Dermatophyte infections are estimated to affect about 25% of the world’s population, representing some of the most common infections in the world. Conditions such as onychomycosis and tinea capitis may significantly impact quality of life by way of their symptoms or appearance, making adequate treatment important. Oral and topical formulations of terbinafine are commonly used on- and off-label for the treatment of numerous dermatophyte infections. We continue our series, Therapeutic Cheat Sheet, with a closer look at terbinafine.
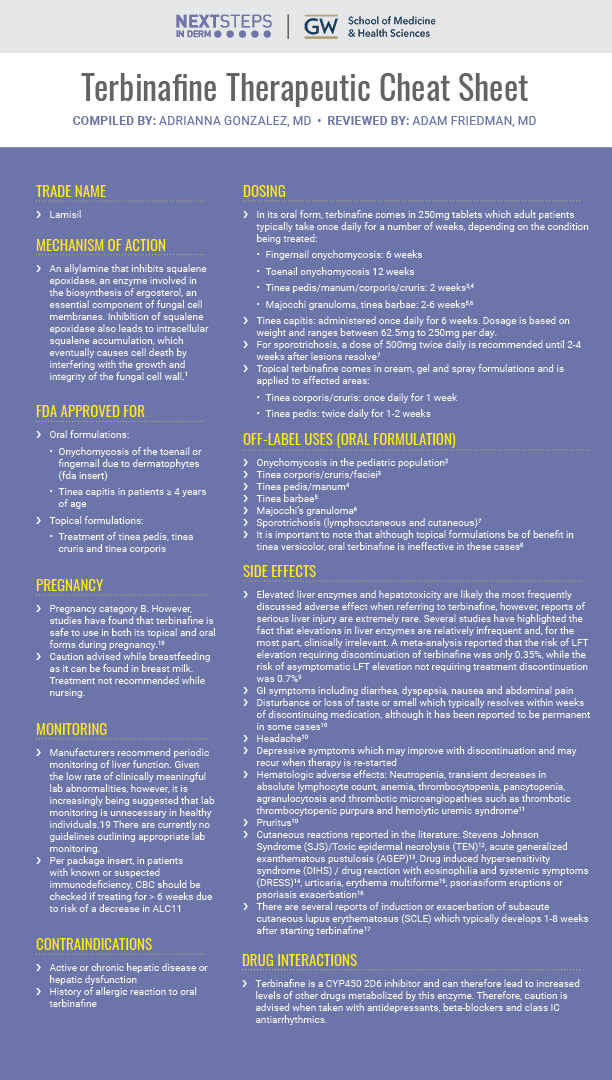
TERBINAFINE THERAPEUTIC CHEAT SHEET
Compiled by: Adrianna Gonzalez, MD | Reviewed by: Adam Friedman, MD
TRADE NAME
-
- Lamisil
MECHANISM OF ACTION
-
- An allylamine that inhibits squalene epoxidase, an enzyme involved in the biosynthesis of ergosterol, an essential component of fungal cell membranes. Inhibition of squalene epoxidase also leads to intracellular squalene accumulation, which eventually causes cell death by interfering with the growth and integrity of the fungal cell wall.1
FDA APPROVED FOR
-
- Oral formulations:
- Onychomycosis of the toenail or fingernail due to dermatophytes (FDA insert)
- Tinea capitis in patients ³ 4 years of age
- Topical formulations:
- Treatment of tinea pedis, tinea cruris, and tinea corporis
- Oral formulations:
OFF-LABEL USES (ORAL FORMULATION)
-
- Onychomycosis in the pediatric population2
- Tinea corporis/cruris/faciei3
- Tinea pedis/manum4
- Tinea barbae5
- Majocchi’s granuloma6
- Sporotrichosis (lymphocutaneous and cutaneous)7
- It is important to note that although topical formulations can be of benefit in tinea versicolor, oral terbinafine is ineffective in these cases8
DOSING
-
- In its oral form, terbinafine comes in 250mg tablets which adult patients typically take once daily for a number of weeks, depending on the condition being treated:
- Fingernail onychomycosis: 6 weeks
- Toenail onychomycosis 12 weeks
- Tinea pedis/manum/corporis/cruris: 2 weeks3,4
- Majocchi granuloma, tinea barbae: 2-6 weeks5,6
- Tinea capitis: administered once daily for 6 weeks. Dosage is based on weight and ranges between 62.5mg to 250mg per day.
- For sporotrichosis, a dose of 500mg twice daily is recommended until 2-4 weeks after lesions resolve7
- Topical terbinafine comes in cream, gel and spray formulations and is applied to affected areas:
- Tinea corporis/cruris: once daily for 1 week
- Tinea pedis: twice daily for 1-2 weeks
- In its oral form, terbinafine comes in 250mg tablets which adult patients typically take once daily for a number of weeks, depending on the condition being treated:
SIDE EFFECTS
-
- Elevated liver enzymes and hepatotoxicity are likely the most frequently discussed adverse effect when referring to terbinafine, however, reports of serious liver injury are extremely Several studies have highlighted the fact that elevations in liver enzymes are relatively infrequent and, for the most part, clinically irrelevant. A meta-analysis reported that the risk of LFT elevation requiring discontinuation of terbinafine was only 0.35%, while the risk of asymptomatic LFT elevation not requiring treatment discontinuation was 0.7%9
- GI symptoms including diarrhea, dyspepsia, nausea and abdominal pain
- Disturbance or loss of taste or smell which typically resolves within weeks of discontinuing medication, although it has been reported to be permanent in some cases10
- Headache10
- Depressive symptoms which may improve with discontinuation and may recur when therapy is re-started
- Hematologic adverse effects: Neutropenia, transient decreases in absolute lymphocyte count, anemia, thrombocytopenia, pancytopenia, agranulocytosis and thrombotic microangiopathies such as thrombotic thrombocytopenic purpura and hemolytic uremic syndrome11
- Pruritus10
- Cutaneous reactions reported in the literature: Stevens Johnson Syndrome (SJS)/Toxic epidermal necrolysis (TEN)12, acute generalized exanthematous pustulosis (AGEP)13, Drug induced hypersensitivity syndrome (DIHS) / drug reaction with eosinophilia and systemic symptoms (DRESS)14, urticaria, erythema multiforme15, psoriasiform eruptions or psoriasis exacerbation16
- There are several reports of induction or exacerbation of subacute cutaneous lupus erythematosus (SCLE) which typically develops 1-8 weeks after starting terbinafine17
CONTRAINDICATIONS
-
- Active or chronic hepatic disease or hepatic dysfunction
- History of allergic reaction to oral terbinafine
DRUG INTERACTIONS
-
- Terbinafine is a CYP450 2D6 inhibitor and can therefore lead to increased levels of other drugs metabolized by this enzyme. Therefore, caution is advised when taken with antidepressants, beta-blockers, and class IC antiarrhythmics.
PREGNANCY
-
- Pregnancy category B. However, studies have found that terbinafine is safe to use in both its topical and oral forms during pregnancy.18
- Caution advised while breastfeeding as it can be found in breast milk. Treatment not recommended while nursing.
MONITORING
-
- Manufacturers recommend periodic monitoring of liver function. Given the low rate of clinically meaningful lab abnormalities, however, it is increasingly being suggested that lab monitoring is unnecessary in healthy individuals.19 There are currently no guidelines outlining appropriate lab monitoring.
- Per package insert, in patients with known or suspected immunodeficiency, CBC should be checked if treating for > 6 weeks due to risk of a decrease in ALC11
Terbinafine is an FDA-approved treatment that is safe and efficacious for the treatment of many dermatophyte infections. Adequate treatment of these conditions is imperative, as it may often negatively impact quality of life. Patients should be educated regarding labeled warnings and side effects prior to starting therapy.
CLICK ON THE IMAGE BELOW TO DOWNLOAD YOUR THERAPEUTIC CHEAT SHEET
FURTHER READING
If you would like to learn more about Terbinafine for the treatment of onychomycosis , check out the following articles published in the Journal of Drugs in Dermatology:
Clinical Insights About Onychomycosis and Its Treatment: A Consensus
Background: Recently, experience and knowledge have been gained using effective topical treatment for onychomycosis, a difficult-to-treat infection.
Methods: This project aims to help understand and improve patient-focused quality of care for fungal nail infections. A panel of dermatologists who treat onychomycosis convened on several occasions to review and discuss recent learnings in the treatment of onychomycosis. The panel developed and conducted a survey on diagnosis, treatment and prevention, discussed the results, and provided recommendations.
Results: The survey was sent out digitally to the Canadian Dermatology community. Ninety-two dermatologists completed the questionnaires, which were included in the analysis. The survey respondents and panel members agreed that the diagnosis of toe onychomycosis should be confirmed with a positive microscopic examination for fungus or a positive mycological culture when oral therapy and/or topical treatment is prescribed, except when it is not clinically feasible, in which case topical therapy could be started based on clinical presentation. The panel and survey respondents also agreed that treatment is to be based on percentage of nail involvement: less than 20%=topical efinaconazole; 20%-60%=topical efinaconazole±oral terbinafine (for greater than 3 nails); greater than 60%=oral terbinafine±topical therapy.
Conclusions: The current treatment paradigm for onychomycosis may have shifted from mainly oral antifungals to topical treatment, improving patient-focused quality of care.
J Drugs Dermatol. 2018;17(3):253-262. Read the full article here.
Rapid Treatment of Subungual Onychomycosis Using Controlled Micro Nail Penetration and Terbinafine Solution
Abstract: Onychomycosis continues to be a common and intractable problem in adults, often responding poorly to topical treatment due to limited drug penetration of the nail plate. Improving penetration has been attempted previously by chemical and physical means with some success. The authors present three cases of toenail onychomycosis treated topical terbinafine 1% solution using controlled micro-penetration of the nail using a novel intelligent nail drill system which is able to drill nail plate without penetrating the delicate nail bed beneath. The cases illustrate how the device has been successfully employed to deliver the anti-fungal drug directly and rapidly to the site of infection with minimal side effects or complications, whilst maintaining the nail integrity.
J Drugs Dermatol. 2016;15(8):974-978. Read the full article here.
References
-
- Van Duyn Graham L, Elewski BE. Recent updates in oral terbinafine: its use in onychomycosis and tinea capitis in the US. Mycoses. 2011;54(6):e679-685.
- Gupta AK, Adamiak A, Cooper EA. The efficacy and safety of terbinafine in children. J Eur Acad Dermatol Venereol. 2003;17(6):627-640.
- Bhatia A, Kanish B, Badyal DK, Kate P, Choudhary S. Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin – A prospective, randomized comparative study. Indian J Pharmacol. 2019;51(2):116-119.
- White JE, Perkins PJ, Evans EG. Successful 2-week treatment with terbinafine (Lamisil) for moccasin tinea pedis and tinea manuum. Br J Dermatol. 1991;125(3):260-262.
- Wendrock-Shiga G, Mechtel D, Uhrlass S, Koch D, Kruger C, Nenoff P. [Tinea barbae profunda due to Trichophyton mentagrophytes after journey to Thailand : Case report and review]. Hautarzt. 2017;68(8):639-648.
- Boral H, Durdu M, Ilkit M. Majocchi’s granuloma: current perspectives. Infect Drug Resist. 2018;11:751-760.
- Francesconi G, Francesconi do Valle AC, Passos SL, et al. Comparative study of 250 mg/day terbinafine and 100 mg/day itraconazole for the treatment of cutaneous sporotrichosis. Mycopathologia. 2011;171(5):349-354.
- Rivard SC. Pityriasis versicolor: avoiding pitfalls in disease diagnosis and therapy. Mil Med. 2013;178(8):904-906.
- Chang CH, Young-Xu Y, Kurth T, Orav JE, Chan AK. The safety of oral antifungal treatments for superficial dermatophytosis and onychomycosis: a meta-analysis. Am J Med. 2007;120(9):791-798.
- Wang Y, Lipner SR. Retrospective analysis of adverse events with systemic onychomycosis medications reported to the United States Food and Drug Administration. J Dermatolog Treat. 2020:1-5.
- Novartis Pharmaceuticals Coorporation. Lamisil (terbinafine hydrochloride) [package insert]. U.S. Food and Drug Administration website.https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/020539s033lbl.pdf. Revised March 2019. Accessed February 22, 2021.
- Banik B, Bhar D, Sil A. Terbinafine-induced Steven-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN) overlap. Postgrad Med J. 2020.
- Correia B, Costa J, Egipto P, Reis P. Terbinafine-induced acute generalized exanthematous pustulosis. J Burn Care Res. 2021.
- Rajagopal Srinivasan V, Singh S, Bharti JN, Vedant D. Terbinafine-induced DRESS syndrome mimicking eosinophilic cellulitis. J Eur Acad Dermatol Venereol. 2021;35(2):e145-e147.
- Slim R, Fathallah N, larif S, et al. Terbinafine induced Erythema multiforme with Hepatitis. Clinical Therapeutics. 2015;37(8):e90-e91.
- Chiu HY, Chang WL, Tsai TF, Tsai YW, Shiu MN. Risk of Psoriasis Following Terbinafine or Itraconazole Treatment for Onychomycosis: A Population-Based Case-Control Comparative Study. Drug Saf. 2018;41(3):285-295.
- Kalinska-Bienias A, Kowalewski C, Wozniak K. Terbinafine-induced subacute cutaneous lupus erythematosus in two patients with systemic lupus erythematosus successfully treated with topical corticosteroids. Postepy Dermatol Alergol. 2013;30(4):261-264.
- Andersson NW, Thomsen SF, Andersen JT. Evaluation of Association Between Oral and Topical Terbinafine Use in Pregnancy and Risk of Major Malformations and Spontaneous Abortion. JAMA Dermatol. 2020;156(4):375-383.
- Stolmeier DA, Stratman HB, McIntee TJ, Stratman EJ. Utility of Laboratory Test Result Monitoring in Patients Taking Oral Terbinafine or Griseofulvin for Dermatophyte Infections. JAMA Dermatol. 2018;154(12):1409-1416.
Did you enjoy this therapeutic cheat sheet? You can find more here.