As dermatology residents, injecting filler during our demo sessions is always exciting, as it is not something we have the opportunity to practice frequently. It can also be daunting, especially with the possibility of vascular complications. Patients come to you wanting to enhance their appearance, and the idea of possibly causing permanent and serious adverse effects can be terrifying.
Thankfully, during a very informative talk presented at the 17th Annual ODAC Dermatology, Aesthetic & Surgical Conference by Dr. Joel Cohen, Mohs Surgeon and well-known and well-published fellowship-trained Aesthetic Dermatologist, Director of AboutSkinDermatology and DermSurgery in metropolitan-Denver, Colorado, and Associate Clinical Professor at the University of California at Irvine, I was able to better understand how to treat any possible vascular complications from filler. Dr. Cohen published a JDD article in the past showing his Mohs photos to help explain related filler anatomy. Here are a few of the tips and practice pearls I learned:
-
- Many people think aspirating prior to injecting helps make it safer, however, false-negative results are still possible!
- When injecting, ensure that there is no blanching and have the patient call if there are any concerns
- There is no need to stop any therapeutic anticoagulation medications prior to injections, however, any supplements can be stopped
What About Cannula?
The new teaching paradigm with fillers is that cannulas are safer than needles, as cannulas typically require more force to enter a vessel. However, Dr. Cohen clarified that studies show that in reality, a 27G needle and a cannula take a similar amount of force to enter a vessel. Where a difference can really be seen is with a 25G cannula, as this usually requires more force and should be safer.
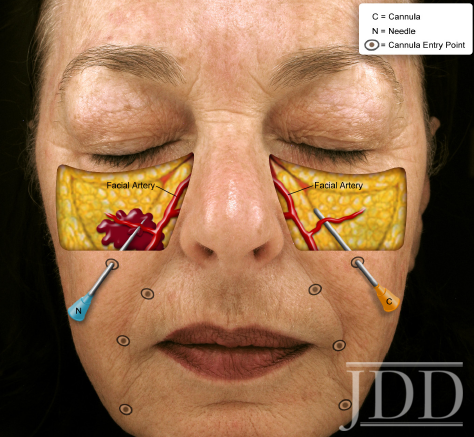
Therefore, when injecting in the area of the angular artery or transverse facial artery, cannula might be a safer option as it can slide above or below the artery. Be careful though, as many people like to pull up on the skin while injecting, and this can actually iatrogenically cause the transverse facial artery to become more superficial and easier to hit.
Purpura vs Impending Necrosis
For non-derms, telling the difference between purpura (figure 1) and impending necrosis (figures 2 and 3) can be tricky. Dr. Cohen explained:
- Necrosis will often appear duskier and more midline, and it is typically painful and in a segmental distribution of the underlying vessel
- On the central face, the palate can be a good place to check for necrosis
- Pustules or bumps over an area can be a clue for arterial compromise and necrosis
- Ocular complications are most common when doing nasal augmentation and glabella injections, but can certainly be seen with various injection points (especially around the eyes) as per the current studies

- Figure 1. Purpura secondary to soft tissue filler at tear throughs.


Be Prepared
As the Scout Motto says, “Be Prepared”. It is important to have hyaluronidase ready just in case anything happens. One important reminder is that hyaluronidase has a short shelf life, therefore expiration dates should be checked frequently to ensure effective hyaluronidase is always available.
-
- Hyaluronidase appears to diffuse through vessel walls and can truly make a difference (figures 4-6). Dr. Cohen co-authored an article along with Dr. Jean Carruthers in Derm Surgery over 10 years ago on successfully recommending hyaluronidase along the distribution of the occluded vessel. Dr. Cohen also co-authored a recent Derm Surgery article with Drs. Joshua Mo and Lance Chapman on common medications used in emergency dermatological situations.
-
- One great tip I learned is to consider using a Doppler to find areas that have less flow and inject hyaluronidase in that area. As it will disperse, being close enough can be sufficient.
-
- Compounded hyaluronidase can be inconsistent, and therefore standard hyaluronidase should always be used.
-
- Restylane might be easier to dissolve than Boletero or Juvederm as it has a higher number of cross-linking bonds and a higher concentration of hyaluronic acid.
-
- Know how to do a retrobulbar injection just in case ocular complications arise.



What else?
Although hyaluronidase is the mainstay of treating any vascular occlusion, don’t forget that there are various adjuvant therapies such as:
-
- Nitroglycerin paste can potentially help increase perfusion to an area and can be applied to the area of impending necrosis (there is a good deal of discussion about this topic. Dr. Cohen co-authored a recent Derm Surgery article with Sama Carley on this topic).
- Low molecular weight heparins, IV prostaglandin-E, hyperbaric oxygen, and sildenafil are all possible therapies to try.
It is important to be an expert at recognizing the different phases of necrosis so that you can quickly identify any problems and treat them appropriately. As they always say, prepare for the worst, hope for the best.
This information was presented by Dr. Joel Cohen at the 17th Annual ODAC Dermatology, Aesthetic and Surgical Conference held January 17–20, 2020 in Orlando, FL. The above highlights from his lecture were written and compiled by Dr. Angela Hou, PGY-3 dermatology resident at George Washington University and one of the 7 residents selected to participate in the Sun Young Dermatology Leader Mentorship Program (a program supported by an educational grant from Sun Pharmaceutical Industries, Inc.).
Image Credits
All images used with permission from the Journal of Drugs in Dermatology.
Figure 1
https://jddonline.com/articles/dermatology/S1545961613P1219X/1
Featured Article Image and Figures 2 and 3
https://jddonline.com/articles/dermatology/S1545961613P1181X/1
Figures 4, 5, 6
https://jddonline.com/articles/dermatology/S1545961607P0325X/1
Did you enjoy this post? Find more on Aesthetic Dermatology here.


