The title of today’s broadcast: Practical Applications of Lasers and Energy-Based Modalities in Skin of Color. That is a mouth-full to basically tell us that we are getting the best tips to treat refractory medical and aesthetically-concerning conditions from 3 of dermatology’s foremost experts in skin of color: Dr. Eliot Battle, Dr. Cheryl Burgess, and Dr. Andrew Alexis.
WOW! We were in for a treat! We learned about patients with refractory melasma, post-inflammatory hyperpigmentation (PIH), acne scars, acne keloidalis nuchae, and vitiligo. Basically, these patients had nearly given up hope and lost self-esteem, then Drs Battle, Burgess, and Alexis turned their lives around.
Before I dive into the details, let me share with you my “Aha!” moments that really changed my mindset in using lasers to treat patients with darker skin types.
My “Aha!” Moments:
1. The 1064nm Nd:YAG may serve as a workhorse laser in treating many conditions in skin of color.
The 1064nm Nd:YAG offers the benefit of long wavelengths, which penetrate more deeply into the skin, and the ability to target melanin in the skin. It can be used for laser hair removal as well as for hyperpigmentation.
2. Teenagers can be treated with lasers, but their condition must be impacting their self-esteem and/or quality of life.
The patient must be bothered by the condition, not just their parent (although parental consent is required, of course). Better yet—we can treat WHILE a teenage or adult patient is on oral isotretinoin. Read on for these juicy details.
3. Multimodal treatment seems to be best.
Based on the cases presented to us by the panel of experts, each one of the patients with refractory scars/discoloration benefited not only from multiple sessions of laser or energy-based therapy but also with a consistent topical and/or chemical peel regimen. A long list of agents can be used for bleaching, lightening, protecting, and moisturizing the skin— not everyone has to use hydroquinone! These seem to be integral to successful treatment.
On to the cases presented by our expert panel:
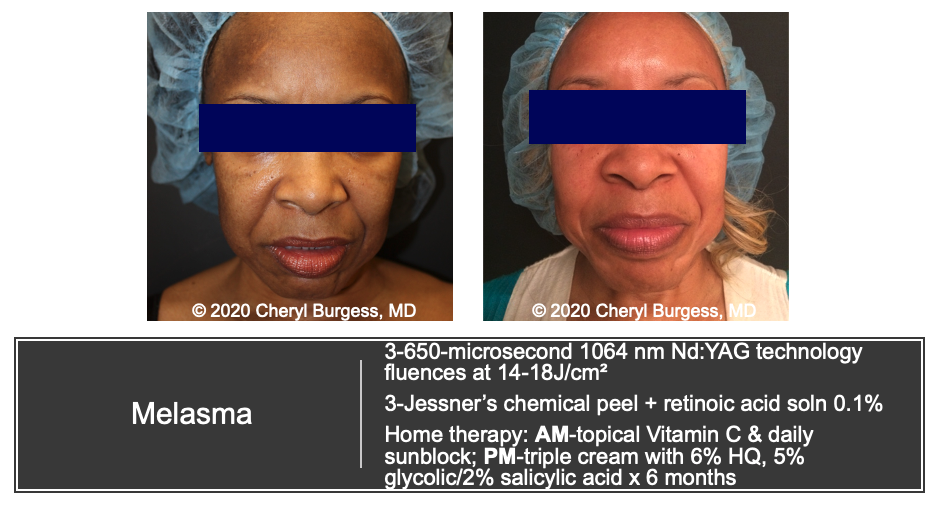
Dr. Burgess presented two cases: refractory melasma and a case of IPL (intense pulsed light) laser hair removal gone wrong (don’t worry—she’s the one that fixed it)
Case 1: Refractory melasma
This first case is a patient with refractory melasma. She had tried a long list of topical therapies, including hydroquinone, but Dr. Burgess saved the day with:
Alternating regimen of:
-
- 1064nm Nd:YAG (750ms at fluences of 14-18J/cm2) AND
- Jessner’s chemical peel with retinoic acid solution. Each was performed 3 separate times.
A home topical regimen of:
-
- Topical vitamin C
- Sunblock
- Triple combination cream with 6% Hydroquinone (+ retinol and topical steroid)
- A facial pad impregnated with 5% glycolic acid/2%salicylic acid. —I wasn’t familiar with this OTC combined glycolic acid/salicylic acid product—see an example photo above.
See the patient’s amazing results below.
Case 2: IPL burns
Unfortunately, this poor patient underwent a botched attempt at laser hair removal—she got 1st and 2nd-degree burns—Ouch! (FYI: IPL is basically a no-no for darker skin types, aka Fitzpatrick skin types 4 and above). The procedure left multiple rectangular, brown patches of hyperpigmentation on her abdomen. Dr. Burgess saved the day by performing the following:
Alternating sessions of:
-
- 650 microsecond 1064 Nd:YAG with fluences of 14 J/cm2
- 1927 nm Fractionated thulium laser
- Jessner’s chemical peel
A home regimen of:
-
- Triple combination cream containing 6% Hydroquinone (remember these creams consist of hydroquinone + retinol + steroid)
Dr. Battle then shared the spotlight by presenting patients who really got the million-dollar makeover (figuratively speaking) from his Washington, DC-based office.
Case 3: Acne with all the issues
This was a teenager who had the trifecta:
-Unwanted facial hair
-Teenage acne
-Post-inflammatory hyperpigmentation (picking, acne, ingrown hairs)
Now, this case really had the wow factor. Dr. Battle brought out all of the tricks in his bag: laser hair removal, oral isotretinoin, topical antibiotics, and more. Before I dive into the details…look at the before and after picture below:
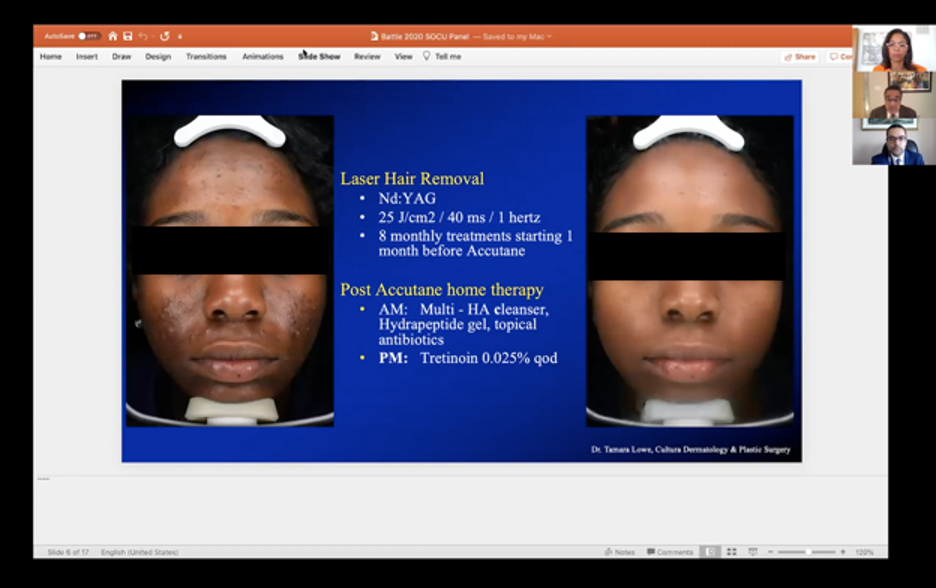
Who wouldn’t want their skin to look like this? “Pimple-faced” teenager no more! But caution, we don’t just treat any teenager. To treat a teenage patient, we should engage in careful consideration and assessment of the patient’s (not mom’s) impairment in quality of life, including distress from appearance. The patient must be bothered by their condition and want to undergo treatment. Parental consent is required, of course.
So here are the details of Dr. Battle’s regimen:
PART 1:
-
- Laser hair removal
- 20 weeks of therapy with Accutane
- Topical: multi-hyaluronic acid cleanser, topical antibiotic, hydrapeptide gel (gotta moisturize that beautiful face)
PART 2: (after Accutane)
-
- Multi-hyaluronic acid cleanser, topical antibiotic, hydrapeptide gel
- Added tretinoin 0.025% cream
Hold on… hold on… did you say laser hair removal WHILE on Accutane? This must be a “no-no”….incorrect, this is a MYTH!
Per the 2017 ASDS Guidelines Task Force, there is insufficient evidence to justify delaying procedures such as superficial chemical peels, nonablative lasers, and nonablative fractional devices1. Superficial and focal dermabrasion may be okay when performed by a well-trained clinician. This means we don’t need to wait to treat textural changes, dyspigmentation, and more while a patient is on oral isotretinoin.
Now back to the case: Look at this GLOW UP!
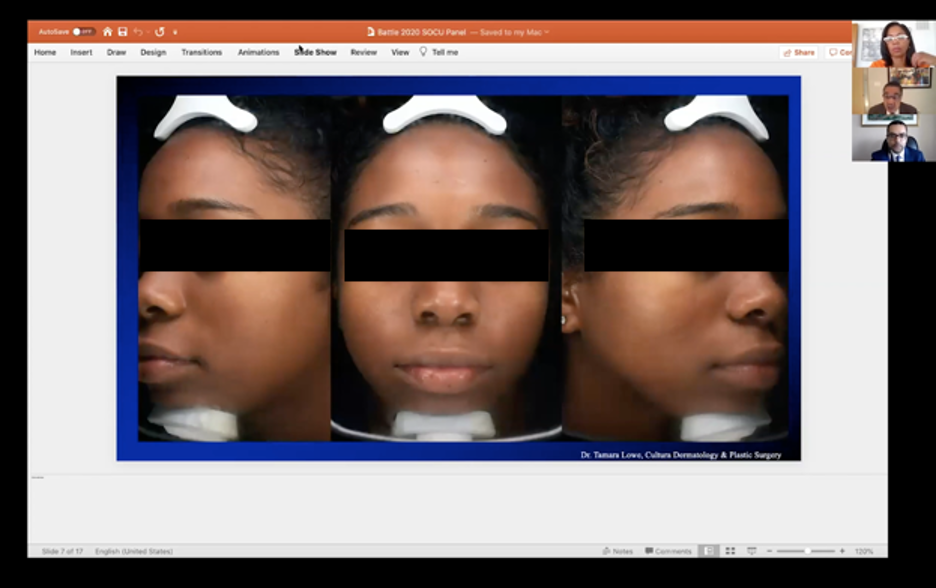
Honestly, these pictures make me think miracles are possible. One huge win for Dr. Eliot Battle and this patient.
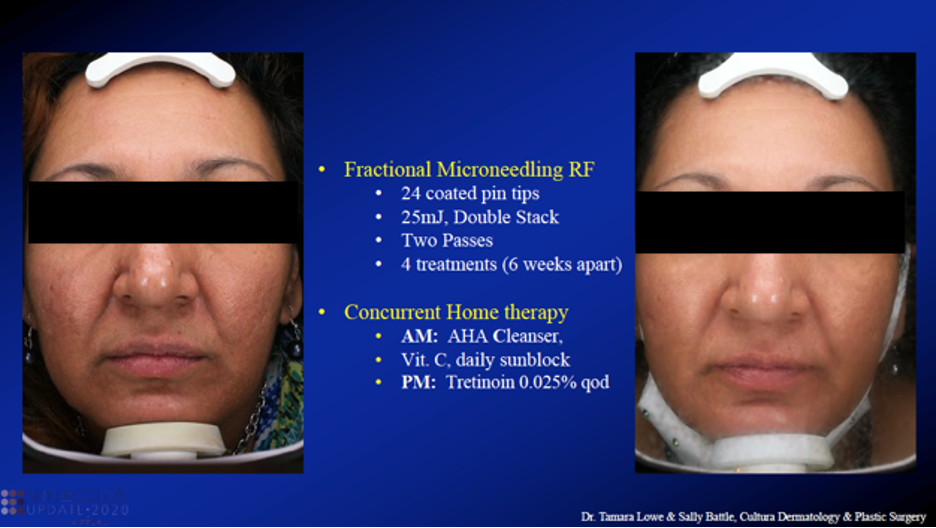
Case 4: Acne Scars for life—no more!
This was a 48-year-old woman with ice pick and boxcar acne scars.
Dr. Battle treated this patient with Fractional Microneedling Radiofrequency (RF). Dr. Battle provided SO many wonderful deets on this new device with coated pin tips. See the before and after photos and treatment regimen below.
Now for lesson #1 of the day:
Fractional Microneedling Radio Frequency 101
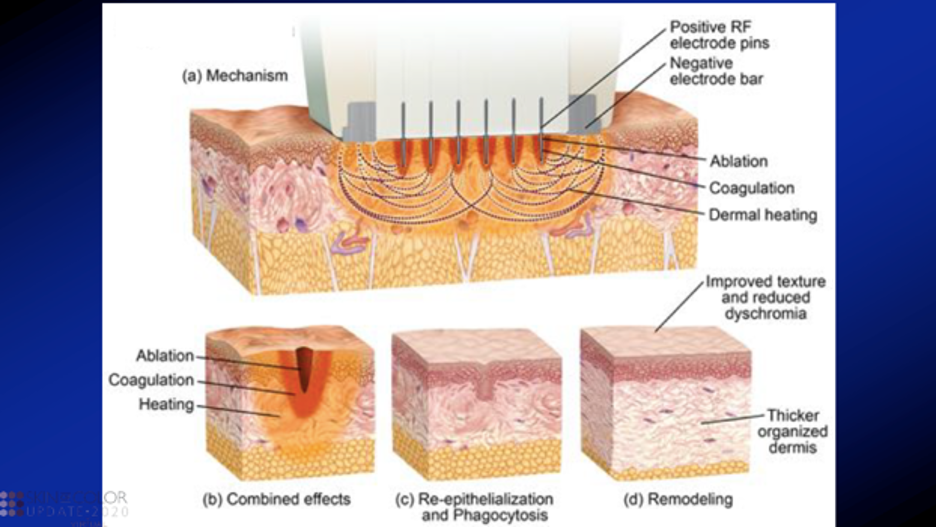
How does Fractional Microneedling Radiofrequency work?
It improves texture, discoloration, and scars by a controlled electromagnetic system in the skin that causes ablation, coagulation, and resultant skin remodeling. Microneedling by itself induces collagen production, however, fractional radiofrequency microneedling adds the element of heat-induced damage to the skin. When the dermis reaches a certain temperature, collagen denatures, and the surrounding tissue contracts. On histologic analysis, there is increased collagen deposition by upregulated transforming growth factor-beta (TGF-ß) and decreased inflammatory markers such as nuclear factor-kB and interleukin-82.
Radiofrequency microneedling is chromophore blind. It causes nonselective tissue heating. This means that it does NOT target a specific chromophore, thus can be considered safe in all skin types when used by a trained professional.
Side effects can include pain, erythema, edema, and PIH (although we try to avoid this with coated tips). Apparently, RF microneedling can also improve active inflammatory lesions of acne as well as wrinkles and laxity of the skin.
What magic actually happens inside this device?
Fractional Microneedling RF devices are new! Radiofrequency is part of an electromagnetic energy spectrum. Kinetic energy from flowing electrons is converted to thermal energy—the electrons flow from the positive electrode in the RF pins to the negative electrodes placed on the sides of the device (see the figure below from Dr. Battle’s slides). Heat then causes controlled damage to skin tissue and this resultantly triggers a natural healing mechanism (neocollagenesis and neoelastogenesis). After healing and remodeling occur, the patient has improved skin texture, reduced dyschromia, and a thicker dermis.
What does it mean to have coated tips?
Radiofrequency microneedling devices can come in two flavors: insulated (coated) or non-insulated. Non-insulated needles deliver heat through the entire length of the needle, whereas insulated needles deliver heat only at the needle tip (in the epidermis).
The coated needles are key for skin of color! We want to minimize heat and resultant thermal damage in the epidermis (this can cause hyper and hypopigmentation). If we use coated tips (e.g. silicone-coated tips), less heat is conducted to the epidermis. This is considered “epidermal sparing.”
Moving the spotlight to Dr. Alexis. He also gave us two great examples of how he used laser to improve two patients’ lives.
Case 5: Acne Keloidalis Nuchae that wouldn’t quit
This was a 36-year-old with Acne Keloidalis Nuchae (AKN) for over 10 years. His previous therapies included topical steroids, intralesional steroids, and liquid nitrogen. Despite these treatments, he had a large area of scarring alopecia which was itchy and often bled. Dr. Alexis changed the game by treating this patient with 3 sessions of fractional nonablative 1550nm Erbium-doped laser followed by transdermal and intralesional triamcinolone 40mg/mL. He continued treatment with topical clobetasol gel twice daily, two weeks on and two weeks off. Check out the patient’s before and after photos below!

Lesson #2 of the day:
Why use a laser for AKN?
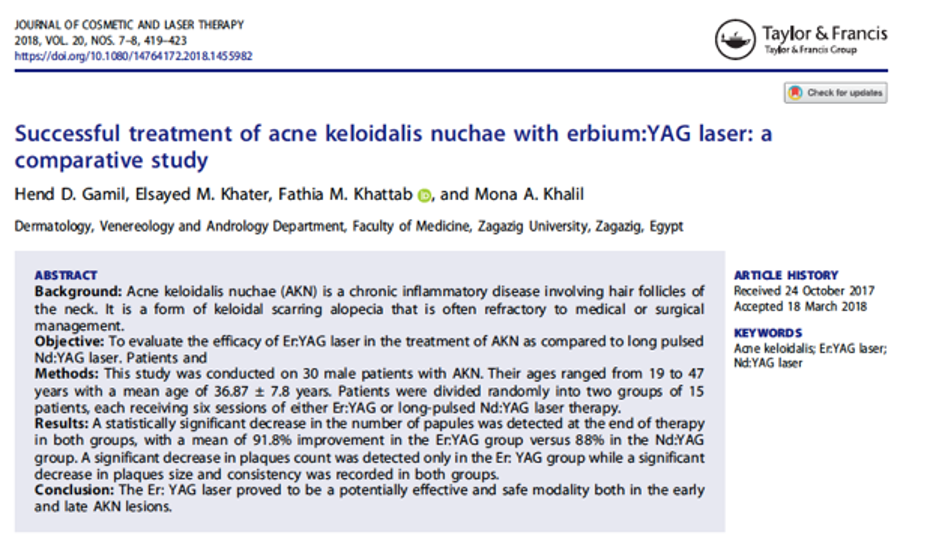
Long pulsed Nd:YAG, long-pulsed Alexandrite, and other lasers have been reportedly effective in treatment of AKN3. Unfortunately, Alexandrite lasers are typically not the best option for our patients with darker skin types. A 2018 study out of the Journal of Cosmetic and Laser Therapy compared 15 patients with AKN treated with Erbium Yag vs 1064nm long-pulsed Nd:YAG laser (see the photo below)4. Both groups showed improvement in the number of papules and plaque size and consistency. The Erbium YAG showed a statistically significant decrease in the number of plaques after treatment whereas the long-pulsed Nd-Yag did not. Dr Alexis stated that the erbium:YAG resurfacing laser may have some advantage over the Nd:YAG for the larger plaque-type presentations of AKN. Further, the long-pulsed Nd:YAG may result in hair removal, which would not have been ideal in this patient’s case because his keloidal-like plaque was in the center of his occipital scalp.
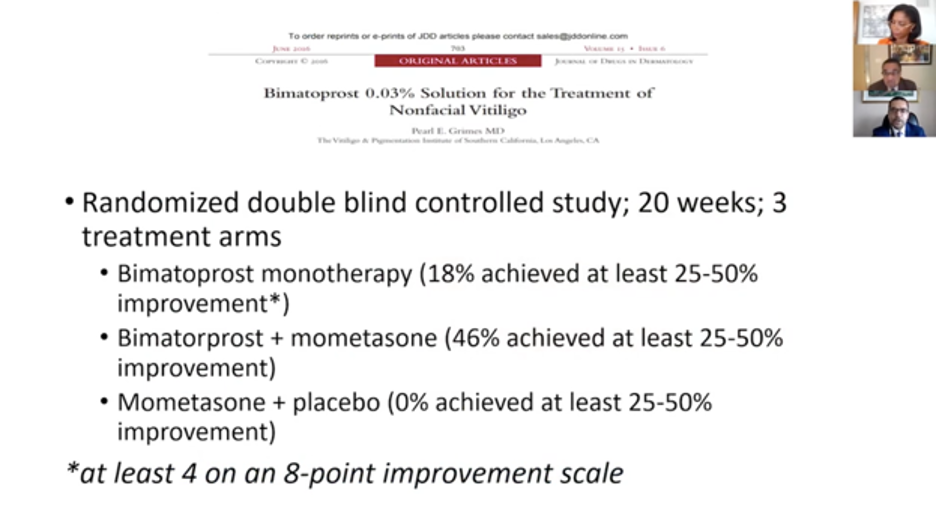
Case 6: Vitiligo without hope
Dr. Alexis next featured a 40-year-old African American female who was told to “give up” on her vitiligo. She came to Dr. Alexis as a last resort when her vitiligo began rapidly spreading on the face. In these cases, we would think about topical or systemic corticosteroids, topical or oral janus kinase inhibitors, and phototherapy. Unfortunately, this patient had some baseline health concerns that prohibited her from the above therapies, making her a perfect candidate for laser therapy (excimer laser that is…). Dr. Alexis highlighted articles focusing on various topical therapies for vitiligo, including topical tacrolimus plus narrowband UVB as well as bimatoprost. Yes, bimatoprost (I guess I haven’t heard of this one much! Maybe it’s because of the cost)5,6. Bimatoprost is a prostaglandin F2a synthetic analog and it is currently FDA approved for the treatment of glaucoma and elevated intraocular pressure (0.01% concentration) as well as for the treatment of eyelash hypotrichosis (i.e., Latisse, Allergan plc, at its 0.03% concentration). Regarding vitiligo, studies have shown that prostaglandins released from ultraviolet exposure cause an increase in the size and number of active melanocytes as well as the number of melanosomes transferred to keratinocytes7. A proof-of-concept study was conducted by vitiligo expert and skin of color dermatology extraordinaire Dr. Pearl Grimes comparing bimatoprost 0.03% solution monotherapy versus bimatoprost + mometasone vs mometasone + placebo6. After 20 weeks of therapy, the combination group achieved the greatest response and the bimatoprost came in second. Interestingly, the mometasone only group underperformed compared to bimatoprost monotherapy. See Dr. Alexis’ slide below.
In Dr. Alexis’ case, he utilized a multimodal approach: Excimer laser therapy + topical tacrolimus + topical bimatoprost. The patient committed to this treatment for a year with twice a week excimer laser as consistently as she possibly could.
Now onto questions from the audience:
1. Can we treat ochronosis with lasers?
Dr. Burgess provided some helpful insight into this question. First of all, we must manage patient expectations regarding the refractory nature of ochronosis. Second, we don’t have to use a laser to treat this condition. Dr. Burgess’ laser of choice is the short pulse, high-intensity 650-microsecond laser. Remember that other “lightning” treatments can be used such as kojic acid, niacinamide, and others without having to use a bleaching agent like hydroquinone. Dr. Battle also reminded us that we can use almost any long-pulse Nd:YAG laser and convert pulse durations to microsecond pulses by changing the settings. There are newer devices today, however, that are solely microsecond lasers.
2. For patients with scarring hair loss (specifically Dr. Alexis’ patient with AKN) should we consider hair tattoos?
Dr. Alexis was not too excited about using permanent hair tattoos on his patient. Here’s why:
-
- This is permanent and cannot be undone. That just means the patient has to carefully weigh out the pros and cons of getting a tattoo.
- What will happen when the patient’s other hair turns gray with age? He will have to commit to dying his hair black for the rest of his life.
- Maybe consider nonpermanent options instead, such as topical camouflaging agents. Check out a picture
 of hair fiber above, which can be used to conceal areas of thinned hair.
of hair fiber above, which can be used to conceal areas of thinned hair.
3. What is the risk of burning the skin with laser hair removal during Accutane use?
The risk of burning with laser hair removal is the same regardless of whether the patient is on Accutane.
We just don’t have the data to support that Accutane increases the risk of adverse events compared to patients receiving the same treatment, not on Accutane. Studies thus far have shown that Accutane does not increase the risk of adverse events with lasers. Thus, there is no increased sensitivity of the skin in Accutane patients when considering laser parameters. We should always be cognizant of what condition we are treating and the patient’s skin type to ensure we minimize adverse effects.
4. Can you use tetracyclines with lasers?
Yes. Most topical or oral antibiotics are okay for use with lasers.
“Which laser is best?”
Unfortunately, our experts can’t offer “which laser is best” because this was a lecture for CME credit and name dropping is not allowed…sigh. Don’t worry, you can email them personally and they would be happy to answer any and all questions you have! Thank goodness for that! What a wonderful discussion this was.
How often do you treat skin conditions with laser in those with darker skin types?
Have any pearls on non-permanent hair camouflage that you would like to share?
Please share your comments at the end of this post, and on Instagram @nextstepsinderm!
References
-
- Waldman A, Bolotin D, Arndt KA, Dover JS, Geronemus RG, Chapas A, Iyengar S, Kilmer SL, Krakowski AC, Lawrence N, Prather HB, Rohrer TE, Schlosser BJ, Kim JYS, Shumaker PR, Spring LK, Alam M. ASDS Guidelines Task Force: Consensus Recommendations Regarding the Safety of Lasers, Dermabrasion, Chemical Peels, Energy Devices, and Skin Surgery During and After Isotretinoin Use. Dermatol Surg. 2017 Oct;43(10):1249-1262. doi: 10.1097/DSS.0000000000001166. PMID: 28498204.
- Alessa D, Bloom JD. Microneedling Options for Skin Rejuvenation, Including Non-temperature-controlled Fractional Microneedle Radiofrequency Treatments. Facial Plast Surg Clin North Am. 2020 Feb;28(1):1-7. doi: 10.1016/j.fsc.2019.09.001. PMID: 31779933.
- Tawfik A, Osman MA, Rashwan I. A Novel Treatment of Acne Keloidalis Nuchae by Long-Pulsed Alexandrite Laser. Dermatol Surg. 2018 Mar;44(3):413-420. doi: 10.1097/DSS.0000000000001336. PMID: 29016541.
- Gamil HD, Khater EM, Khattab FM, Khalil MA. Successful treatment of acne keloidalis nuchae with erbium:YAG laser: a comparative study. J Cosmet Laser Ther. 2018 Nov-Dec;20(7-8):419-423. doi: 10.1080/14764172.2018.1455982. Epub 2018 May 14. PMID: 29757041.
- Chang HC, Sung CW. Efficacy of combination therapy of narrowband-ultraviolet B phototherapy or excimer laser with topical tacrolimus for vitiligo: An updated systematic review and meta-analysis. Photodermatol Photoimmunol Photomed. 2020 Jul 12. doi: 10.1111/phpp.12593. Epub ahead of print. PMID: 32654300.
- Grimes PE. Bimatoprost 0.03% Solution for the Treatment of Nonfacial Vitiligo. J Drugs Dermatol. 2016 Jun 1;15(6):703-10. PMID: 27272076.
- Friedmann PS, Gilchrest BA. Ultraviolet radiation directly induces pigment production by cultured human melanocytes. J Cell Physiol. 1987;133:88-94.
This information was presented by Drs. Andrew Alexis, Eliot Battle, and Cheryl Burgess during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Dr. Jacqueline McKesey.
Did you enjoy this article? Find more on Skin of Color topics here.

