Just as hair types often differ among different ethnicities, the prevalence and presentation of dermatological diseases affecting the hair and scalp can also be diverse. These are attributed to innate hair shaft differences, hair styling practices, genetic influence, and inflammatory co-morbidities. Differentiating scarring alopecia from other types of hair loss is especially critical in developing a treatment plan to target the underlying pathology.
At the 2020 Skin of Color Virtual Update, Dr. Amy McMichael discussed Hair & Scalp Disorders in SOC: Diagnostic Approaches. Her lecture reviewed common scalp and hair concerns, and how best to diagnose these diseases, highlighting unique concerns to patients with pigmented skin. As hair and scalp concerns are in the top ten most common reasons African American patients visit a dermatologist, Dr. McMichael discussed the importance of being proficient in diagnosing these disorders.
Causes of hair fragility
One of the most common hair complaints among patients with skin of color is increased hair fragility, presenting itself as poor growth and increased fragmenting. So what contributes to this increased fragility? Let’s review Dr. McMichael’s main points:
-
- Trichorrhexis nodosum (TN) is an innate hair fragility seen in African American patients. This defect in the hair can be congenital or acquired and is characterized by thickening or weak points (nodes) that cause the hair to break off easily. TN is not a disorder of trichothiodystrophy, meaning there is no disruption of cysteine-rich proteins in the hair. Hair practices, however, can exacerbate this innate fragility. It is important to discuss washing, brushing, and styling practices with your patient!
- The hair shafts are smaller in diameter in African American hair compared to Caucasian women. African Americans also have decreased hair counts in a standard area of the scalp and slower growing hair.
- Up to 55% of black women experience hair shaft breakage with normal styling.
- In one study African American women were noted to have significantly increased broken hairs compared to Caucasian women in a 60-second comb test. Further, black women were 3.5 times more likely to experience hair breakage than Caucasian women.
- Up to 40% of African American women reported exercise avoidance due to hair related issues.
- In survey studies, 60% of African American women report their hair type as dry, whereas 67% of Caucasian women report normal hair type. Further, black women were 10 times more likely to want to change hair dryness.
- Increased hair fragility or breakage may present from different causes, including early central centrifugal cicatricial alopecia or after chemical damage.
Is all chemical processing equally damaging to the hair? No, explains Dr. McMichael. Chemical straightening is the most likely to cause catastrophic damage to the hair because it removes the mono-molecular layer of fatty acids bonded to the cuticle. Hair dye is much less likely to be catastrophic, however, repeat treatments have a cumulative effect to damage the hair shaft. Bleach and permanent colorants are most damaging, whereas semi-permanent and temporary dyes are the least. Thermal straightening can also cause hair shaft weakening, with flat irons and curling irons being more damaging than blow dryers.
Here is the approach Dr. McMichael recommends for a patient complaining of increased hair breakage:
-
- Evaluate for underlying abnormalities (e.g., iron levels, thyroid function, nutrition status)
- Recommend to give the hair a rest! Protective practices including stopping any chemical relaxer or dye for 6-12 months, placing the hair in a weave that is not tight and will allow for hair treatment (e.g., loose braids, a wig, or natural hair), and avoidance of heat straightening.
- Recommend serial trimming of the hair every 6-8 weeks.
- Recommend to use heat protectant products before any styling.
- Recommend layering moisturizing regimen: start with a moisturizing shampoo and conditioner specifically for dry and damaged hair, add a leave-in-conditioner with coating agents to the wet hair; and finish with a leave-in-conditioner (e.g., oils) to dry hair. Such oils can be applied after washing and then daily as needed.
- Advise it is a long wait to see improvement!
Inflammatory scalp diseases
Inflammatory scalp conditions and their associated hair loss are another common concern among African American patients. Dr. McMichael reviewed the four most common conditions, including seborrheic dermatitis, traction alopecia, central centrifugal cicatricial alopecia (CCCA), and frontal fibrosing alopecia, and how these disease present in the patient with pigmented skin.
Seborrheic dermatitis is a common inflammatory scalp disorder dermatologists see in their offices on a daily basis. Among African American patients, it is the third most common diagnosis during dermatology encounters according to a national database study. With high costs of healthcare use and significant quality of life impact due to this disease, Dr. McMichael noted it is remarkable that there is very little literature about seborrheic dermatitis in this patient population. Clinical features of seborrheic dermatitis in pigmented skin types include:
-
- Hypopigmented and hyperpigmented patches and petaloid plaques on the peripheral face
- Decreased hair density at the frontal hairline and localized telogen effluvium.
- There may be associated folliculitis
- The scalp may be significantly pruritic
- Can be complicated by lichen simplex chronicus and hair shaft breakage
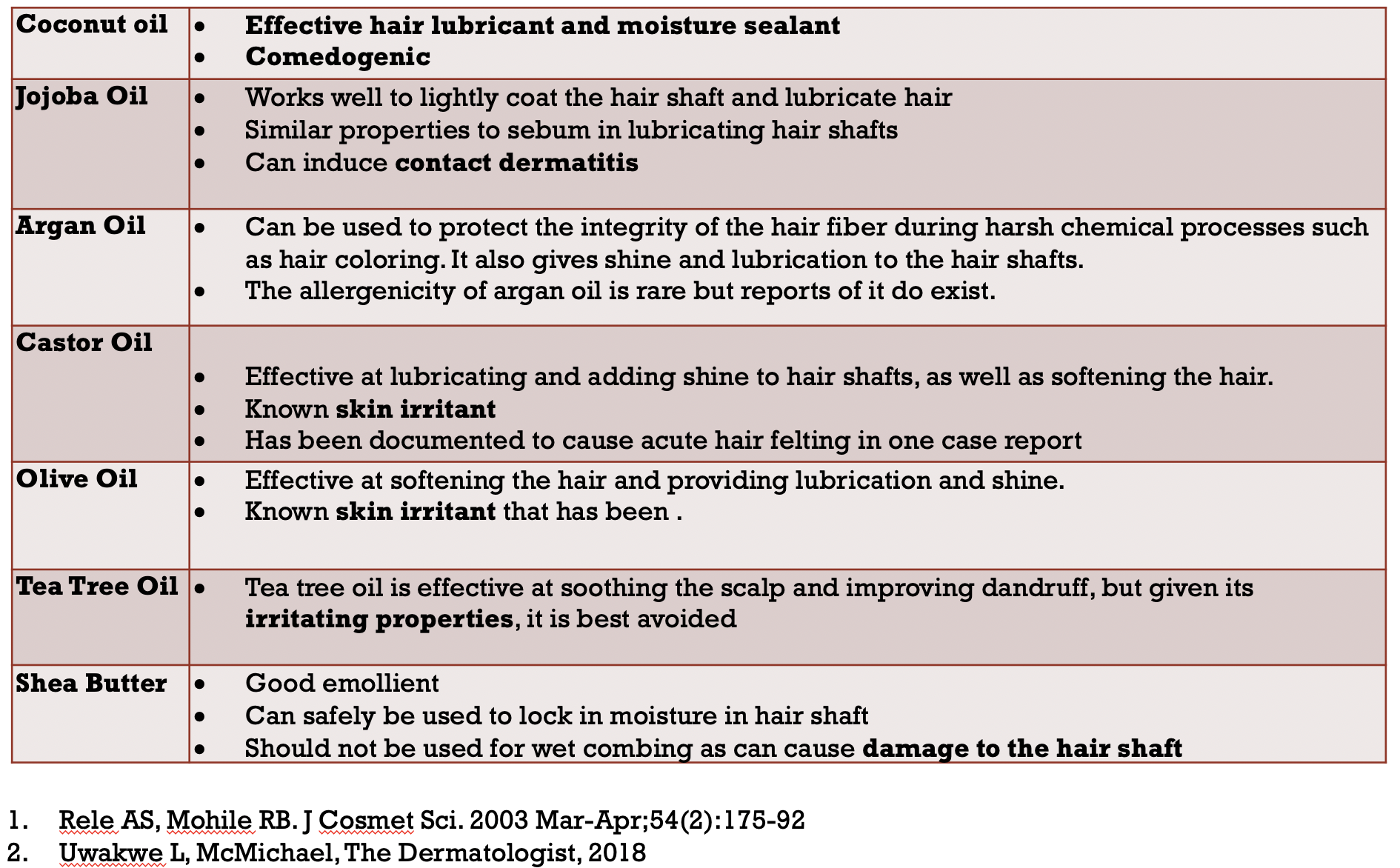
What causes seborrheic dermatitis? The exact mechanism is not known. However, there are multiple theories with proposed roles for lipase activity in the sebaceous glands, individual susceptivity to toll-like-receptors, absent or decreased desmosomes causing flaking, infiltration with Malassezia, and cytokine dysregulation. Further, some hair practices can complicate this disease, including infrequent hair washing and inappropriate use of hair care oils and pomades. While oils are a necessary part of the care of coiled hair types, some oils can have negative side effects. Dr. McMichael noted coconut and argan oils are generally well tolerated. On the other hand, jojoba oil can induce allergic contact dermatitis, and castor, olive, and tea tree oils can be irritating to the scalp. Shea butter serves as a good emollient, but it should not be used for wet combing because it can cause damage to the hair shaft.
Traction alopecia is another commonly seen inflammatory alopecia of high prevalence in women and girls of African descent. The mechanism of traction alopecia is thought to be due to chronic mechanical tension on the hair shaft, such as tight braids. However, chemical processing of the hair increases the risk of traction alopecia. More than 80% of patients with traction alopecia have experienced pain with hairstyles. In traction alopecia, recession of the frontal hairline with the fringe sign is seen clinically. Dermoscopy features include perifollicular, hyperpigmented macules, miniaturized hairs, and preserved marks of follicular openings outlined in brown pigmentation.
When evaluating alopecia of the frontal hairline, Dr. McMichael advises it is important to consider frontal fibrosing alopecia (FFA) in the differential diagnosis. FFA is a variant of lichen planopilaris, and its incidence has been increasing dramatically in all ethnicities. These are the key features of FFA:
-
- Clinically there is complete hair loss on the frontal scalp with the lonely hair sign and associated eyebrow loss. There may also be atrophy of the frontal scalp.
- Perifollicular erythema with hyperkeratosis can be seen in areas of active disease.
- Dermoscopy features include hypopigmented macula and hyperkeratotic plaques with erythema around the hair shafts.
- Associated lichen planus pigmentosus is seen in pigmented skin types.
- There is no evidence of sunscreen use causing FFA. Mineral sunscreen use should be encouraged.
To close out the review of inflammatory hair diseases in pigmented skin types, Dr. McMichael highlighted central centrifugal cicatricial alopecia (CCCA). CCCA has gained attention recently due to increasing prevalence, frequently referred to as an epidemic among African American women. CCCA poses a diagnostic challenge because the clinical presentation can vary significantly, especially early in the disease. Here are some highlights about CCCA:
-
- The prevalence of CCCA varies from 2.7% in South African women to 5.6% in the United S
- There is a wide range in clinical severity as well as symptom burden, from asymptomatic to severe pain and pruritus.
- CCCA is most prevalent in women of African descent, ages 30-65.
- CCCA predates chemical relaxer use. However, traction may play a role. There is a strong association with extensions, sewn-in hair weaves, cornrow, and braided styles. Patients with CCCA often have accompanying traction alopecia.
- Breakage at the vertex scalp can be an early sign of CCCA.
- Scarring hair loss of the vertex is the most common presentation of CCCA. However, it can also affect the frontal scalp. There is also a patchy and progressive form of CCCA.
- Dermoscopy features include perifollicular scale and erythema during active disease, miniaturization of hair shafts during early disease, and significant loss of follicular openings associated with burnt out disease. The miniaturized hairs still have potential for regrowth.
- Dermoscopy can be a useful tool to identify extent of active disease. Features of activity can be observed up to four centimeters away from areas of clinical disease and have been confirmed by features of CCCA on histology.
- Women with CCCA are five times more likely to have uterine leiomyomas suggesting an underlying fibrosing disorder.
- There is an association with insulin resistance. There is an increased risk of diabetes mellitus in women with CCCA; inversely, women with diabetes for greater than 10 years are at increased risk of CCCA. Positive response to topical metformin is further support of this association.
- Recently a genetic cause of CCCA was identified with the discovery of an autosomal dominant pattern of inheritance of the peptidyl arginine deiminase, type III (PADI3) gene in black South Africans. Dr. McMichael, one of the authors of this groundbreaking study, described how a missense mutation in this enzyme that is essential for post-translation modification of protein required for hair-shaft formation contributes to familial CCCA.
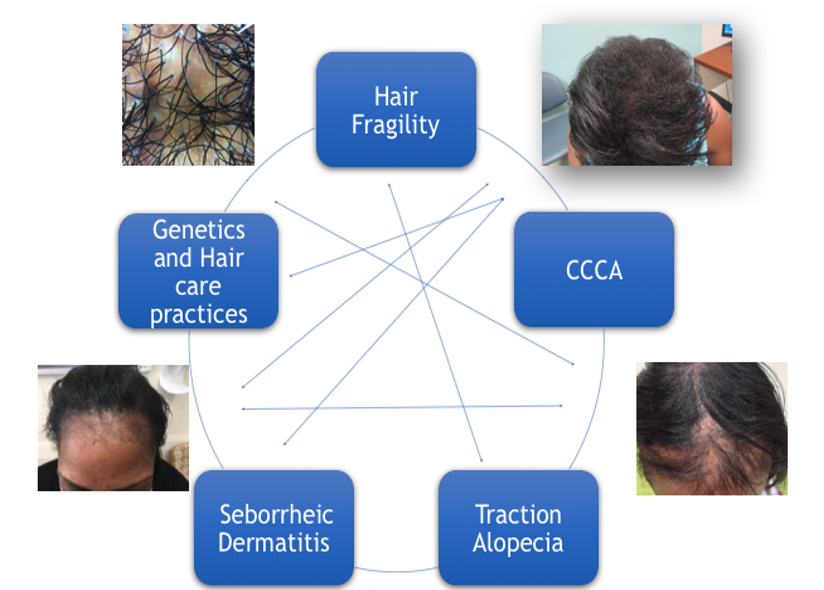
The hair loss and scalp symptoms experienced by patients with pigmented skin are caused by a mix of these inflammatory scalp disease and innate fragility of the hair. It is critical to identify the subtle clinical features of these diseases to lead to the correct diagnosis.
This information was presented by Dr. Amy McMichael during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Dr. Edita Newton.
All images courtesy of Dr. Amy McMichael
Did you enjoy this article? Find more on Skin of Color topics here.

