ABSTRACT
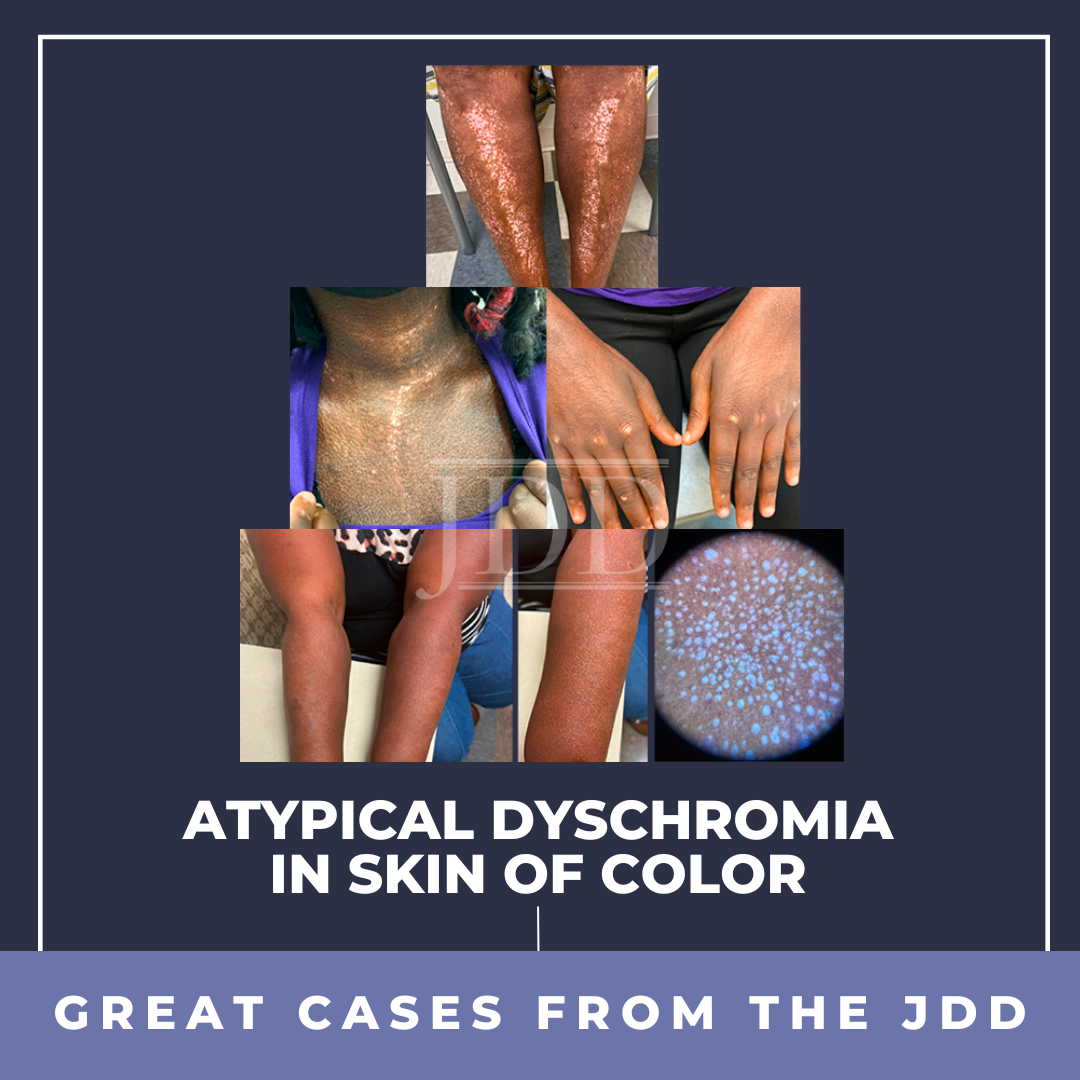
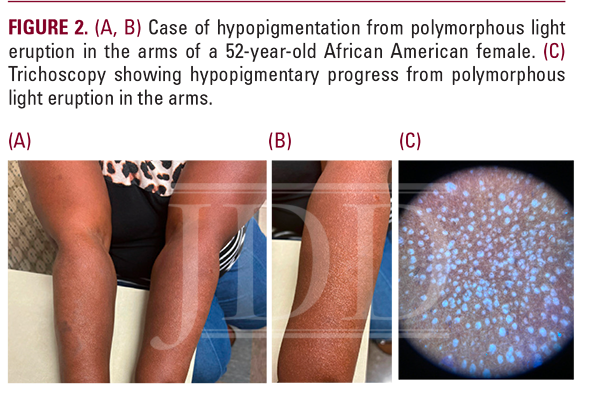
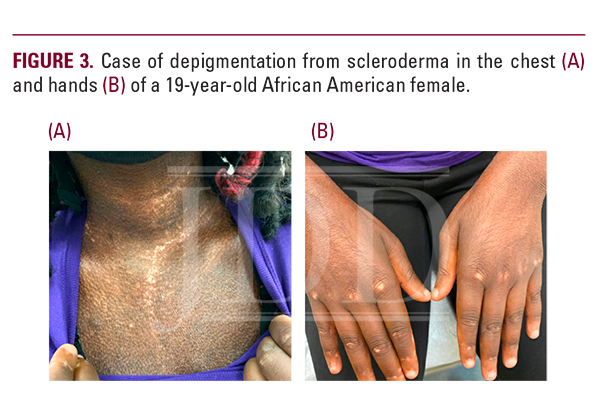
INTRODUCTION
Dyschromia is often the result of an external or internal insult to the skin.1 It is a concern for many patients, especially persons of color.2,3 In black patients, dyschromia is a common diagnosis and substantially affects their quality of life.2-4 Current literature focuses on post-inflammatory hyperpigmentation and treatment options. However, literature on etiologies of secondary hypopigmentation and depigmentation is sparse.1 Hypopigmentation and depigmentation can affect all skin tones; they are more apparent in darker skin.1 Literature suggests several diseases that may present with hypopigmentation and/or depigmentation despite this not being a major criterion for these conditions.5-11 Inflammation associated with atopic dermatitis (AD) may result in hypopigmented change and has been reported in several cases.5-7 There have been three reports of lichen planus (LP) presenting in skin of color as hypopigmented macules.8 Hypopigmentation is unusual for LP as it presents classically with hyperpigmentation.8 Discoid lupus erythematosus (DLE) often presents with erythema, induration, and follicular plugging.9 Presentation of DLE as depigmentation has been reported in seven cases and remains a rarely reported occurrence.9-11 Similarly, scleroderma-associated depigmentation has also been reported.12-15 Here, we present three cases of atypical dyschromia in skin of color to highlight the underlying hypo- and depigmentation that may present with active disease and persist despite appropriate treatment.
Report of a Case of Depigmentation From AD
A 66-year-old African American woman presented to our clinic for a complete body examination of AD. She reports that her AD started around age 52 at menopause, with itching on the legs. Her AD worsened in the past 2-3 years and was particularly bothersome in the summer. She had been treated previously at an outside dermatology office and had tried Dupilumab for a short time; she developed a rash and stopped this medication. She had also tried ultrapotent topical steroids, and topical calcineurin inhibitors, none of which controlled her pruritus or outbreaks.

Report of a Case of Hypopigmentation From Polymorphous Light Eruption (PMLE)
Report of a Case of Depigmentation From Scleroderma
DISCUSSION
Research is limited on treatment options for hypopigmentation and depigmentation in skin of color.15 Treatment recommendations focus on the identification and treatment of the primary disease process.15 Cosmetic topical and procedural therapies are also available.15 Two studies reported moderate to excellent repigmentation in skin of color patients treated with topical Psoralen + ultraviolet light A.17,18 Reszko et al reported complete repigmentation in an African American male with postinflammatory hypopigmentation using 17 treatments of Q-switched Ruby Laser.19 However, this has not been reported in a large number of skin of color patients and could lead to worsening of dyschromia in patients with dark skin.
Postinflammatory hypopigmentation and depigmentation remain a challenge faced by patients and providers. The impact of this process is more apparent in those with darker skin. Some members of the dermatology community may not comprehensively understand the mechanisms of these reactions and the extent of the psychosocial effect they have on persons of color. Skin of color patients experiencing a decrease or loss of pigmentation are left with few options for treating this process, with no available evidence-based treatment established from a sufficient sample size.
DISCLOSURES
REFERENCES
-
- Madu PN, Syder N, Elbuluk N. Postinflammatory hypopigmentation: a comprehensive review of treatments. J Dermatolog Treat. 2022;33(2):704-708. doi: 10.1080/09546634.2020.1793892. PMID: 32643458.
- Kang SJ, Davis SA, Feldman SR, et al. Dyschromia in skin of color. J Drugs Dermatol. 2014;13(4):401-6. PMID: 24719058.
- Davis SA, Narahari S, Feldman SR, et al. Top dermatologic conditions in patients of color: an analysis of nationally representative data. J Drugs Dermatol. 2012;11(4):466-473.
- Grimes PE. Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg. 2009;28(2):77-85.
- Eichenfield LF, Stein Gold LF. Practical strategies for the diagnosis and assessment of atopic dermatitis. Semin Cutan Med Surg. 2017;36(2 Suppl 2):S36-S38. doi: 10.12788/j.sder.2017.009. PMID: 28654708.
- Nader-Djalal N, Ansarin K. Hypopigmented skin lesions associated with atopic dermatitis in asthma. J Asthma. 1996;33(4):231-8. doi: 10.3109/02770909609055364. PMID: 8707778.
- Ichimiya M, Ohmura A, Muto M. Numerous hypopigmented patches associated with atopic dermatitis. J Dermatol. 1998 Nov;25(11):759-61. doi: 10.1111/j.1346-8138.1998.tb02498.x. PMID: 9863292.
- Arnold D, Hoffman MB, Onajin O, et al. Hypopigmented Macules as Manifestation of Lichen Planus and Lichen Planopilaris. Am J Dermatopathol. 2019;41(7):514-517. doi: 10.1097/DAD.0000000000001389. PMID: 30946098.
- Heath CR, Usatine RP. Discoid lupus. J Fam Pract. 2022;71(2):E16-E17. doi: 10.12788/jfp.0369. PMID: 35507819.
- Gupta S. Epidermal grafting for depigmentation due to discoid lupus erythematosus. Dermatology. 2001;202(4):320-3. doi: 10.1159/000051665. PMID: 11455144.
- Mulekar SV, Ghwish B, Al Issa A, et al. Melanocyte-keratinocyte transplantation for postdiscoid lupus erythematosus depigmentation. Dermatol Surg. 2008;34(2):261-2. doi: 10.1111/j.1524-4725.2007.34053.x. PMID: 18177409.
- Fujimoto N, Hamaguchi Y, Tanaka T. Vitiligo-like depigmentation with perifollicular pigment retention in systemic sclerosis treated successfully with suplatast tosilate. Eur J Dermatol. 2016;26(1):110-2. doi: 10.1684/ ejd.2015.2687. PMID: 26841835.
- De Villiers WJ, Jordaan HF, Bates W. Systemic sclerosis sine scleroderma presenting with vitiligo-like depigmentation and interstitial pulmonary fibrosis. Clin Exp Dermatol. 1992;17(2):127-31. doi: 10.1111/j.1365-2230.1992. tb00180.x. PMID: 1516238.
- Sanchez JL, Vazquez M, Sánchez NP. Vitiligolike macules in systemic scleroderma. Arch Dermatol. 1983;119(2):129-33. doi: 10.1001/ archderm.1983.01650260037013. PMID: 6337560.
- Carlson JA, Grabowski R, Mu XC, et al. A possible mechanism of hypopigmentation in lichen sclerosus. Am J Dermatopathol. 2002;24(2):97-107.
- Ruiz-Maldonado R, Orozco-Covarrubias ML. Postinflammatory hypopigmentation and hyperpigmentation. Semin Cutan Med Surg. 1997;16(1):36-43.
- Grimes PE, Bhawan J, Kim J, et al. Laser resurfacing-induced hypopigmentation: histologic alterations and repigmentation with topical photochemotherapy. Dermatol Surg. 2001;27(6):515-520.
- Lopez I, Ahmed A, Pandya AG. Topical PUVA for post-inflammatory hypopigmentation. J Eur Acad Dermatol Venereol. 2011;25(6):742-743.
- Reszko A, Sukal SA, Geronemus RG. Reversal of laser-induced hypopigmentation with a narrow-band UV-B light source in a patient with skin type VI. Dermatol Surg. 2008;34(10):1423-1426.
SOURCE
Moumen, M., & McMichael, A. J. (2024). Atypical Dyschromia in Skin of Color. Journal of Drugs in Dermatology: JDD, 23(2), 100-102.
Adapted from original article for length and style.