The following two cases presented by JDD authors Ryan A. Gall MD, John D. Peters MD, and Alyson J. Brinker MD add to the growing literature supporting the use of dupilumab in the treatment of patients with recalcitrant dyshidrotic eczema, both with and without diagnosed contact allergens.
Introduction
Dyshidrotic eczema, also known as dyshidrosis or pompholyx when involving larger bullae, is a chronic, relapsing palmoplantar dermatosis characterized by intensely pruritic and frequently painful deep-seated vesicles and bullae. Often likened to tapioca pudding, the vesicles typically erupt on the lateral aspects of the fingers and persist for several weeks before progressing to desiccation and desquamation.1Perpetual cycles of relapse and remission frequently last several years and recurrence is common.
Rather than an independent disease entity, dyshidrotic eczema is often thought to be a manifestation of other eczematous dermatosis such as atopic dermatitis or contact dermatitis (allergic and irritant).2,3 Factors thought to be associated with the development of dyshidrotic eczema include a history of atopic dermatitis,4 a history of allergic contact dermatitis,4-6exposure to contact irritants,7 id reactions,8 IVIG exposure,6,8,9hyperhidrosis,4 smoking,5-7 and sunlight exposure.10
Basic treatment strategies for all patients with dyshidrotic eczema include avoidance of contact irritants, gentle skin care to reduce irritation, and use of emollients to restore barrier function.11 Mild to moderate cases may be treated with topical steroids, calcineurin inhibitors, and ultraviolet light (narrow band UV-B and UVA1). Treatment failure with first line topical agents is common, and more potent treatments such ultra-high potency topical corticosteroids under occlusion, systemic corticosteroids, psoralen-ultraviolet A therapy (PUVA), and systemic immunosuppressants such as methotrexate, mycophenolate mofetil, cyclosporine, and azathioprine are often used. Unfortunately, many cases of dyshidrotic eczema are recalcitrant to multiple treatment trials, resulting in significant morbidity. In this series, we discuss two cases of recalcitrant dyshidrotic eczema that had profound improvement after treatment with dupilumab.
Case 1
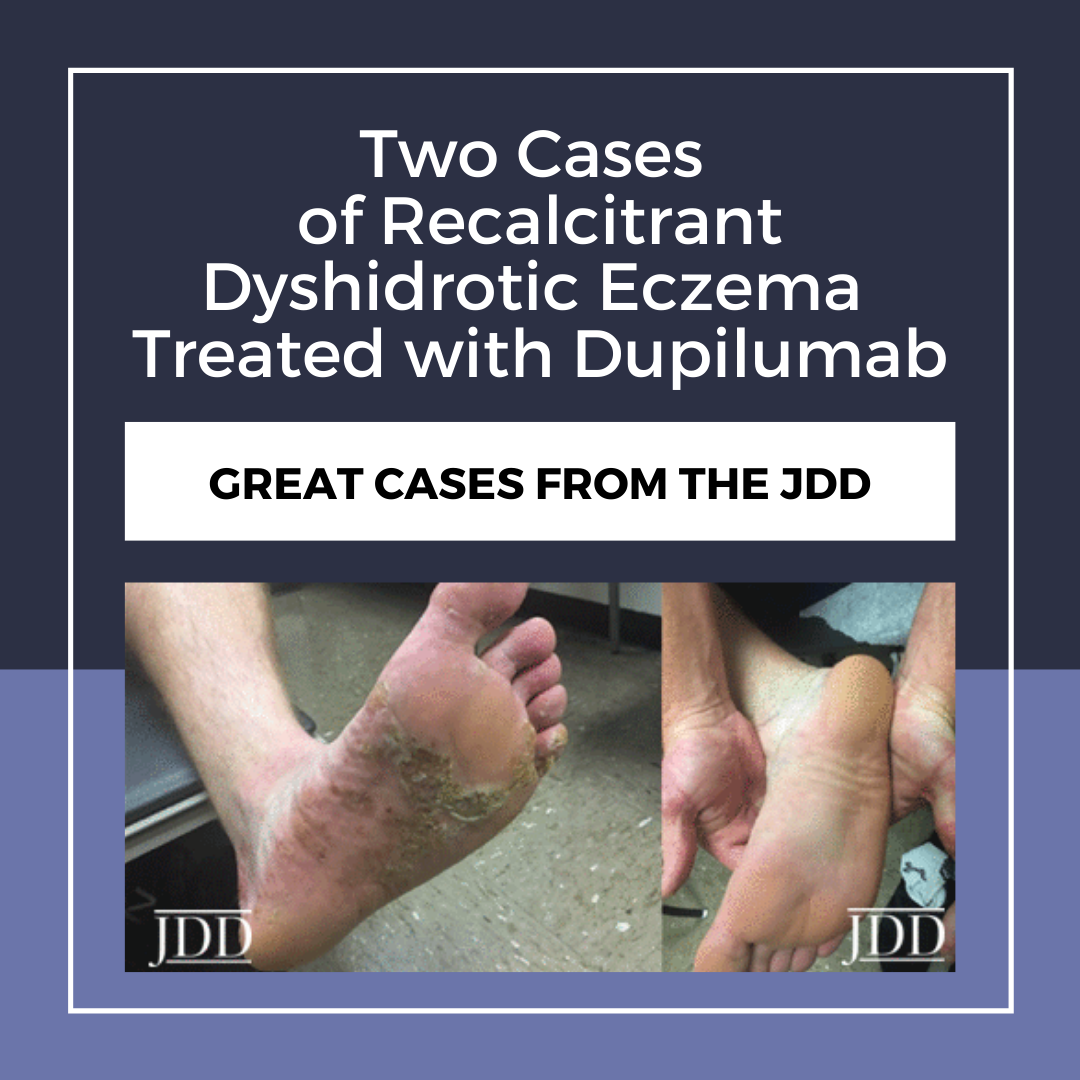
A 38-year-old male Chief Petty Officer in the United States Navy presented to the Dermatology Clinic with a five-year history of firm, intensely pruritic vesicles on his hands and feet. He had been previously treated with keratolytic agents, topical clobetasol, PUVA, and acitretin without significant improvement of symptoms. Biopsy of the palm demonstrated spongiotic dermatitis with intraepidermal vesicle formation supporting the diagnosis of dyshidrotic eczema. Patch testing showed reactions to benzocaine, nickel sulfate, methylisothiazolinone, iodoproponyl butylcarbamate, cocamidopropyl betaine, and formaldehyde. Despite avoidance and adherence to a low nickel diet, he only had mild improvement of symptoms. He continued to report a sensation akin to “constantly walking on Legos.” Treatment with 60mg of intramuscular triamcinolone led to complete resolution of symptoms, but recurrence occurred within 1 month. He was started on dupilumab 600mg subcutaneously (SQ) followed by 300mg SQ every other week with clobetasol as needed. At follow up, he noted rapid and profound improvement beginning within 1 week of his first dose. At 6 months, improvement was sustained without application of clobetasol.

Case 2

Discussion
Dyshidrotic eczema is a distinct entity thought to be on the clinical spectrum with atopic dermatitis. It is often difficult to control, and relapses are common after cessation of therapy. To date, there have been few randomized control trials for the treatment of dyshidrotic eczema and no FDA approved treatment exists. Current treatment options for refractory cases are limited by poor efficacy and significant side effects. Systemic corticosteroids are often effective but are generally not a viable long-term option. Immunosuppressants are limited by their significant side effect profile and relapse typically occurs after discontinuation.14,15 Dupilumab is typically very well tolerated with a low side effect profile, with the most common adverse effects being conjunctivitis, injection site reaction, and localized herpes simplex.12
These two cases add to the newly emerging evidence that dupilumab can be used as a highly effective treatment for patients with unmanageable dyshidrotic eczema on the palms or soles. To date, four other total cases of the successful treatment of dyshidrotic eczema with dupilumab have been reported in the literature, all of which have been associated with profound and sustained responses.16-18 This case series adds to the growing literature supporting the use of dupilumab in the treatment of patients with recalcitrant dyshidrotic eczema, both with and without diagnosed contact allergens.
Disclosures
The authors of this publication have no disclosures, relevant financial relationships, patents, or conflicts of interest to report. Disclaimer: The views expressed in this article are those of the authors and do not reflect the official position of the institution, the Department of the Navy, the Department of Defense, or the US Government.
References
2. Agner T, Aalto-Korte K, Andersen KE, et al. Classification of hand eczema. J Eur Acad Dermatol Venereol. 2015;29(12):2417-2422.
3. Meding B, Swanbeck G. Epidemiology of different types of hand eczema in an industrial city. Acta Derm Venereol. 1989;69(3):227-233.
4. Lodi A, Betti R, Chiarelli G, Urbani CE, Crosti C. Epidemiological, clinical and allergological observations on pompholyx. Contact Dermatitis. 1992;26(1):17-21.
5. Jain VK, Aggarwal K, Passi S, Gupta S. Role of contact allergens in pompholyx. J Dermatol. 2004;31(3):188-193.
6. Guillet MH, Wierzbicka E, Guillet S, Dagregorio G, Guillet G. A 3-year causative study of pompholyx in 120 patients. Arch Dermatol. 2007;143(12):1504-1508.
7. de Boer EM, Bruynzeel DP, van Ketel WG. Dyshidrotic eczema as an occupational dermatitis in metal workers. Contact Dermatitis. 1988;19(3):184-188.
8. Pitche P, Boukari M, Tchangai-Walla K. Factors associated with palmoplantar or plantar pompholyx: a case-control study. Ann Dermatol Venereol. 2006;133(2):139-143.
9. Lee KC, Ladizinski B. Dyshidrotic eczema following intravenous immunoglobulin treatment. Can Med Assoc J. 2013;185(11):E530-E530.
10. Man I, Ibbotson SH, Ferguson J. Photoinduced pompholyx: a report of 5 cases. J Am Acad Dermatol. 2004;50(1):55-60.
11. Warshaw EM. Therapeutic options for chronic hand dermatitis. Dermatol Ther. 2004;17(3):240-250.
12. Harb H, Chatila TA. Mechanisms of dupilumab. Clin Exp Allergy. 2020; 50: 5-14.
13. Dupilumab Clinical Trials. Available at : https://clinicaltrials.gov/ct2/results?c ond=&term=dupilumab&cntry1=&state1=&recrs=a. Accessed November 14, 2019.
14. Egan CA, Rallis TM, Meadows KP, Krueger GG. Low-dose oral methotrexate treatment for recalcitrant palmoplantar pompholyx. J Am Acad Dermatol. 1999;40(4):612-614.
15. Pickenacker A, Luger TA, Schwarz T. Dyshidrotic eczema treated with mycophenolate mofetil. Arch Dermatol. 1998;134(3):378-379.
16. Weston GK, Hooper J, Strober BE. Dupilumab in the treatment of dyshidrosis: a report of two cases. J Drugs Dermatol. 2018;17(3):355-356.
17. Nanda S, Nagrani N, MacQuhae F, Nichols A. A case of complete resolution of severe plantar dyshidrotic eczema with dupilumab. J Drugs Dermatol. 2019;18(2):211-212.
18. Weins AB, Biedermann T, Eyerich K, Moeckel S, Schnopp C. Successful treatment of recalcitrant dyshidrotic eczema with dupilumab in a child. J Dtsch Dermatol Ges. 2019.
Source
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.