Atopic dermatitis (AD) is a chronic inflammatory skin disease. The pathogenesis of AD is complex with many mediators involved and can be broken down into 4 categories:
-
- Immune dysregulation
- Abnormal skin barrier
- Abnormal itch/scratch cycle
- Abnormal skin microbiome
In AD, there is a breakdown in molecular control of the immune system, leading to overproduction and expression of pro-inflammatory cytokines. Patients with AD have a mutation in the filaggrin gene (FLG) causing abnormal skin barrier function and an early or severe presentation of disease. In addition, environmental and external triggers can influence and change how an individual’s genes are expressed.
Our skin barrier helps to maintain skin hydration and prevent infections. In those with AD, skin barrier dysfunction leads to water loss and entry of immunogens, which propagates the itch/scratch cycle.
Finally, our skin contains commensal microorganisms that inhibit colonization of foreign pathogens, maintain the pH balance of the skin and inhibits inflammation. In AD, there is dysbiosis or an imbalance between good and bad bacteria on skin surface. This leads to increased infections due to increased S. aureus colonization.
Let’s review the most recent guidelines for AD management:
-
- Baseline therapy – Basic management including patient education, frequent use of emollients, avoidance of allergens
- Mild/Transient disease – Reactive therapy with topical prescription therapies, topical corticosteroids and/or topical calcineurin inhibitors
- Moderate/Recurrent disease – Proactive therapies with more potent topical glucocorticosteroids, wet wrap therapy, UV therapy, psychosomatic counseling
- Severe/Persistent disease – systemic therapies (immunosuppressant, oral corticosteroids, immunomodulators), hospitalization if needed
It is imperative for providers to design and tailor patient-specific treatment plans. We need to develop a toolbox for lifestyle modifications, prescription medications, and complimentary and alternative treatment plans. The goal is an integrative approach with comprehensive care.
The Pillars of AD management include:
-
- Repair the skin barrier
- Reduce/stop inflammation
- Decrease/stop itch
- Restore the microbiome
The goal is to manage all four simultaneously in order to optimize the treatment outcome and decrease disease burden.
Let’s start with skin barrier repair. Healthy skin attracts and retains water and prevents evaporation of water. The skin cells are surrounded by extracellular lipids, and together this forms the skin barrier. The skin barrier prevents entry of irritants, allergens and pathogens.
In AD, the skin barrier is disrupted and the extracellular lipid layer breaks down causing cracks to form. The skin cells shrink, gaps form between them, and water is evaporated from the skin surface. This dry, cracked skin leads to enhanced entry of irritants, allergens and pathogens that cause inflammation and increased itching.
Moisturize early! Recent studies show that early moisturization in infants that are at high risk for AD, those with a first degree relative with AD, can have a protective effect and is associated with a significant decrease in acquiring AD.
Moisturizer Selection and Atopic Dermatitis
There are several valuable ingredients to look for in topical emollient formulations, including essential fatty acids, anti-inflammatory ingredients, and beneficial cold-pressed oils:
-
- Essential Fatty Acids
- Polyunsaturated fatty acids – Linoleic acid
- Sphingolipids – Ceramides
- Anti-microbial lipids – Monolaurin
- Anti-inflammatory ingredients
- Nicotinamide (Niacinamide)
- Glycyrrhetinic acid
- Palmitoylethanlamine (PEA)
- Telmesteine
- Cold-pressed oils
- Coconut oil
- Sunflower seed oil
- Borage seed oil
- Essential Fatty Acids
Let’s highlight a few of these good ingredients. Ceramides are the major building blocks of the skin barrier and deficient in eczema patients. Ceramides are essential in retaining moisture and protecting against environmental irritants. PEA is a cannabinoid-like compound that has been found to have anti-itch properties. Monolaurin is found in coconut oil and has antimicrobial properties against S. aureus , the main organism involved in atopic skin infections. Finally, telmesteine, in addition to anti-inflammatory properties, also exhibits antioxidative properties.
Not all moisturizers are created equally. A recent study published by Thompson AM, et al. (PMID 32844562) showed that 28 out of the 30 top-selling eczema moisturizers were found to contain known allergens. On average, there are 3.6 allergens per product. Eczema products with anti-inflammatory marketing claims have the highest average allergen count. Those with sensitive skin/hypoallergenic marketing claims have significantly lower average allergen count. Choose your moisturizer wisely!
Cannabinoids and their role in Atopic Dermatitis
Cannabinoids are compounds found in cannabis. Ligands for cannabinoid receptors include:
-
- Phytocannabinoids found in plants, eg. tetrahydrocannabinol (THC)
- Synthetic cannabinoids produced in the lab
- Endocannabinoid (EC), eg. PEA
Endocannabinoids are produced by our own body. Our skin has many EC receptors across various cell types (keratinocytes, sebocytes, immune cells and sensory nerves). Therefore, cannabinoids and their receptors play an important role in our skin health and skin physiology, and disruption of this interaction can lead to skin disease.
EC reduce inflammation by inhibiting release of inflammatory mediators from immune cells such as mast cells, which release histamine, nitric oxide, cytokines, & leukotrienes. ECs may decrease itch by reducing axonal reflex development in cutaneous nerve fibers.
There are a number of studies that have looked at topical cannabinoids. Eberlein B, et al. showed that topical PEA in addition to a mid-potency topical steroid is more effective in improving AD compared to topical steroid alone (PMID 18181976). Anti-inflammatory efficacy of topical cannabinoids are comparable to hydrocortisone 1% cream. Topical cannabinoids decrease symptoms of atopic dermatitis such as dryness, itch, scratching, skin thickness, scaling and redness, and improve quality of sleep.
In a RCT, split-body trial of 25 children and 18 adults with AD (Del Rosso JQ, Cosmetic Derm. 2007 Vol 20 (4), it was demonstrated that the combination of PEA-containing emollient with topical corticosteroid twice daily for 6 weeks resulted in faster AD clearance when compared to moisturizer and topical corticosteroid. Additionally, the PEA-containing emollient prolonged the mean time to flare by 28 days compared to moisturizer.
The ATOPA study by Eberlein B, et al. is the largest multinational, multi-center, observational, non-controlled, prospective cohort study assessing the effectiveness of a PEA-containing emollient in atopic patients. There was a total of 2456 patients enrolled in the study, including 923 children up to 12 years old. The patients applied a PEA-containing emollient for 4-6 weeks. The study showed substantial relief of objective and subjective symptoms of atopic eczema after regular skin care with a PEA-containing emollient. Patients reported a progressive decrease in itch, as well as a decrease need to apply topical corticosteroids.
Skin Dysbiosis in Atopic Dermatitis
There is an imbalance of pathogenic bacteria and commensal surface bacteria in AD. Atopic patients have an increase of S. aureus, and decrease of commensal flora such as S. epidermidis, Corynebacterium and Propionibacterium. The microbiome is intimately associated with the severity of AD. As we develop treatments to target AD, we need to be mindful of how to modulate the skin microbiome.
Myles, IA, et al. performed the first skin bacterial transplant in AD patients (PMID 29720571). This was an open-label phase I/II safety and activity trial with 10 adults and 5 children enrolled. Application of Roseomonas lysate from healthy volunteers onto the skin of AD patients. Preliminary data showed decreased in intensity of eczema severity and itch. Treatment with R. mucosa was associated with decreased topical steroid requirement and S. aureus burden. Decrease in surface S. aureus was demonstrated starting at week 12 and maintained through week 16.
Systemic Treatment Options
Traditionally, immunosuppressant medications have been used to combat severe atopic eczema. These medications work upstream and have effects on multiple immune cells, effecting the body’s ability to fight infection or cancer.
Immunomodulators are targeted therapy focused on a small part of the immune system, leaving the function of the other parts of the immune system intact, eg. ability to fight infections and cancer.
Dupilumab: the biggest game changer in AD
Dupilumab is a human monoclonal antibody against IL-4 receptor alpha. It inhibits IL-4 and IL-13 signaling. It is FDA-approved for moderate-to-severe AD in ages 6 and greater. In clinical trials, dupilumab showed a rapid and sustained decrease in itch, as well as decrease in S. aureus on the skin and increased microbial diversity. Dupilumab is very effective and much safer than immunosuppressants. Notable side effects include conjunctivitis in 14% of patients, although this was not observed in patients with asthma.
There are many other immunomodulatory drugs on the horizon, both systemic and topical.
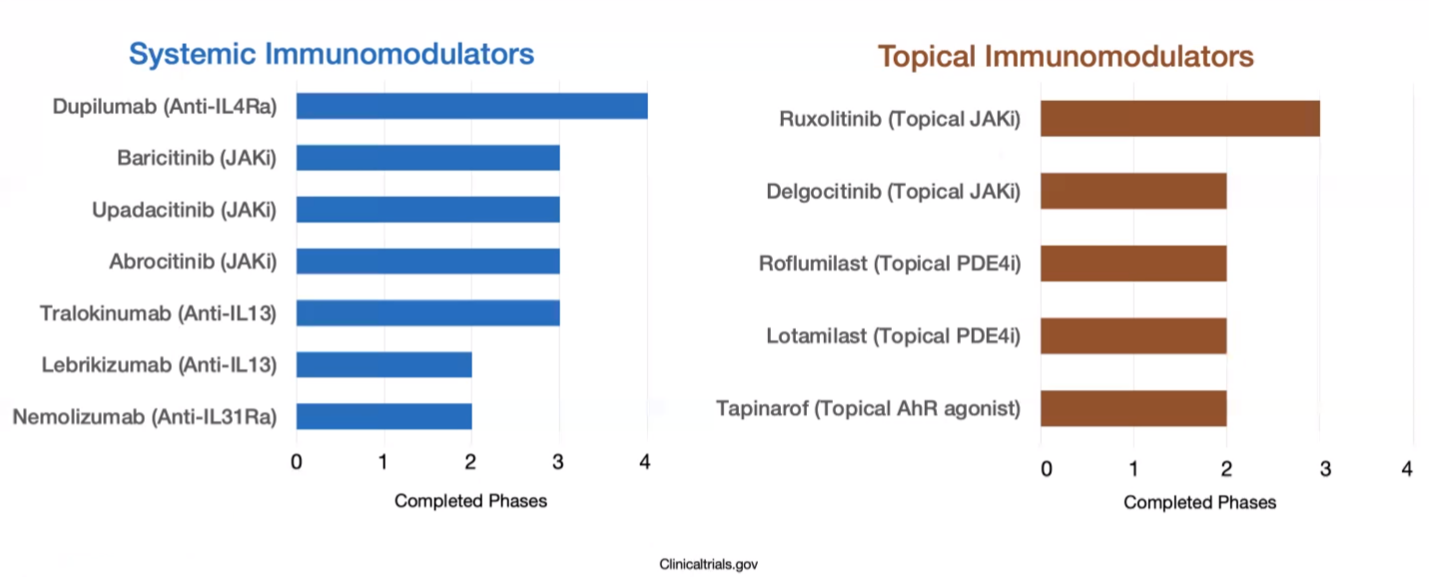 Visit https://www.clinicaltrials.gov/ for more detailed information.
Visit https://www.clinicaltrials.gov/ for more detailed information.
Take home points
-
- There are many mediators involved in the pathogenesis of atopic dermatitis, and therefore many targets for treatment options
- There are complimentary, integrative therapies that enhance treatment response in AD
- Compared to traditional moisturizers, bioactive moisturizers can decrease inflammation and repair oxidative damage.
- The immune system plays a major role in the pathogenesis of AD and novel, targeted immunomodulatory therapies have enhanced therapeutic strategies
The above article was written by Dr. Mojgan Hosseinipour and represents her interpretation of the information presented by Dr. Vivian Shi during her lecture “Novel Therapeutics in Atopic Dermatitis ” at the 2020 Integrative Dermatology Symposium.
Did you enjoy this article? Find more on Integrative Dermatology here.