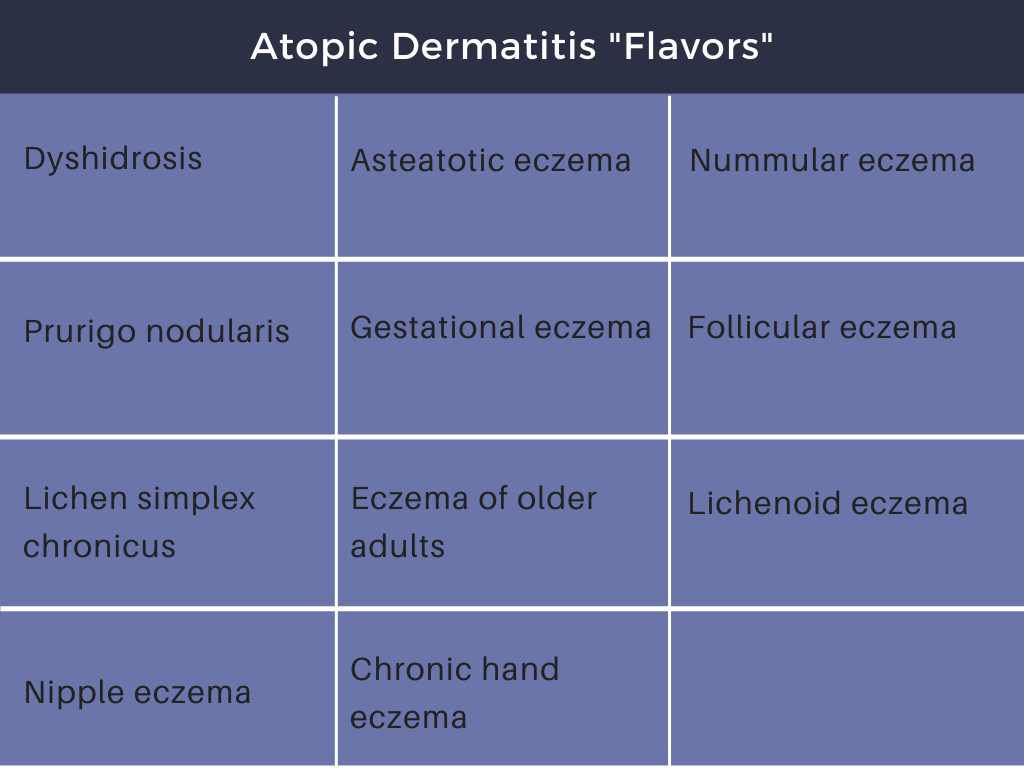
Despite its prevalence, Dr. Friedman reminded us that there can be significant diagnostic challenges due to the wide spectrum of presentation of AD. AD is a clinical diagnosis of a pruritic, relapsing eruption with typical morphology and age-specific distribution. There is great emphasis on the pruritus as a feature, or what Dr. Friedman refers to as “the itch that feels good to scratch”. Pruritus is truly essential for diagnosing AD. Beyond that, AD can come in many flavors (Table 1). AD diagnosis is supported by childhood onset, features of atopy, elevated serum IgE and generalized xerosis, although these are not essential. Further, there are many associated clinical features such as keratosis pilaris and pityriasis alba that can be seen in the setting of AD. More recently, there has been evidence that AD may not be only skin deep. In addition to comorbid infections such as impetiginization with Staphylococcus aureus and eczema herpeticum, there are additional comorbidities pertaining to sleep disturbance, mental health, and potential cardiovascular disease. If there is doubt, however, in the diagnosis, a biopsy can be helpful.
Tip: Biopsy an area that has been untreated for at least 3 weeks.
Approach to Management
Now that we feel certain of the diagnosis of AD in a patient, how do we go about management? Before we talk about the approach to treatment, Dr. Friedman reminded us that documentation is key to assist with coverage of medications. It is critical that the diagnosis, severity, and related co-morbidities are clearly and consistently documented to maximize success when dealing with the payer. Even features such as sleep disturbance and impairment in school can be critical details for successful coverage for medications.
Dr. Friedman started with what he has coined the EASY E’s of management of atopic dermatitis: education, expectations, encouragement, and enough:
-
- Education: It is important the patient and anyone involved in their care, including family and teachers, have an understanding of atopic dermatitis. One particularly helpful resource is the National Eczema Foundation that has succinct guides, such as the one found here.
- Expectations: The goals of treatment are to reduce the severity of symptoms and the duration of flares. We know we are unable to promise a cure for AD. These are important discussions to set expectations for the natural course of AD and what effective treatment really looks like. Without this conversation, it is possible that patients will consider any treatment a failure if their rash returns after stopping treatment.
- Encouragement: Patients need close follow-up and support to continue with the plan. Dr. Friedman recommended close follow-up to make sure the treatment plan is being done correctly and leading to improvement.
- Enough: Enough medication that is. Patients need large quantities of topicals when treating large areas of AD-affected skin on a regular basis.
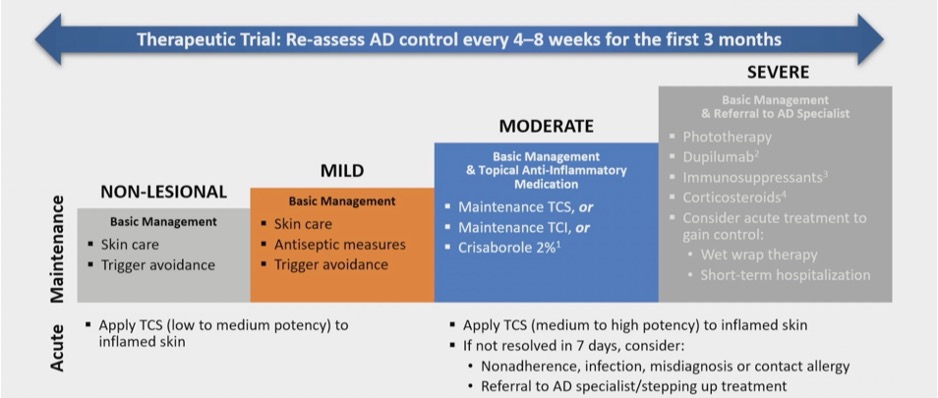
Beyond these basics that apply to every AD patient, the treatment plan should be customized for your patient. Dr. Friedman advised the severity and response to therapy should guide treatment: build on basic measures as needed and reassess the response (see Figure 1).
While a great therapeutic plan may be formulated in the clinic, its efficacy is achieved by what the patients do at home. To improve adherence to the treatment plan, it is important to discuss what has gone well and what has gone wrong in the past, including teasing out the details of what they have used in the past and for how long to understand what barriers may exist for adherence. Dr. Friedman advised steroid phobia is also a concern among patients and may be something to address up front. Fortunately, there is no evidence of hypothalamic-pituitary axis suppression unless using more than 50 grams of ultra-potent corticosteroids per week.
Tip: Consider once a day application of topicals to improve adherence. For many topicals, twice daily application only results in marginally better outcomes.
Dr. Friedman shared his treatment algorithm for patients being managed with topical medications. He starts with a higher potency corticosteroid one to two times daily for a relatively short period of time (2-4 weeks) to achieve clearance during a flare. He then recommends an intermittent regimen for maintenance, which may be a moderate potency corticosteroid a few days a week. He also recommended incorporating a nonsteroidal topical treatment as part of proactive therapy to prevent flares. Topical calcineurin inhibitors (TCI) are a great option, although patients need to be warned there is an expected initial burning discomfort as well as the black box warning. Fortunately, no evidence of increased risk of malignancy has ever been found for TCIs. The phosphodiesterase 4 inhibitor crisaborole ointment is another steroid alternative. In Dr. Friedman’s experience, this treatment can also cause burning discomfort on initial application. Its FDA approval for infants over 3 months of age makes it appealing in very young patients. Lastly, the topical Jak kinase inhibitor ruxolitinib cream 1.5% has very recently been approved for use for up to 8 weeks adding to the arsenal of steroid sparing agents.
When Topical are Not Enough
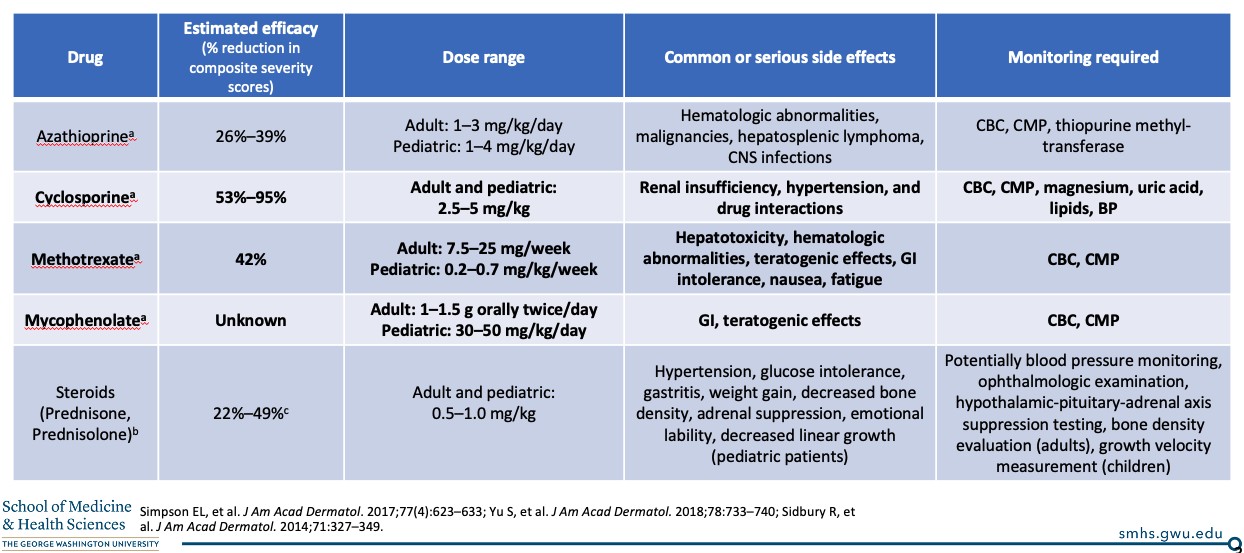
In patients with moderate to severe AD that cannot achieve adequate clinical response with topical therapies alone, systemic treatment is indicated. Dr. Friedman shared some of his favorite classic oral immunosuppressant medications that are commonly used off-label for the treatment of AD (see Table 2).
What about the new age of AD therapies that are FDA approved for the treatment of AD? Dupilumab, which blocks the IL-4Ra subunit of cytokines IL-4 and IL-13, is currently approved for moderate to severe AD 6 years and older. Due to the cost of this medication, it is not uncommon for the payer to require failure of topical steroids, TCI for at least 6 weeks and often an oral immunosuppressant as well. Dr. Friedman highlighted some notable clinical features of dupilumab that have supportive data:
-
- Is it safe in pregnancy? Registry data supports safety in pregnant persons.
- Is it a concern in cases of COVID-19? The clinical syndrome appears to be attenuated in patients on dupilumab, demonstrating a potential protective mechanism during infection.
- What if patients flare before their next injection on the typical 2-week schedule? There is evidence that some patients benefit from weekly dosing, and there is safety data supporting this.
- What are the adverse effects? Ocular disease, inflammatory arthritis, alopecia great and facial dermatitis have been reported.
Dupilumab is no longer the only drug that can impact IL-13 signaling, as tralokinumab has been recently approved to treat AD in adults. Its mechanism is slightly different in that tralokinumab inhibits the IL-13 cytokine itself, as opposed to the receptor. Notably, treatment consists of 2 injections every 2 weeks, although it can be reduced to monthly if well controlled. Its adverse effect profile is similar, with conjunctivitis being common.
Tip: If your patient has known ocular symptoms prior to initiating either FDA approved biologic for AD, Dr. Friedman advised to start prophylactic artificial tears to potentially prevent the onset of these symptoms.
What else is new? Excitedly, several oral JAK kinase inhibitors have very recently been approved for the treatment of AD, including upadicitinib for patients 12 and up and abrocitinib in adults. Time will tell how these medications fit into the rapidly expanding treatment toolbox for AD!
This information was presented by Dr. Adam Friedman at the 2022 ODAC Dermatology, Aesthetic and Surgical Conference held January 14-17, 2022. The above highlights from his lecture were written and compiled by Dr. Edita Newton.
Photo Credit: The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas
Did you enjoy this article? Find more on Atopic Dermatitis (AD) here.