Over 350 years Dr. Samual Hafenreffer first defined itch as the “unpleasant sensation that provokes a person to scratch”. Pruritus has been challenging to treat ever since. Pruritus is complicated, and it’s often hard to know where to start when a patient has a chief complaint of itching. Thankfully, Dr. Friedman gave the audience some practical tips for diagnosing and treating pruritus at the 17th Annual ODAC Dermatology, Aesthetic and Surgical conference held January 17-20, 2020 in Orlando, FL. We owe it to our patients to figure out why they are itchy and ease their symptoms because pruritus can be a harbinger for underlying disease and has a tremendous impact on patient quality of life. Moreover, pruritus is very common: about 13.5% point-prevalence in the general adult population. In this article, we’ll break down the major causes of pruritus and try to tease out nuances to diagnosis and treat our itchy patients.
Sources of Itch
We can categorize itch into different groups, organized by what is causing the sensation.
The first category, which dermatologists are often most comfortable with, is caused by inflammation or skin damage, and presents with skin lesions with or without evidence of scratching. Examples include atopic dermatitis, psoriasis, xerosis, scabies, contact dermatitis, arthropod assault, and lichen planus. Don’t forget about nonbullous pemphigoid! Consider performing a perilesional DIF and serum IIF for patients in the right age group.
When there are no primary skin lesions, with or without evidence of chronically scratched lesions, the cause can be systemic, neuropathic, or psychogenic.
There are many systemic diseases that lead to pruritus including chronic kidney disease, cholestasis, Hodgkin’s lymphoma, polycythemia vera, HIV infection, and hyperthyroidism. This list is not exhaustive by any means- other causes include iron deficiency, intestinal parasites, pregnancy, myeloma, solid tumors, multiple sclerosis, and anorexia nervosa. If you’re suspicious of internal causes, your physical exam should include a check of the patient’s lymph nodes and hepatomegaly (concern for malignancy), and fine tremor (concern for hyperthyroidism).
Patients with pruritus on the palms without a rash, especially in females, should spark consideration of primary biliary cirrhosis or cholestatic itch.
Neuropathic causes of pruritus include brachioradial pruritus, notalgia paresthetica, and post-herpetic itch. If you see itching in dermatomal distribution, this is likely a clue to neuropathic causes. Localized itch of the genital area (i.e. vulva, scrotum) or to the scalp is often neuropathic in etiology. This type of itch is often described as “painful” by patients.
Finally, the psychogenic causes include OCD, delusions of parasitosis, and substance abuse.
It’s also important to keep in mind that patients can have a mixed etiology of their itch!
Mediators of itch
Another way to think about itch is a consideration of what in the body is mediating the sensation. These mediators work centrally and peripherally to drive the itch and include commonly known substances like histamines, proteinases (i.e. tryptase), substance P, opiates, and prostaglandins. We can think about the keratinocyte as the primary organ of itch, as keratinocytes have receptors that receive these mediators of itch. Targeting these mediators of itch has been the backbone of treatment for pruritus.
“Is it a rash that itches, or an itch that rashes?”
When a patient with a chief complaint of itch comes into your clinic, there are a few questions that can help you elucidate which type of itch they have, and/or what is mediating their itch. Dr. Friedman referred to Dr. Pereiria’s 1 approach to the initial visit for an itchy patient, which assesses the following:
-
- Where on your body did the itch start?
- Did the itch start with or without a rash? Is the itch just where the rash is?
- Is the duration of the rash less than a year?
- Consider lymphoma or liver tumor in the right age group
- Does it itch worse with water exposure?
- Consider polycythemia vera if so
- Is the itch induced by friction?
- How intensely itchy is it?
- How is the itch affecting your quality of life?
On physical exam, it’s important to look for evidence of scratching on diseased skin only, or if the scratching on non-diseased skin, or if there are signs of chronic scratching.
A good baseline laboratory work-up for itchy patients would include CBC, CMP, and thyroid function labs. Chest X-ray for malignancy and stool O&P for parasites are good add-ons in certain age groups or exposures, or with pertinent travel history.
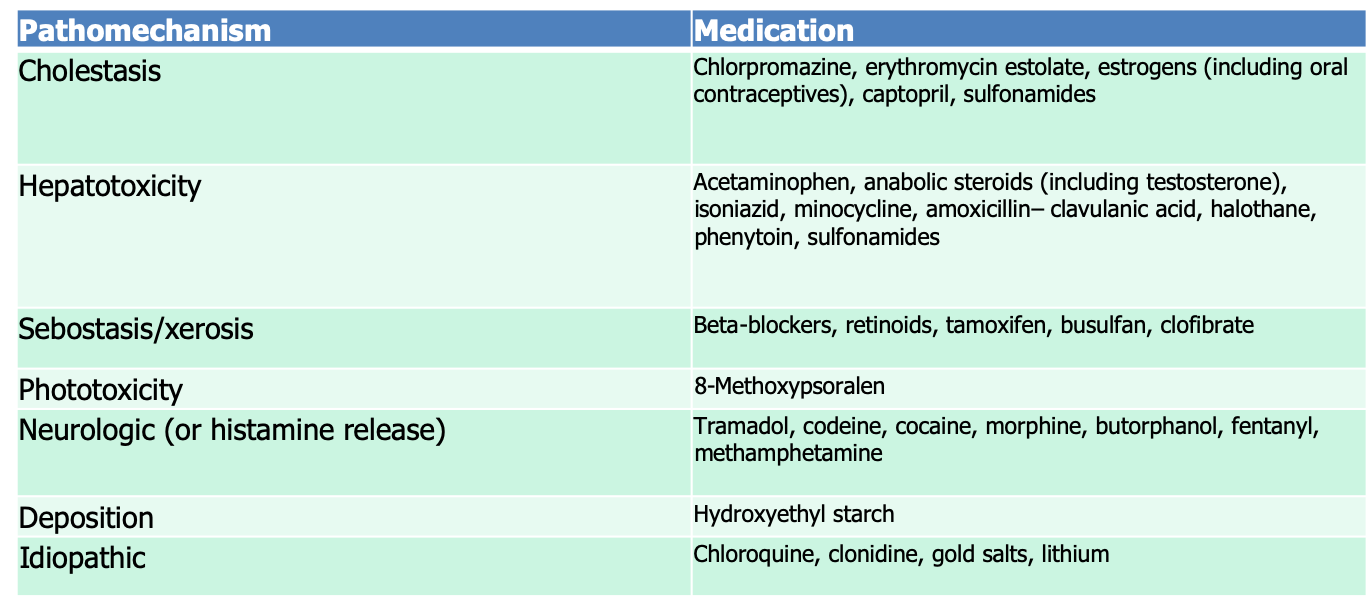
It’s also essential to review medications that the patient is taking, as there are many pharmacologic etiologies that may be responsible. A thorough review of all the medications, including over-the-counter therapies and vitamins, should be performed for all new patients with unexplained pruritus.
Dr. Friedman included the following helpful table of common pharmacologic causes of pruritus:
Quality of life
Dr. Friedman emphasized the impact on the quality of life suffered by patients with pruritus. Itch leads to irritability, anxiety, stress, loss of sleep, and even depression and suicidal ideation. Chronic pruritus manifests differently in children too- difficulty sleeping or paying attention in school can have major impacts on their development and ability to participate in school activities. Parents of kids who itch are also negatively impacted. An assessment of quality of life impact in your pruritic population at each appointment will be a good indicator of how your therapies are working. With that in mind, let’s dive into some basics and more nuanced recommendations for treatment of pruritus.
Therapies for the itchy patient
Therapeutic approaches for pruritus are as varied as the causes of pruritus.
Dr. Friedman discussed some basics that work for all causes of pruritus and are a good starting point.
-
- Non-alkaline soaps and moisturizers
- Soft cotton clothes
- Luke warm water with baths (hot water causes histamine release!)
- Daily emollient use
A mis-conception is that anti-histamines are good for chronic itch- however, most of the time, chronic pruritus is not histamine-mediated, therefore this class of medications is usually not very helpful in this population. The main benefit is that anti-histamines can help people sleep at night, due to their centrally-acting side effects.
Topicals:
-
- Some topical medications work by decreasing inflammation (i.e. glucocorticosteroids and calcineurin inhibitors)
- Some topical medications work by inhibiting neurologic activation (i.e. menthol, capsaicin, pramoxine, compounded ketamine)
New areas of interest are the use of topical endocannabinoids and palmyitoyethanolamide (which stimulates anandamide activation of cannabinoid 1 receptor) for the treatment of pruritus2 , as well as inflammatory conditions like atopic dermatitis. Topical ketamine, often compounded with topical amitriptyline and/or topical lidocaine, has been used for intractable itch3 and neuropathic itch with significant itch reduction4.
Systemic agents:
Dermatologist have borrowed medications used for other diseases, and in other fields of medicine, to treat itch. Gabapentin, SSRIs, mirtazapine, naltrexone, doxepin and amitriptyline have all been utilized to target mediators of chronic itch. Immunosuppressants and immunomodulators are potentially helpful for itch, especially in the context of pruritus due to diseased skin. The main goal is to target common elements found in multiple different itchy conditions to provide symptom relief.
Here are some pearls regarding systemic therapy for itch
-
- Gabapentinoids and mirtazapine work centrally through blockage of neurotransmitters in the CNS
- Adjust gabapentinoids for patients with kidney disease and for elderly patients
- Common adverse effects of naltrexone include abdominal cramps, muscle aches, difficulty sleeping, and feeling nervous
- Doxepin has potent anti-histamine activity via H1 and H2 blockage
- Aprepitant, which is a neurokinin-1 antagonist affecting substance P activation on keratinocytes, has been found to be helpful in patients with chronic pruritus due to underlying malignancy
- Cyclosporine can be used to help pruritic patients with fast onset of improvement. Dosing needs to be adjusted for renal disease and hypertension. Weekend dosing is a nice consideration for maintenance therapy once improved.
- Dupilimab has been shown to not only reduces presence of atopic dermatitis, but improves the itch associated with it.
- New studies are looking at IL-31 as a potential therapeutic target for itchy patients.
Lower doses of mirtazapine are more sedating than higher doses.
Other therapeutic considerations:
Treatment of itch should potentially include some psychological and behavior modifications. Relaxation techniques, habit reversal training, and using competing physical sensation to block the itch are all potentially useful tricks that are clearly safe for patient to try. Simple things like wearing long-sleeve shirts can make a difference in how much scratching someone is able to do. Behavioral changes can be especially helpful in pediatric patients who need a plan to help when they are itchy at school. Stress potentiates itch for many patients, therefore stress-reduction may be an important avenue to improve itch.
Prurigo nodularis special considerations
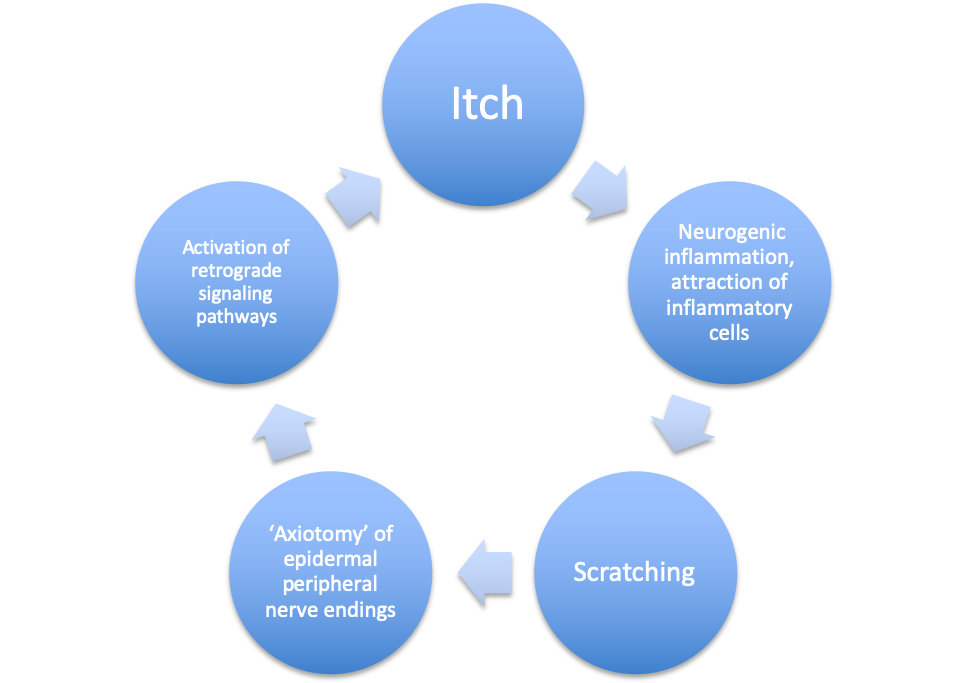
Prurigo nodularis should be considered its own disease entity. We don’t know the exact pathogenesis, but it is thought to be an inflammatory cycle that involves neurogenic inflammation and peripheral nerve endings that lead to the sensation of itching and eventual scratching, as shown in Dr. Friedman’s helpful graphic below.
The therapy approach should start with topical steroids and consideration of UV phototherapy, but patients may also need addition of systemic therapies, as discussed above. Thalidomide has been shown to be helpful in severe cases of prurigo nodularis, as has dupilimab.
The bottom line
Pruritus can be challenging to diagnosis and treat. The dermatologist’s job is to assess for primary dermatologic processes, neuropathic issues, and underlying systemic disease. The therapeutic approach should be multimodal. Don’t be afraid to treat aggressively, because the quality of life impact is significant for itchy patients.
References
-
- Pereira MP, Stander S. Assessment of severity and burden of pruritus. Allergol Int. 2017;66(1):3-7.
- Mounessa JS, Siegel JA, Dunnick CA, Dellavalle RP. The role of cannabinoids in dermatology. J Am Acad Dermatol. 2017;77(1):188-90.
- Lee HG, Grossman SK, Valdes-Rodriguez R, Berenato F, Korbutov J, Chan YH, et al. Topical ketamine-amitriptyline-lidocaine for chronic pruritus: A retrospective study assessing efficacy and tolerability. J Am Acad Dermatol. 2017;76(4):760-1.
- Poterucha TJ, Murphy SL, Davis MD, Sandroni P, Rho RH, Warndahl RA, et al. Topical amitriptyline-ketamine for the treatment of brachioradial pruritus. JAMA Dermatol. 2013;149(2):148-50.
Source:
This information was presented by Dr. Adam Friedman at the 17th Annual ODAC Dermatology, Aesthetic and Surgical Conference held January 17–20, 2020 in Orlando, FL. The above highlights from his lecture were written and compiled by Dr. Caroline Laggis, one of the 7 residents selected to participate in the Sun Young Dermatology Leader Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.).
Did you enjoy this post? Find more on Medical Derm topics here.