During the 2021 ODAC Dermatology, Aesthetic and Surgical Conference held virtually on January 14th-17th, dermatologists from around the country submitted newly published research findings and novel therapeutics in the areas of acne and rosacea, all presented as part of a virtual scientific poster gallery. We share the highlights of each poster below!
![]() Efficacy and Safety of Narrow-spectrum Oral Sarecycline for Moderate to Severe Acne Vulgaris
Efficacy and Safety of Narrow-spectrum Oral Sarecycline for Moderate to Severe Acne Vulgaris
Angela Moore, MD, Lawrence J. Green MD, Jodi L. Johnson, MD, Ayman Grada, MD
Introduction
-
- Sarecycline is a narrow-spectrum tetracycline-class antibiotic designed for the treatment of moderate-to-severe acne.
- Sarecycline’s narrow-spectrum anti-bacterial activity and lipophilicity may minimize side effects commonly associated with broad-spectrum tetracyclines, such as minocycline and doxycycline.
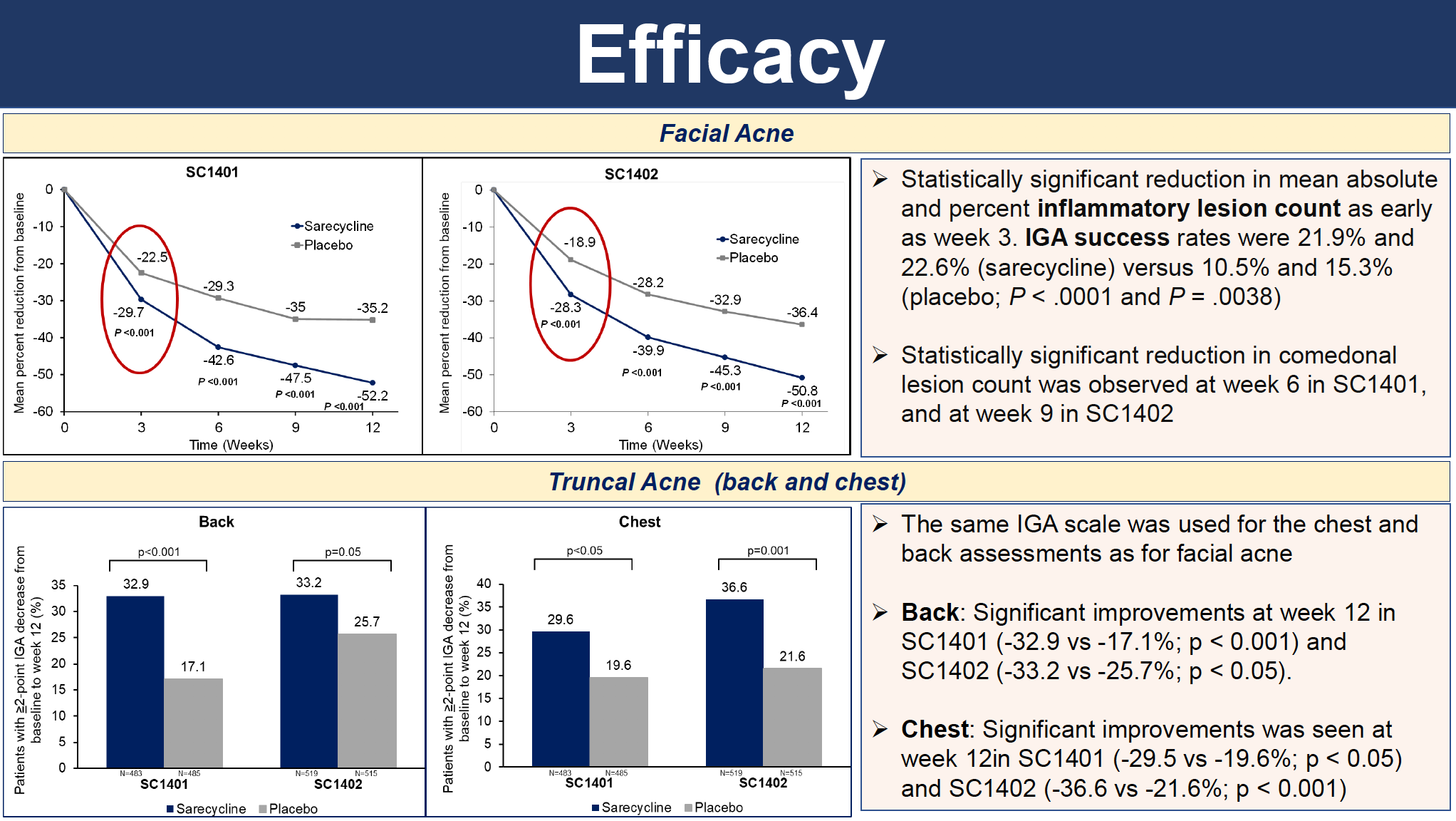
- Moore A, MD et al. report the results of 2 identically designed, phase 3 pivotal trials, SC1401 and SC1402, to evaluate the efficacy and safety of once-daily sarecycline (n=2002).
Conclusions
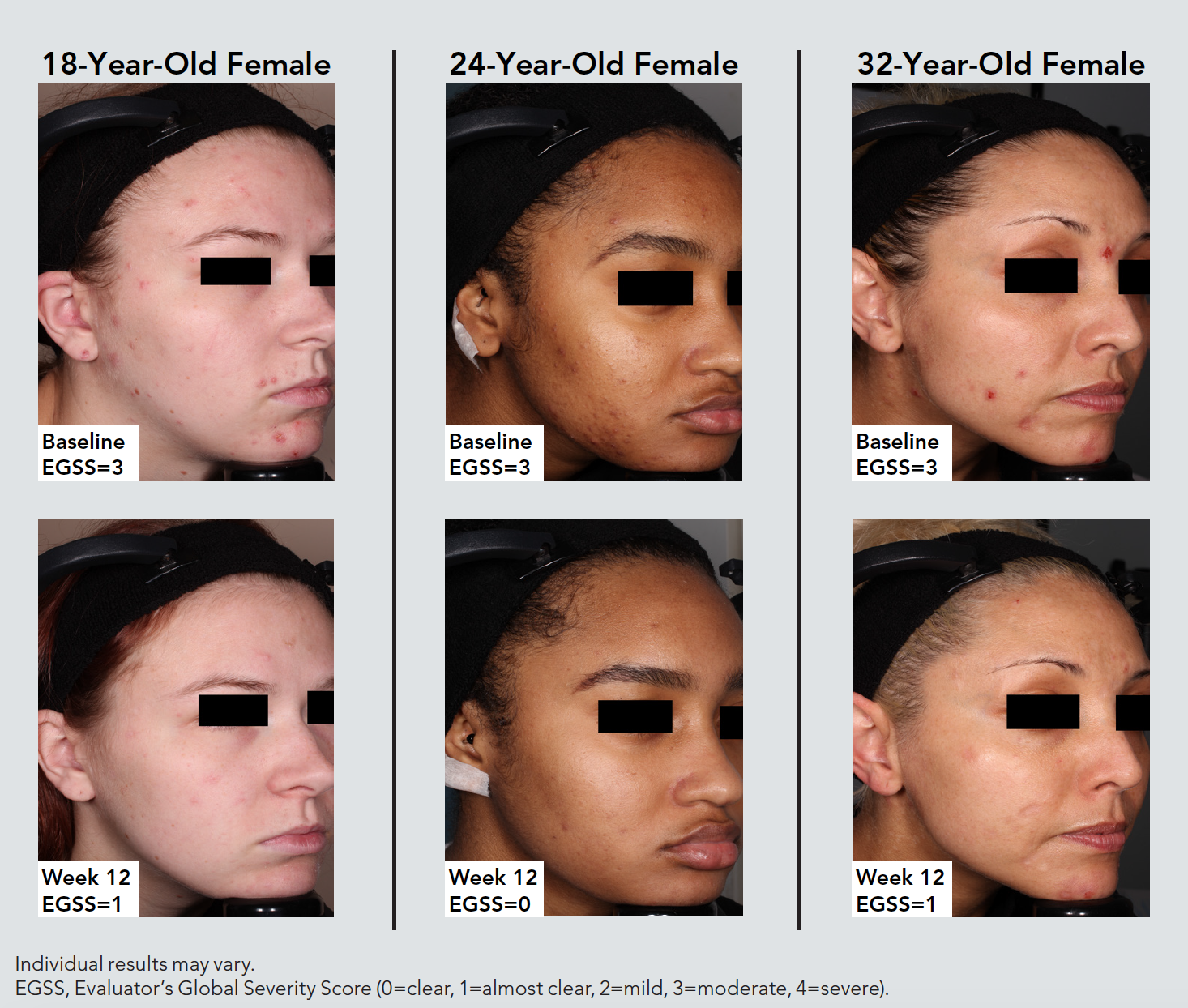
The FDA-approved narrow-spectrum antibiotic sarecycline was safe, well-tolerated, and effective for moderate to severe inflammatory acne vulgaris in patients 9 years old and older
-
- Significant reduction in inflammatory lesions as early as 3 weeks
- Significant improvement in truncal acne (chest and back) was reported
- Significant improvement on comedonal acne was reported as well
- Incidence of side effects commonly associated with tetracycline-class antibiotics was low (<5%)
View the full scientific poster here.
_____________________________________________________________________
 Efficacy and Safety of Tazarotene 0.045% Lotion in Female Patients with Moderate to Severe Acne: Post Hoc Analysis by Age
Efficacy and Safety of Tazarotene 0.045% Lotion in Female Patients with Moderate to Severe Acne: Post Hoc Analysis by Age
Linda Stein Gold, MD; Hilary Baldwin, MD; Fran Cook-Bolden, MD; Lawrence Green, MD; Glynis Ablon, MD; Neil Sadick, MD; Jonathan Weiss, MD; Eric Guenin, PharmD, PhD, MPH
Synopsis
-
- Acne is common among adolescents, occurring in 85% of this population¹
- The overall prevalence of acne tends to decrease with age; however, acne can persist throughout adulthood, more often in females than males2,3
- In addition, older age and female sex are associated with greater negative impacts on quality of life4
- The first lotion formulation of tazarotene 0.045%, developed using a novel polymeric emulsion technology, was efficacious and well-tolerated in two phase 3 studies of patients ≥9 years of age with moderate-to-severe acne (NCT03168334 and NCT03168321)5
Conclusions
-
- Treatment with tazarotene 0.045% lotion reduced inflammatory and noninflammatory lesions by approximately 55–60% in adolescent and adult females with moderate-to-severe acne
- No age-related trends for safety/tolerability were observed; erythema and hyperpigmentation remained relatively unchanged or improved with tazarotene 0.045% lotion
References
-
- Zaenglein AL, et al. J Am Acad Dermatol. 2016;74(5):945-973.e933.
- Skroza N, et al. J Clin Aesthet Dermatol. 2018;11(1):21-25.
- Collier CN, et al. J Am Acad Dermatol. 2008;58(1):56-59.
- Tan JK, et al. J Cutan Med Surg. 2008;12(5):235-242.
- Tanghetti EA et al. J Drugs Dermatol. 2020;19(3):272-279.
View the full scientific poster here.
_____________________________________________________________________
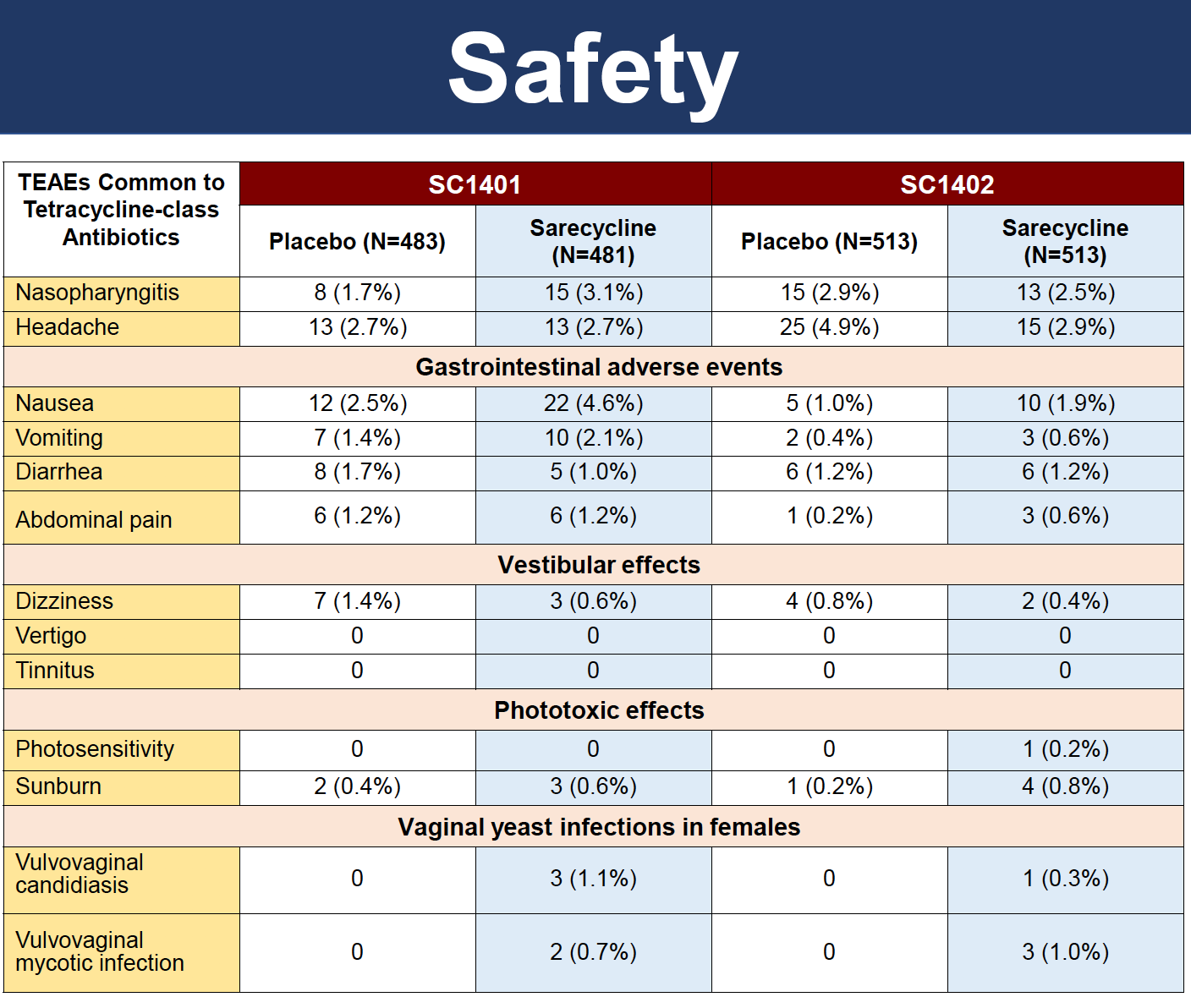
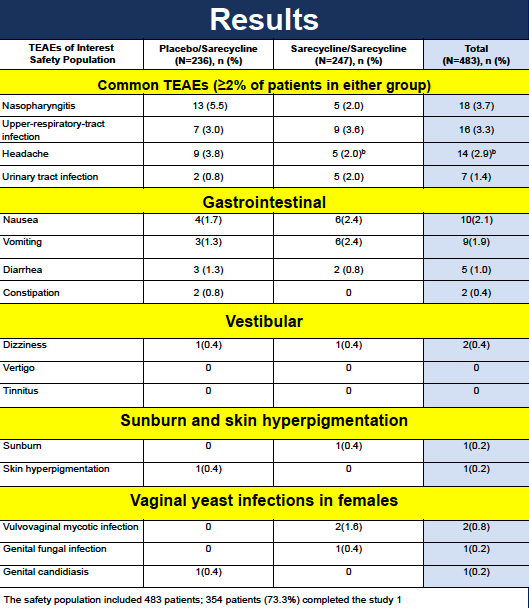
 Long-term Safety and Tolerability of Sarecycline for the Treatment of Acne Vulgaris: Results from a Phase III, Multicenter, Open-Label Study and a Phase I Phototoxicity Study
Long-term Safety and Tolerability of Sarecycline for the Treatment of Acne Vulgaris: Results from a Phase III, Multicenter, Open-Label Study and a Phase I Phototoxicity Study
David M. Pariser, MD; Lawrence J. Green, MD; Edward L. Lain, MD; Jodi L. Johnson, MD; Ayman Grada, MD
Introduction
-
- Sarecycline is a narrow-spectrum tetracycline-class antibiotic designed for the treatment of moderate-to-severe acne.
- Sarecycline’s narrow-spectrum anti-bacterial activity and lipophilicity may minimize side effects commonly associated with broad-spectrum tetracyclines, such as minocycline and doxycycline.
- Pariser DM, MD et. al report the results of 2 identically designed, phase 3 pivotal trials, SC1401 and SC1402, to evaluate the efficacy and safety of once-daily sarecycline (n=2002).
Conclusion
-
- Sarecycline was associated with low rates of TEAEs, with nasopharyngitis, upper-respiratory-tract infection, headache, and nausea being the only TEAEs reported ≥2% or more of patients with moderate-to-severe acne vulgaris aged nine years or older treated with sarecycline once daily for up to 40 weeks.
- Rates of TEAEs commonly associated with other tetracycline antibiotics were for dizziness (0.4%) and sunburn (0.2%), and for gastrointestinal TEAEs, nausea (2.1%), vomiting (1.9%), and diarrhea (1.0%). Vulvovaginal mycotic infection (0.8%).
- Sarecycline has low potential to cause clinically significant phototoxicity
- No clinically meaningful safety findings were noted.
View the full scientific poster here.
_____________________________________________________________________
 Oral Sarecycline for Treatment of Papulopustular Rosacea: Results of a Pilot Sudy Evaluation of Effectiveness and Safety
Oral Sarecycline for Treatment of Papulopustular Rosacea: Results of a Pilot Sudy Evaluation of Effectiveness and Safety
By James Q. Del Rosso, DO; Leon H. Kircik, MD; Cheryl Effron, MD; Zoe D. Draelos, MD
Introduction
Cutaneous rosacea is a common inflammatory facial dermatosis characterized visibly by persistent central facial erythema, episodic dilation of vasculature (flushing), and telangiectasias, with or without papulopustular lesions and phymas.1,2
Beyond the signs and symptoms of rosacea, the disorder may be stigmatizing, can negatively influence workplace behavior, and has been associated with several adverse psychosocial sequelae.3
Flushing episodes and papulopustular lesions have been reported by patients to be the most bothersome manifestations of rosacea across all severities.4
The second-generation broad spectrum tetracyclines—doxycycline and minocycline—have been commonly used as oral therapies for rosacea over the past several years.5 In 2018, sarecycline (Seysara, Almirall), a third-generation oral tetracycline, was FDA-approved for treatment of acne. It exhibits a narrow spectrum of antibiotic activity and a low rate of adverse effects historically associated with oral tetracyclines, such as photosensitivity, GI side effects, vertigo, and vaginal yeast infections.6
Due to the well-established role for oral tetracyclines in rosacea and the desire to circumvent emergence of antibiotic-resistant bacteria as much as possible, a pilot study was completed to evaluate oral sarecycline in adults with papulopustular rosacea.
Conclusion
Results of this pilot study demonstrate that oral sarecycline is efficacious as early as 4 weeks and safe for the treatment of papulopustular rosacea in adults based on IGA assessments, total inflammatory lesion reductions, SGA outcomes, and safety evaluations.
Notably, this study assesses facial skin signs and symptoms at baseline and throughout the study, and evaluates results with oral therapy only; therefore the noted significant improvements in facial skin manifestations such erythema, dryness, peeling, burning, and pruritus are believed to be reflective of the therapeutic response of rosacea to oral sarecycline.
The type, frequency, and severity of AEs reported in this study are consistent with what has been reported with oral sarecycline in clinical trials completed to date for treatment of acne, including the pivotal studies performed for FDA approval.
The authors suggest additional studies be conducted to further evaluate the use of oral sarecycline for the treatment of rosacea.
References
1. Ahn CS, Huang WW. Dermatol Clin. 2018;36(2):81-86.
2. Del Rosso JQ, Thiboutot D, Gallo R, et al. Cutis. 2013;92(5):234-40.
3. Oussedik E, Boucier M, Tan J. Psychosocial burden and other impacts of rosacea on patient’s quality of life. Dermatol Clin. 2018;36(2):103-113.
4. Harper J, Del Rosso JQ, Ferrusi IL. Cross-sectional survey of the burden of illness of rosacea by erythema severity. J Drugs Dermatol. 2018;17(2):150-158.
5. Del Rosso JQ, Thiboutot D, Gallo R, et al. Cutis. 2014;93:18-28.
6. Moore AY, Charles JEM, Moore S. Future Microbiol. 2019;14(14):1235-1242.
View the full scientific poster here.
_____________________________________________________________________
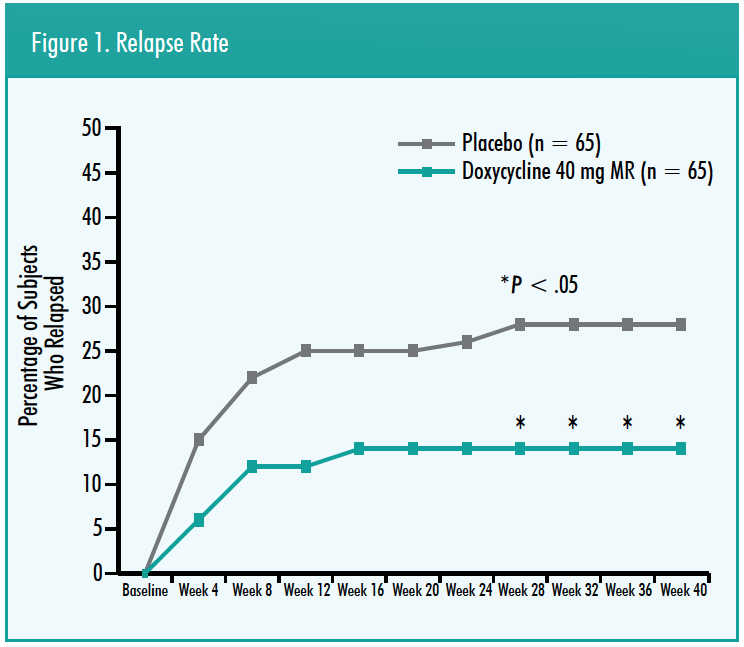
 The Role of Long-Term Doxycycline 40 Mg Modified Release in the Prevention of Disease Relapse in Moderate to Severe Rosacea
The Role of Long-Term Doxycycline 40 Mg Modified Release in the Prevention of Disease Relapse in Moderate to Severe Rosacea
Joshua Berlin, MD; Warren Winkelman, MD, MBA, PhD
Introduction
Approximately 25% of subjects with papulopustular rosacea relapse after discontinuation of systemic therapy suggesting that long-term systemic therapy is required for certain populations.¹ Tetracyclines have utility for longer treatment periods to maintain control, particularly in more severe and recalcitrant rosacea presentations.² Doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads) is a Food and Drug Administration-approved oral therapy indicated to treat the inflammatory lesions of rosacea. A 2-phase, long-term study was conducted to assess the relapse rate, efficacy, and safety of doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads) vs placebo after an initial 12-week combination regimen of doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads) and metronidazole 1% gel in subjects with moderate to severe rosacea. The results of the 40-week phase 2 period are presented here.
Summary
-
- Doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads) treatment over 40 weeks in moderate to severe rosacea subjects successfully treated with 12 weeks of combination doxycycline 40 mg MR with metronidazole 1% gel resulted in a statistically significant reduction in relapse rate.
- Relapse rate with doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads) was 14%, compared to 28% for placebo
- The placebo rate was similar to the relapse rate to tetracyclines (25%) quoted in the literature.¹
- No new safety or tolerability signals were noted in continuous use over 40 weeks of doxycycline 40 mg (30 mg immediate-release, 10 mg delayed-release beads).
References
1. Powell FC. Clinical practice. Rosacea. N Engl J Med. 2005;352(8):793-803.
2. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. May 2005;19(3):273-285.
View the full scientific poster here.
_____________________________________________________________________
 Understanding Concerns and Expectations of Acne Respondents to Improve Management of the Disease: Results of Two Large, Online Surveys In The United States Of America
Understanding Concerns and Expectations of Acne Respondents to Improve Management of the Disease: Results of Two Large, Online Surveys In The United States Of America
Jerry Tan, MD; Anna L Chien, MD; JP York, Ph3; Alison M Layton, MD
Introduction
-
- Acne is a common chronic disease fraught with public misconceptions about causes and treatments.
- Understanding the patient’s experiences and expectations may help highlight shortcomings; however, there is a paucity of such information from those with acne.¹
Results
Survey Populations
-
- Demographics and acne data of the acne respondents (AcnePop) and general population respondents (GenPop)
General Perceptions About Acne
-
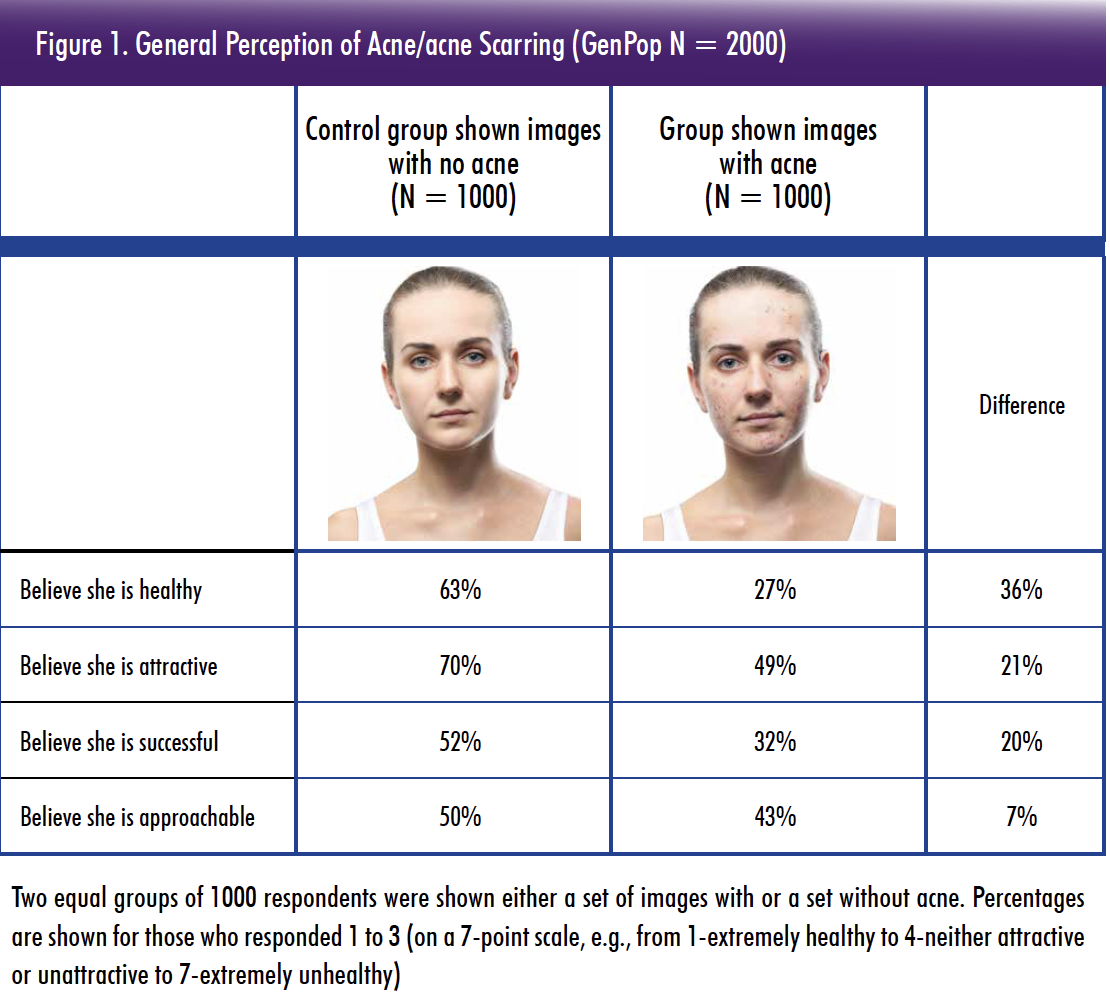
- When GenPop were shown images of people with acne/acne scarring, they were perceived as less healthy, less attractive, less successful, and less approachable than images without acne (Figure 1)
- Furthermore, 24% of GenPop indicated they believed that people with acne have poor hygiene
Burden of Acne
-
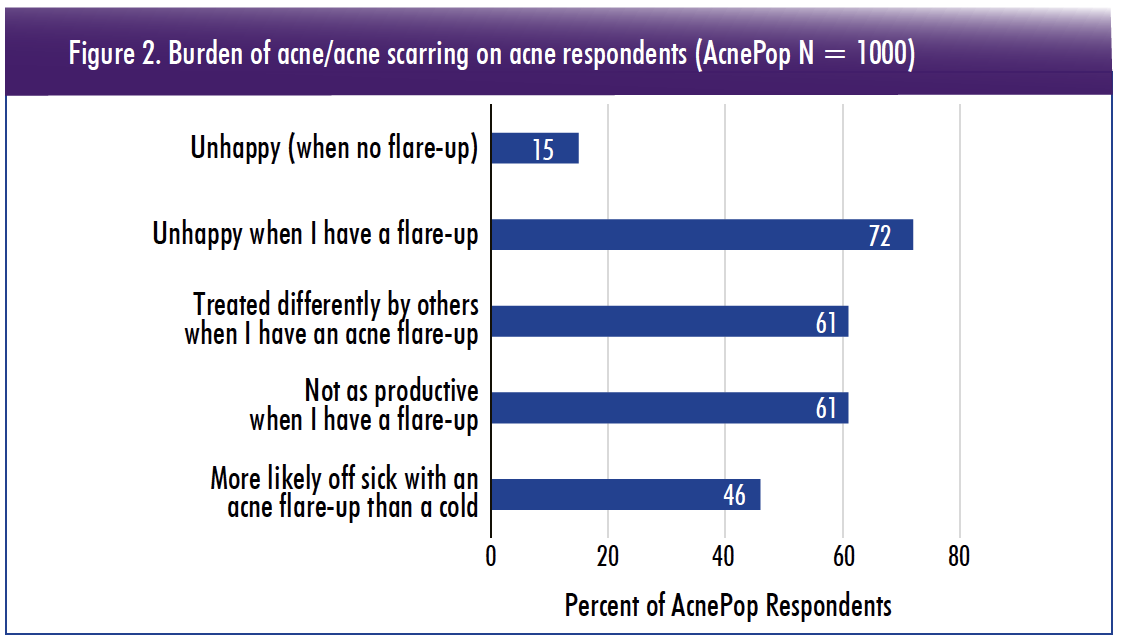
- Around half of AcnePop (46%) indicated they were more likely to take sick leave for an acne flare-up than a cold
- Almost two-thirds of AcnePop (61%) felt they were less productive at work or school during a flare (Figure 2)
Professional Help Received by Acne patients
-
- The vast majority of AcnePop (92%) reported having received unsolicited advice and 39% of GenPop admitted they have given people with acne unsolicited advice at least once.
- Of GenPop (n = 781) who had given unsolicited advice to people with acne, the most common suggestion was to see a doctor (47%).
- Overall, 26% of AcnePop had never consulted a healthcare professional and 36% never received prescriptions for acne/acne scarring (Figure 3a).
- Of those who had seen a medical professional for their acne/acne scarrin
- 72% had consulted a dermatologist
- 45% a primary care physician
- 23% a therapist/psychiatrist (Figure 3b)
Information Gaps
-
- The vast majority (94%) were dissatisfied with information they received from the healthcare provider.
- The main topics they desired more information on were:
- available treatment options (46%)
- how different skin types are affected by acne (44%)
- acne triggers (44%)
- establishing their acne severity (43%) (Figure 4)
References
1. Tan, J. K., K. Vasey, and K. Y. Fung. 2001. ‘Beliefs and perceptions of patients with acne’, J Am Acad Dermatol, 44: 439-45.
View the full scientific poster here.