One of my favorite diseases to treat as a dermatology resident is acne, as I find that it often has a huge impact on quality of life and self-confidence. Patients often come in when they have tried various over the counter medications and holistic treatments with no success and are frustrated at their lack of improvement. The good news for these patients is that there are many new medications that have been recently approved for acne. At the ODAC 2021 Pre-Conference Sneak Peek Inflammatory Diseases Symposium, Dr. Jenna Lester, Assistant Professor at the University of California San Francisco, covered many of the novel acne treatments in her talk Acne: Changing Practices in a Changing Clinical Landscape.
Topical Treatments
Creams are incredibly popular as many patients like having a non-systemic option. A few takeaways on the new topical treatments:
-
- Trifarotene cream, a RAR gamma selective retinoid, is actually approved for both facial and truncal acne. This is great for patients who need broad coverage but do not want a systemic medication. An interesting pearl I learned from Dr. Lester is that trifarotene can be a little sticky, but the majority of patients are willing to tolerate it for the results.
- An open-label, non-comparative study of 455 patients over 52 weeks found trifarotene to be well tolerated, with a 53% increase in quality of life and 57.9% were considered a treatment success.
- Clascoterone cream, a competitive androgen receptor antagonist, helps decrease downstream pathways that cause acne, such as sebum production and activation of inflammatory pathways.
- Two randomized, vehicle-controlled, double-blind studies with over 1000 patients on the efficacy of clascoterone cream found decreases in both inflammatory and non-inflammatory lesions. Dr. Lester noted that efficacy of the topicals can change based on demographics, and these studies did not specify the efficacy of the medications for patients with Fitzpatrick IV-VI skin
- Topical minocycline, an antibiotic, has the least antibiotic resistance along with the best side effect profile of all the tetracyclines. However, minocycline can cause dyspigmentation issues when taken systemically.
- A randomized, double-blind, vehicle-controlled study of 1488 patients found significant improvement in inflammatory lesions of patients using topical minocycline, with 30.8% of patients achieving treatment success. Of note, this study specified the demographics of their subjects, with 16.9% identifying as black and 5.7% as other.
Oral Treatments
For some patients, topical treatment is not sufficient and systemic medications are necessary. Although tetracyclines have been used for many years, a new tetracycline, sarecycline, was introduced recently for the treatment of acne.
-
- Antibiotic stewardship has become more important in dermatology as multidrug-resistant bacteria has increased. Sarecycline is a great choice as it is a narrow spectrum tetracycline due to a modification in the C-7 ring. It has less activity against gram-negative organisms and the intestinal microbiome while still targeting acnes. It also causes less gastrointestinal upset and can lead to better patient adherence with their medication regimens.
- Sarecycline can be taken by patients 9 and older and is dosed by weight (60mg for 73-120lb, 100mg for 121-185lm, and 150 for 186-300lb). It was found to be good for both truncal and facial acne.
- An important clinical pearl I learned today from Dr. Lester is that the gut microbiome is very important for secreting short-chain fatty acids that are anti-inflammatory and can help with acne.
Acne and the Microbiome
I, along with many of the participants at the symposium, are not very confident in talking about the association between acne and skin microbiome. Luckily, Dr. Lester discussed how the two are connected:
-
- Human skin has 1000 commensal species that are essential as they help prevent pathogenic bacteria from overgrowing and are a vital part of healthy skin. Feedback from commensal microbes to our immune system also helps modulate any inflammation and inhibit pathogenic bacteria.
- The main connection between gut organisms and the skin comes from the influence of our microbiome on glycemic control, tissue lipid content, and inflammation, all of which can have an impact on acne and skin diseases
- Unfortunately, there have been very limited clinical trials on topical probiotics and acne. However, Dr. Lester believes this is an area of accelerating research.
- Interestingly, a few studies on oral probiotics have been hopeful. One study showed it was just as effective as minocycline and another study showed decrease in inflammatory lesions.
This was a talk full of clinically relevant information on new and trending topics in acne treatment. I learned so much in regards to new medications and options for patients who have either failed traditional treatments or are hesitant to start a systemic option. The biggest takeaway points from this lecture are:
-
- There are novel topical treatments along with oral antibiotics with minimal impact on gut flora that should be added to every dermatologist’s arsenal of treatments.
- The gut microbiome also likely has a very important role in acne, and the research on their impact on inflammation and glycemic control is just beginning.
Source:
This information was presented by Dr. Jenna Lester at the 2021 ODAC Sneak Peek Inflammatory Diseases Symposium held on December 3rd, 2020. The above highlights from her lecture were written and compiled by Angela Hou, MD, dermatology resident at the George Washington University School of Medicine and Health Sciences in Washington, DC.
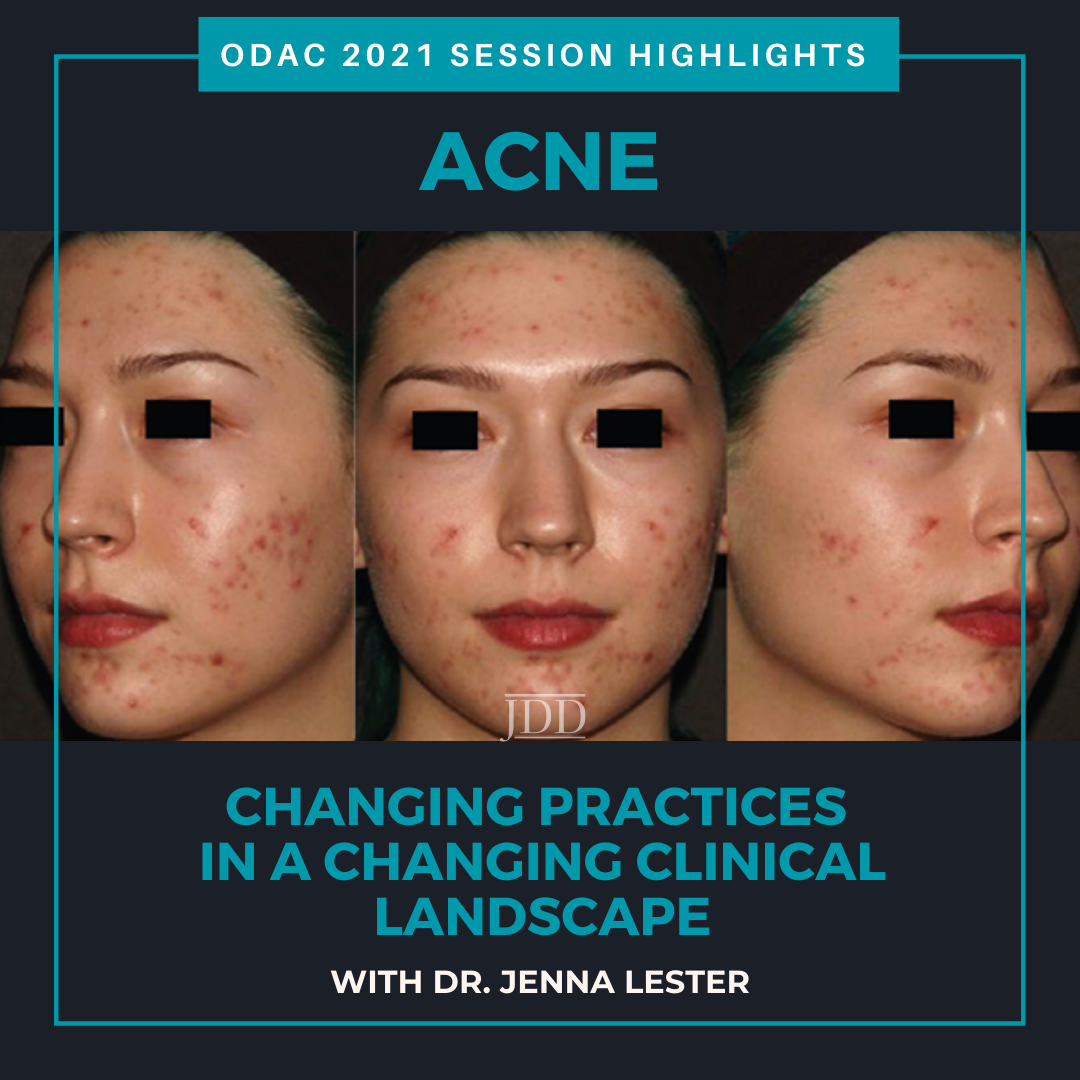
Images:
All images courtesy of the Journal of Drugs in Dermatology.
Did you enjoy this article? Find more on Medical Dermatology here.