Have you prescribed low-dose Naltrexone for skin disease? Not sure why it works? Not sure how best to use it, or how to prescribe it? Feel like you could use more information to help you more safely and effectively utilize this medication? I myself utilize this medication for itch but have had mixed success. Enter Dr. Bodemer and her recent lecture.
During the 2020 Integrative Dermatology Symposium, Dr. Apple Bodemer provided a succinct, but impactful, discussion about low-dose Naltrexone (LDN) in her lecture – Low dose Naltrexone in Dermatology.
This review will provide an overview of the talk, including:
-
- A brief discussion of the opioid system in the human body
- Three conditions that are likely to be helped by LDN
- Potential side effects of LDN
Before we get into the full review, here are my “practice barometers” – what I take away from the lecture that may change my practice or confirm my standards:
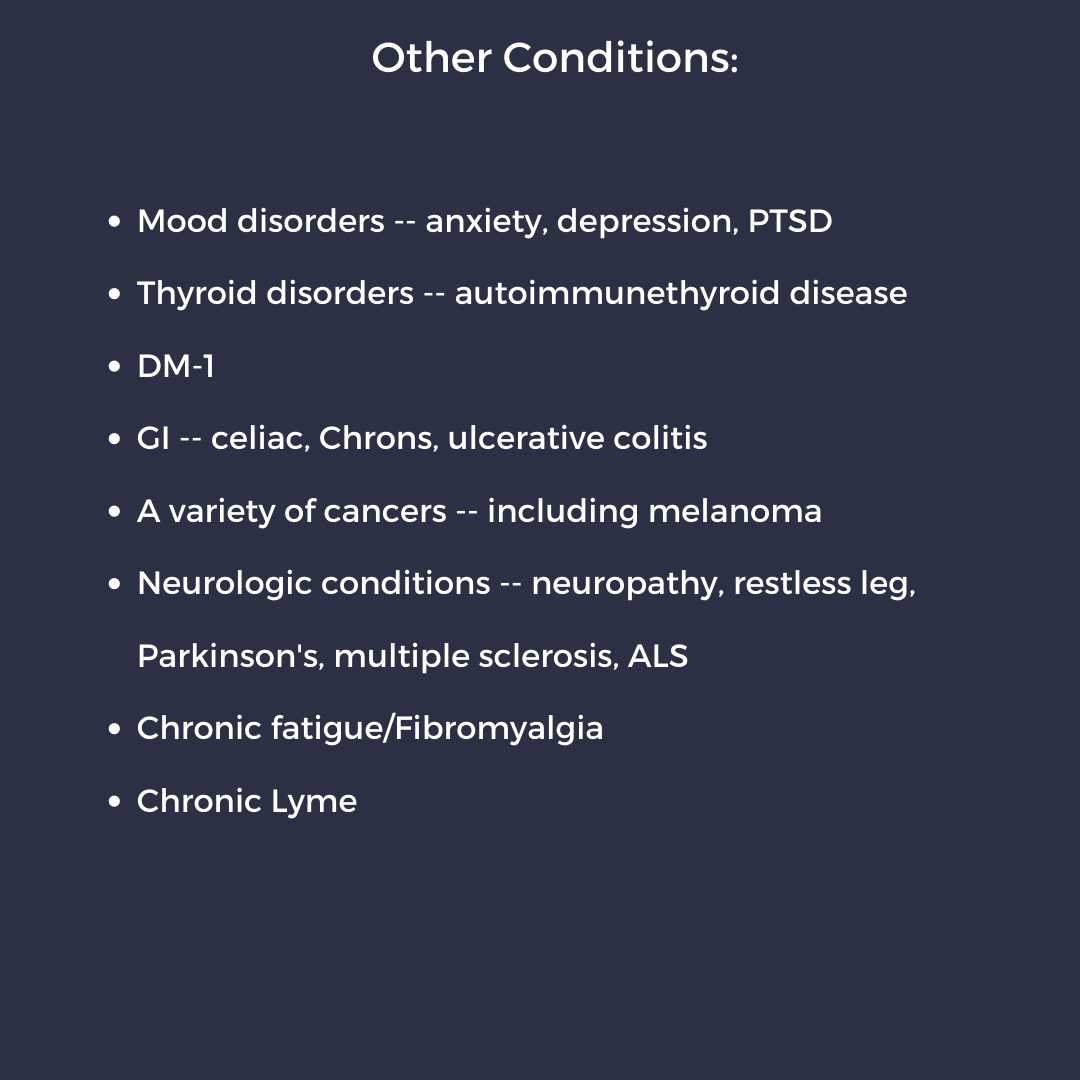
 Low-dose naltrexone has many uses beyond dermatology (Want to help your patient beyond the skin? Read on!)
Low-dose naltrexone has many uses beyond dermatology (Want to help your patient beyond the skin? Read on!)
 Low-dose naltrexone takes time to work – be patient! (How long? The answer is not far away!)
Low-dose naltrexone takes time to work – be patient! (How long? The answer is not far away!)
 I may be using the wrong formulation! (which is likely to be more successful? Hint: sometimes you get what you pay for ☹)
I may be using the wrong formulation! (which is likely to be more successful? Hint: sometimes you get what you pay for ☹)
 Continue to discuss side effects with patients (what side effects? In your dreams…keep reading)
Continue to discuss side effects with patients (what side effects? In your dreams…keep reading)
What is Naltrexone and how does it work?
-
- Opiate antagonist – analog to Naloxone
- FDA approved for – prevention of relapse in opioid addiction (1984) and to treat alcoholism (1994)
- Naltrexone vs Naloxone – both have high affinity for opioid receptor without activity at the receptor
- Naltrexone – metabolized slowly, lasts about one day, takes longer to work
- Naloxone – metabolized quickly, lasts about one hour
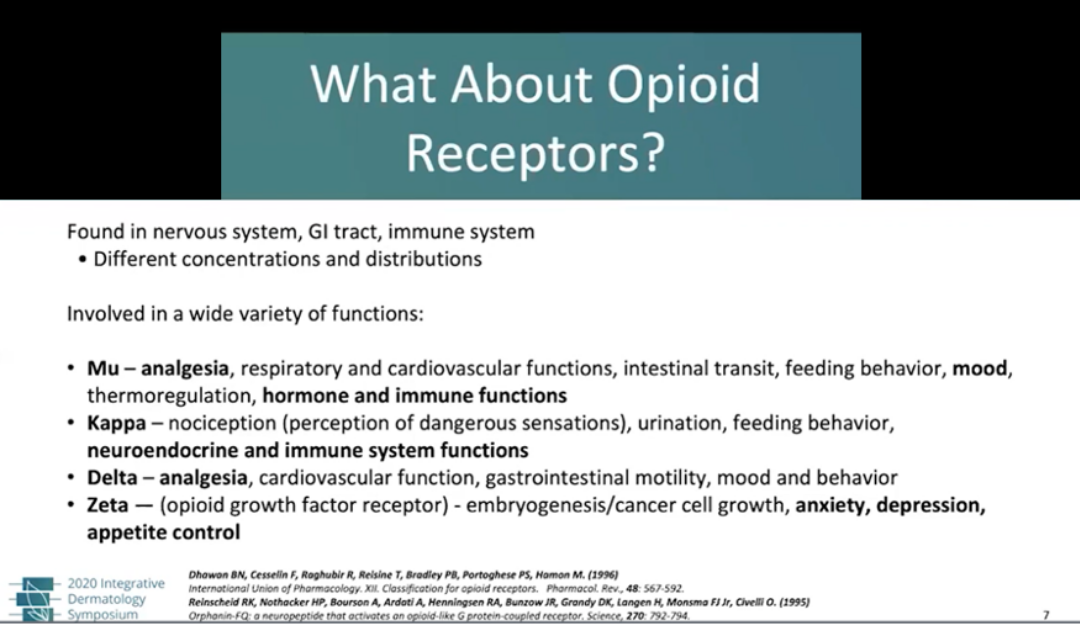
- Opioids have many functions (check out the list below)
- Interestingly opioids are also involved in cell division – by blocking the transition from G1 to S phase
- LDN causes a transient blockade of opioid receptors which leads to increased production of opioids and opioid receptors
- LDN can inhibit TLR4, TLR7, TLR8, and TLR9 – which is the mechanism behind LDNs anti-inflammatory effects
- TLR-4 can activate microglial cells (macrophages of the nervous system)
 Source: 2020 Integrative Dermatology Symposium – “Low dose Naltrexone in Dermatology” by Dr. Apple Bodemer
Source: 2020 Integrative Dermatology Symposium – “Low dose Naltrexone in Dermatology” by Dr. Apple Bodemer
What can LDN be used to treat?
-
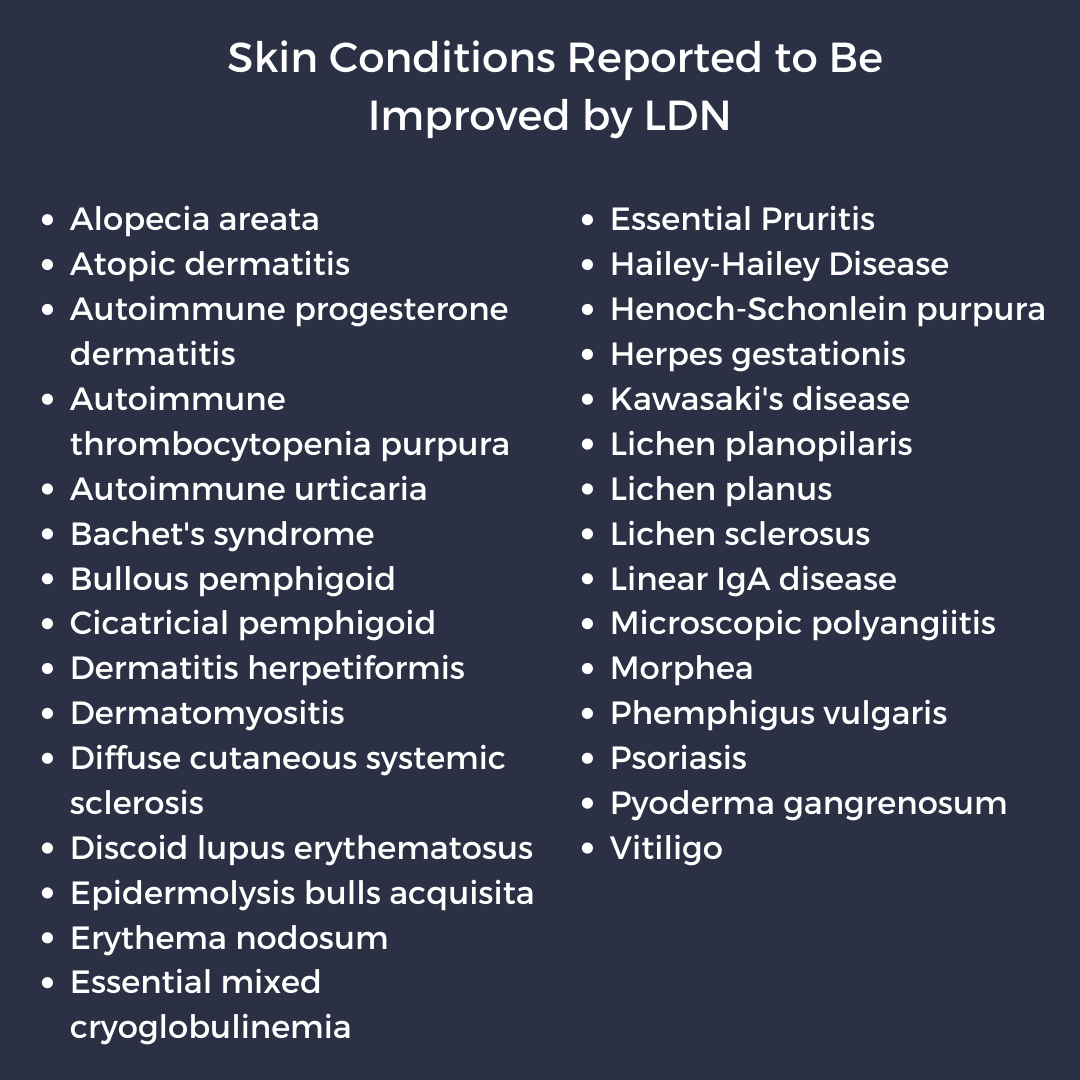
- See the lists below of possible skin diseases and non-dermatologic diseases that could be improved with LDN. Dr. Bodemer recommends using LDN, in particular, when patients also have these other issues as there may be additional benefit for the patient
- Specifically, for LPP – consider starting the patient on Plaquenil (or other medication) as well as LDN and understand that LDN takes time to work and patience on the part of the physician and patient
What are the risks?
-
- No labs are generally needed prior to starting or for monitoring
- Important to screen for thyroid disease (clinically) as LDN can improve thyroid function in patients with autoimmune thyroiditis and decrease the need for thyroid hormone replacement – so the patient could end up in a hyperthyroid state
- Someone with thyroid disease should have TSH levels checked every 3-4 months until stable dose of naltrexone
- Interacts with opiate medications – withdrawal symptoms
- Sleep disturbance (vivid dreams for 4-7 nights), insomnia (4-7 days), nausea, diarrhea, constipation, most side effects disappear in 4-7 days, if severe symptoms – decrease dose by 50% for 7 days and then titrate up slowly
Prescribing
-
- The best way to dose this is with compounded liquid – 1mg/ml
- Dr. Bodemer typically has it compounded in a fixed oil base at 1 mg/ml (not a pleasant taste)
- Can also be created in capsules, sublingual drops, and creams (1-2% cream topically for neurogenic itch or essential pruritis)
- Crushing a tablet and mixing with 50ml of water has been reported but this may be less effective as it will be more difficult to accurately titrate for the patient – Dr. Bodemer mentioned that this method may be why some patients fail as it may be hard to find the narrow therapeutic window this way.
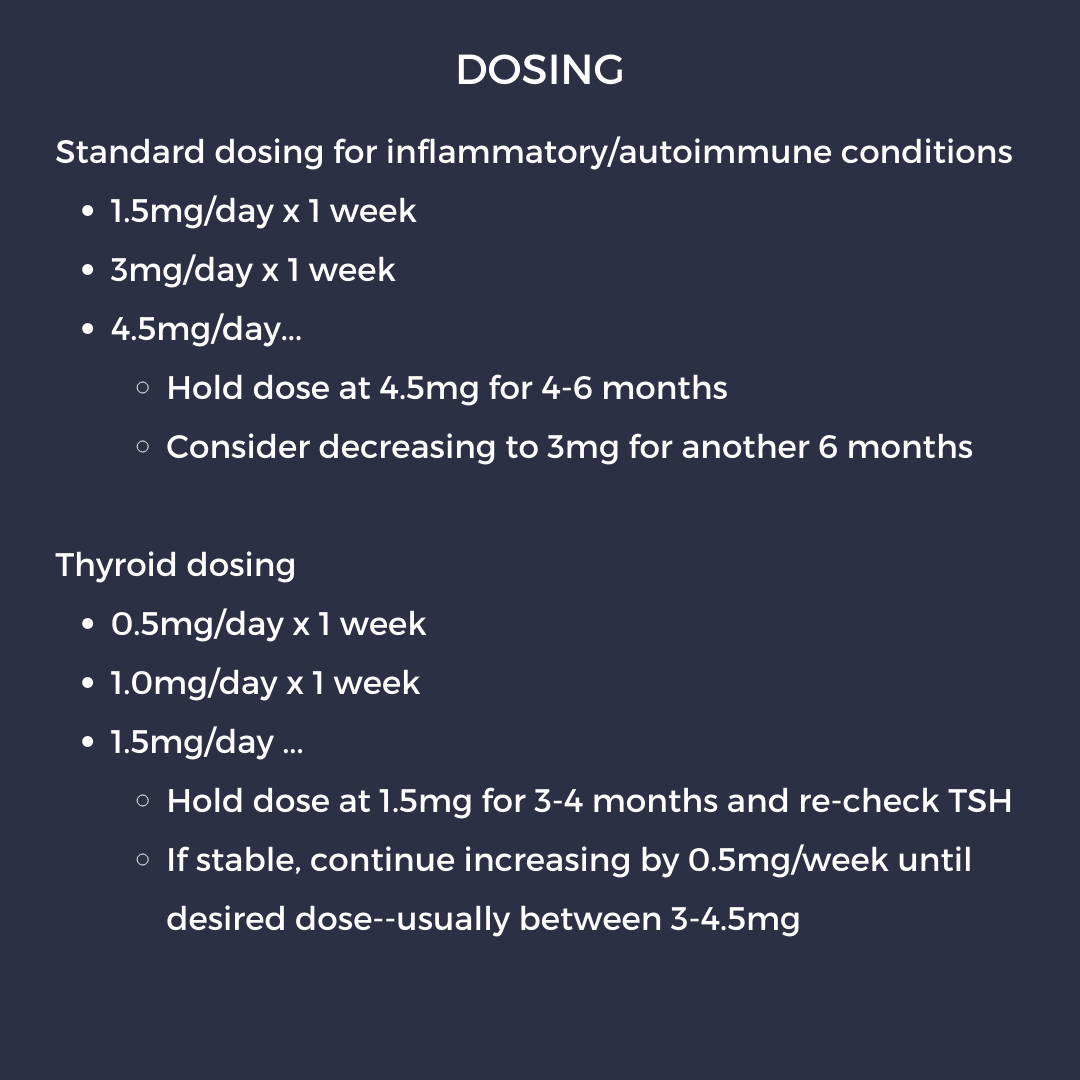
- See below for thoughts on dosing strategies
- There is a sweet spot for each patient – so dose adjustments are often needed and sometimes using this for 1-2 years and trying different doses to get it right for each patient is required
Final Thoughts
-
- Consider LDN as a nice adjunctive treatment for many inflammatory and auto-immune conditions
- It takes time to find the right dose
- Remember the possible effects on thyroid equilibrium in patients with thyroid disease
Are you treating patients with LDN? Have you had success with a crushed tablet mixed with liquid, are you getting it compounded? Have you/your patients had success?
Please share your comments and join the discussion at the end of this post, and on Instagram @nextstepsinderm!
Dr. Apple Bodemer, MD, FAAD, DABOIM is an Associate Professor of Dermatology at the University of Wisconsin, Madison.
The above article was written by Dr. James J. Contestable (Derm In-Review Advisory Council Member) and represents his interpretation of the information presented by Dr. Bodemer during her lecture “Low dose Naltrexone in Dermatology” at the 2020 Integrative Dermatology Symposium.
Did you enjoy this article? Find more on Integrative Dermatology here.