When treating Fitzpatrick skin types IV, V, and VI, it is important to recognize differences in common adverse events that may be experienced. In patients of color, hyperpigmentation is a primary concern. This article will discuss various causes of hyperpigmentation after dermal filler injections in patients of color as well as management strategies.
There is increasing racial and ethnic diversity in dermatology. By 2043, no single racial/ethnic group will make up a majority of America.1 The largest change will be among Hispanics, who will increase from 53.3 million in 2012 to 128.8 million in 2060, comprising 31% of the population. By 2060, 15% of Americans will be black, and 8.2% will be Asian.
Facial shape, skin surface and subsurface changes vary across racial and ethnic groups. Fitzpatrick IV-VI skin phototypes have increased collagen, elasticity and sebum production. Increased melanin pigment in these skin phenotypes can be both protective and a nuisance. Higher melanin concentrations will protect against the sun but can also result in hyperpigmentation in response to skin injury.
Surface changes (Extrinsic):
-
- Pigmentation
- Texture
- Fine wrinkling
Subsurface changes (Intrinsic):
-
- Volume loss
- Contours changes
- Redistribution of fat
The Hyaluronic Acid (HA) fillers that are currently available are safe to use in Fitzpatrick skin types IV, V, and VI. There is no significant risk for hypo- or hyperpigmentation, scarring or keloid formation. Patients may experience mild and transitory adverse events such as swelling and tenderness at the injection site, as well as redness, bruising and pain.2
When treating Fitzpatrick skin types IV, V, and VI, it is important to recognize differences in common adverse events that may be experienced. Redness, bruising and presentation of hyperpigmentation will vary among different skin phototypes.
Let’s review some real-life cases!
Case 1:
A 50-year-old female presented with infraorbital hollows. Two months after receiving tear trough fillers, she experienced reticulated hyperpigmentation.
What is the most likely cause?
This is an example of a hypersensitivity reaction to hyaluronic acid fillers. Hypersensitivity to HA presents as red-brown discoloration unresponsive to lightening agent such as hydroquinone or laser treatments (Nd:YAG 1064nm).
This is an uncommon reaction in all skin types but has been occasionally seen in skin types IV, V, VI undergoing aesthetic treatments in the infraorbital or nasolabial areas. Persistent red-brown hyperpigmentation resolves with hyaluronidase treatment in the affected areas. Hypersensitivity reactions have not been seen with hydroxylapatite or poly-L-lactic acid.
Treating Complications with Hyaluronidase
-
- Hyaluronidase has been found to be a spreading or diffusing substance, which modifies the permeability of connective tissue through the hydrolysis of HA
- Hyaluronidase breaks down excess HA by local injection into the area of excess
- Caution with bee sting allergy!
- Do not inject into any areas of infection
- There are 4 FDA-approved products
- Hyaluronidase usually comes as 150 IU per ml
- It is usually injected by diluting it with preserved saline and local anesthetics in a 1:1 dilution
- 5 units/0.1 ml of hyaluronic acid
- For Vycross technology, 10 units/0.1ml
This patient received 50 units of hyaluronidase to dissolve infraorbital HA with subsequent resolution of the reticulated hyperpigmentation.
Case 2:
A 35-year-old female presented with infraorbital hollows. She received tear trough fillers and developed bruising post-injection. Subsequently, a yellowish hue developed, followed by persistent, chronic gray-brown discoloration unresponsive to hydroquinone.
What is the most likely cause?
Hemosiderin deposition in the skin.
Hemosiderin has a slate gray appearance and results from extravasation of red blood cells that breakdown and expose iron contents in the skin. Hemosiderin deposition is unresponsive to bleaching agents.
Management: The patient received a trial of Q-switched Nd:YAG laser treatments over a period of 3 months with resolution of the gray-brown discoloration. If the patient was unresponsive to Nd:YAG laser treatment, hyaluronidase is necessary to dissolve the HA filler due to possible hypersensitivity reaction.
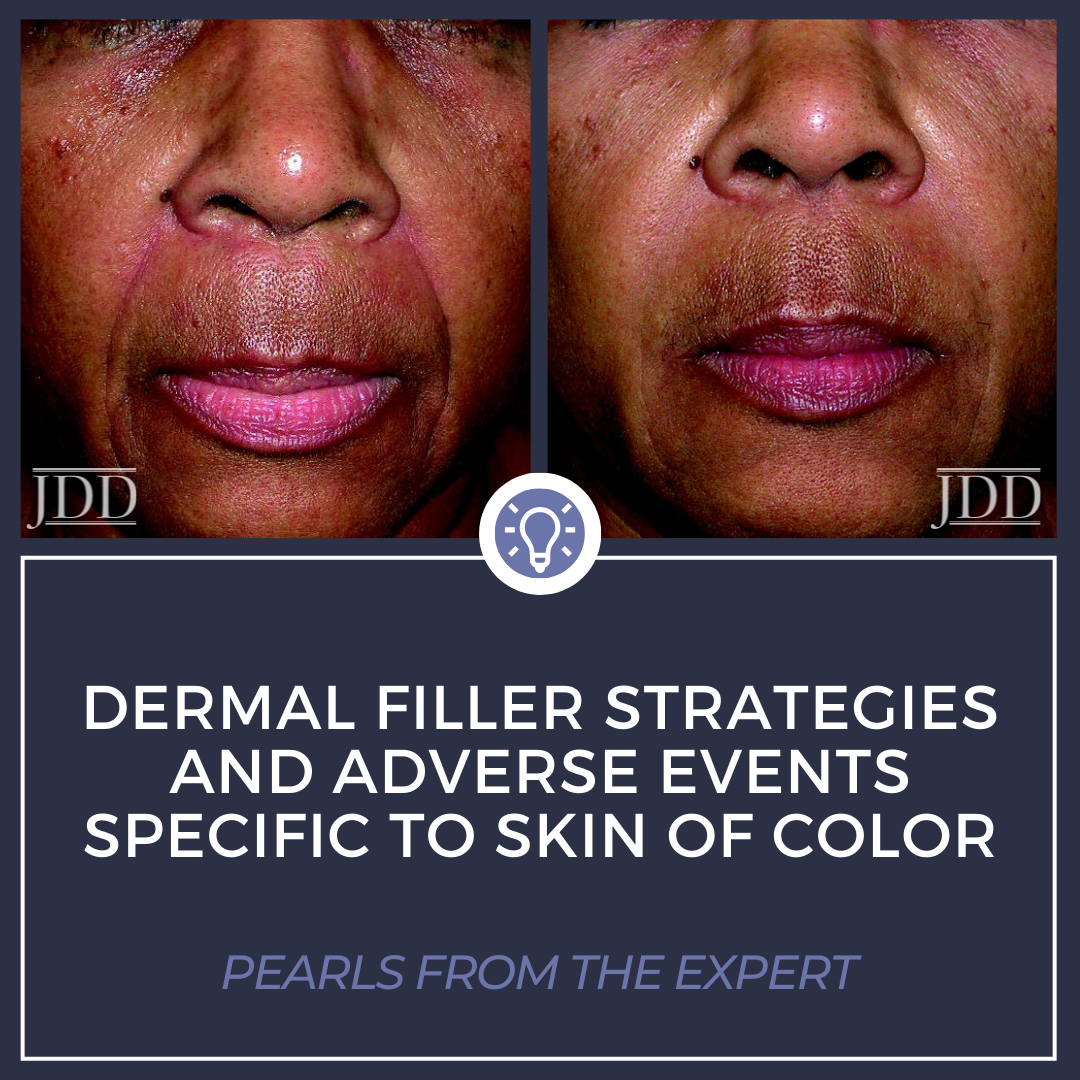
Case 3:
An 82-year-old woman was injected with HA fillers in the nasolabial folds. Serial injection technique was performed at the site of the deepest fold. Patient reports discoloration.
What is the most likely cause?
Post-inflammatory hyperpigmentation (PIH) secondary to multiple puncture injection technique.
In patients of color, a primary concern is minimizing the risk of hyperpigmentation. This can be accomplished by limiting the number of puncture sites.
Slower injection times also results in less PIH. Injecting sub-dermally with longer injection durations (slower injection time) will decrease the risk of PIH.
Management: 6 weeks of hydroquinone cream at bedtime resulted in resolution of PIH.
Case 4:
A 46-year-old woman was injected with HA dermal fillers of bilateral malar regions. A fanning injection technique was performed with a cannula. Patient reports a purple discoloration.
What is the most likely cause?
Bruising secondary to high injection speed.
When using hyaluronic acid dermal fillers, slower injection rates decrease the incidence of PIH and clinical bruising.
Management: supportive therapies such as ice, Arnica and time.
In patients of color, hyperpigmentation is a primary concern. Use of HA dermal fillers in POC may result in:
-
- Purple discoloration – ecchymosis
- Brown discoloration – PIH
- Grayish-brown discoloration – Hemosiderin deposition
- Reddish-brown discoloration – Hypersensitivity reaction
Take Home Points: There is an increased risk of hyperpigmentation with serial injection and fast injections, as well as with hypersensitivity to Hyaluronic Acid.
If pigmentary changes occur, the most effective mechanism for treatment includes a combination of a topical lightening agent such as hydroquinone, consistent mineral sunscreen use and sun avoidance, and chemical peels (preferably salicylic acid or glycolic acid).
If the dyschromia is related to the hyaluronic acid filler, hyaluronidase may be necessary to dissolve the filler and resolve the post-inflammatory discoloration. Occasionally, persistent dyschromia may be the result of hemosiderin deposition in where Nd-Yag lasers would need to be considered for clearance.
Most importantly, avoid pigmentary changes by utilizing low risk methods of injection and implementing slow injection times.
References
-
- Pandya AG, Alexis AF, Berger TG, Wintroub BU. Increasing racial and ethnic diversity in dermatology: A call to action. J Am Acad Dermatol. 2016 Mar;74(3):584-7. doi: 10.1016/j.jaad.2015.10.044. Epub 2016 Jan 8. PMID: 26774427.
- Taylor SC, Burgess CM, Callender VD. Safety of nonanimal stabilized hyaluronic acid dermal fillers in patients with skin of color: a randomized, evaluator-blinded comparative trial. Dermatol Surg. 2009 Oct;35 Suppl 2:1653-60. doi: 10.1111/j.1524-4725.2009.01344.x. PMID: 19807760.
This information was presented by Dr. Cheryl Burgess at the 2021 Skin of Color Update virtual conference held on September 10-12, 2021. The above highlights from her lecture were written and compiled by Dr. Mojgan Hosseinipour.
Did you enjoy this article? Find more on Skin of Color Dermatology here.