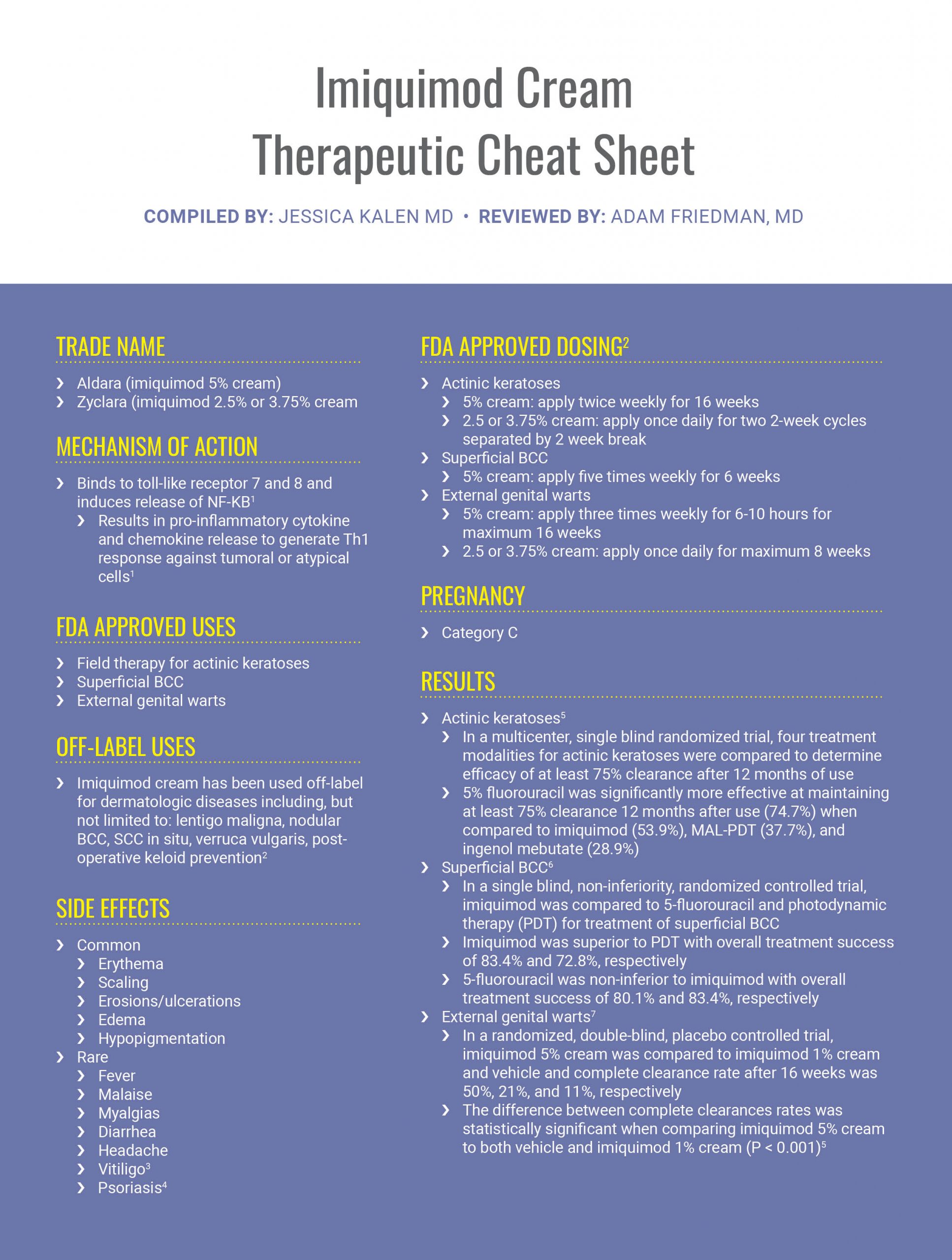
In this month’s installment of our Therapeutic Cheat Sheet Series, we will review the topical immunomodulatory agent imiquimod. Originally approved for the treatment of external genital warts, FDA approval has expanded to include use as field therapy for actinic keratoses as well as treatment of superficial basal cell carcinomas. Here’s what you need to know about imiquimod.
Further Reading
If you would like to read more about imiquimod cream, below are 3 articles published in the Journal of Drugs in Dermatology.
 Real-World Effectiveness and Safety of Field- and Lesion-Directed Treatments for Actinic Keratosis
Real-World Effectiveness and Safety of Field- and Lesion-Directed Treatments for Actinic Keratosis
Background: Real-world data for actinic keratosis treatment in the United States is lacking.
Objectives: To understand real-world treatment patterns for actinic keratosis by type and modality, and compare effectiveness and safety of therapies, either alone or in combination.
Methods: Medical charts of 429 patients were identified; clinical and outcome data were analyzed.
Results: The first treatment after the index diagnosis was most frequently a procedure, followed by a topical agent. Treatment with 5-fluorouracil, ingenol mebutate, imiquimod, cryotherapy, or cryotherapy plus one topical (CRYO+One Topical) reduced actinic keratoses by 66.0%, 69.3%, 72.5%, 72.9%, and 73.0%, respectively; ≥75% clearance (AKCLEAR 75) was achieved in 57.1%, 72.7%, 57.1%, 62.4%, and 62.0% of those patients. Treatment effectiveness was positively correlated with the number of baseline actinic keratoses for topical and for procedural plus topical combination treatments, but not for procedural treatments alone. Adverse reactions (ARs) were more common with cryotherapy (9.7%); local skin responses (LSRs) were more common with field-directed (18.5%-43.1%) and CRYO+One Topical therapy (21.3%).
Limitations: This was a retrospective study of limited duration and population size.
Conclusions: The most commonly used treatments for patients with 6 or more actinic keratoses were topicals and a procedure plus topical combination, which also achieved higher rates of complete clearance than a procedure alone. ARs and LSRs were few in frequency and type. J Drugs Dermatol. 2020;19(8):756-762. doi:10.36849/JDD.2020.5123
 Imiquimod 2.5% and 3.75% for the Treatment of Actinic Keratoses: Two Phase 3, Multicenter, Randomized, Double-Blind, Placebo-Controlled Studies
Imiquimod 2.5% and 3.75% for the Treatment of Actinic Keratoses: Two Phase 3, Multicenter, Randomized, Double-Blind, Placebo-Controlled Studies
Background: Imiquimod 3.75% and 2.5% creams were studied for the treatment of actinic keratosis (AK) of the full face or balding scalp, to determine comparable efficacy and tolerability to imiquimod 5% cream.
Methods: In two identical multicenter, randomized, double-blind, placebo controlled studies. Adult subjects with 5 to 20 visible lesions, or palpable AKs in an area that exceeded 25cm2 on either the face or balding scalp were randomized to imiquimod 3.75%, 2.5% or vehicle cream (1:1:1) applied once daily for two 2-week treatment cycles, with a 2-week, no-treatment interval between cycles. Efficacy was assessed 8 weeks posttreatment (End of Study Visit [EOS]). Primary efficacy was rate of complete clearance of AK lesions. Secondary efficacy endpoints were rate of partial clearance at EOS (≥ 75% reduction in number of AK lesions compared to baseline) and median percent decrease from baseline lesion count. Safety assessments included visual assessment of local skin reactions (LSRs), number and duration of study treatment rest periods required due to intolerant LSRs, adverse events (AEs) and clinical laboratory tests.
Results: Overall 479 patients were randomized to imiquimod 3.75%, 2.5%, or vehicle. Complete clearance rates were 35.6%, 30.6%, and 6.3% respectively (both P<.001 versus vehicle). The difference in complete clearance rates (imiquimod minus vehicle) was 29.3% and 24.3%, respectively. Partial clearance rates were 59.4%, 48.1%, and 22.6% respectively (both P<.001 versus vehicle). Median % reductions in AK lesions were 81.8%, 71.8%, and 25.0% respectively (P<.001 versus vehicle). All primary and secondary efficacy endpoints were greater in Study 1. Photodamage in the treatment area was ‘much improved’ with imiquimod 3.75%. Both active creams were well tolerated with few treatment-related discontinuations.
Conclusions: In two well-controlled Phase 3 studies, both imiquimod 3.75% and 2.5% creams were more effective than vehicle and well-tolerated when administered daily as a 2-week on/off/on regimen to treat AK. Reduction in AK lesions was comparable to that reported with imiquimod 5% with fewer local AEs.
 Subungual Melanoma In Situ Treated With Imiquimod 5% Cream After Conservative Surgery Recurrence
Subungual Melanoma In Situ Treated With Imiquimod 5% Cream After Conservative Surgery Recurrence
Subungual melanoma is a rare variant of acral lentiginous melanoma that often has a poor prognosis compared with other types of melanoma. The aim of the present study is to report a case of a patient with recurrence of subungual melanoma treated with imiquimod 5%, which presented a total regression of the lesion and no recurrence for 4 years.
References
-
- Schön MP, Schön M. Imiquimod: mode of action. Br J Dermatol. 2007;157(Suppl. 2):8-13
- Bolognia JK, Scahher JV, Cerroni L. Dermatology. Philadelphia: Elsevier. 2018
- Zhu W, Zhang R. Genital vitiligo following use of imiquimod 5% cream. Indian J Dermatol. 2011 May-Jun;56(3):335-336.
- Patel U, Mark NM, Machler BC, Levine VJ. Imiquimod 5% cream induced psoriasis: a case report, summary of the literature and mechanism. Br J Dermatol.
- Jansen MH, Kessels JP, Nelemans PJ. Randomized trial of four treatment approaches for actinic keratosis. N Engl J Med. 2019;380:935-946.
- Arits AH, Mosterd K, Essers BA, et al. Photodynamic therapy versus topical imiquimod of superficial basal-cell carcinoma: a single-blind, non-inferiority, randomized controlled trial. Lancet Oncol. 2013 Jun;14(7):647-54.
- Edwards L, Ferenczy A, Eron L, et al. Self-administered topical 5% imiquimod cream for external anogenital warts. Arch Dermatol. 1998 Jan;134;25-30.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.

