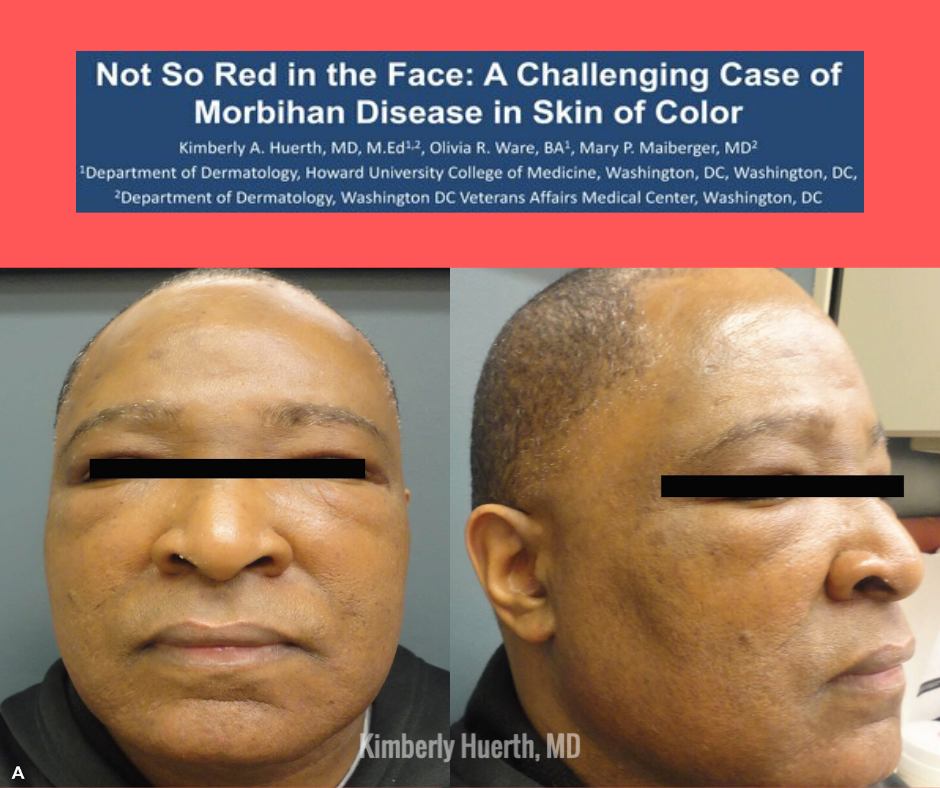
Morbihan Disease (MD) is a rare condition but can be a very rewarding diagnosis to make. I interviewed Dr. Kimberly Huerth on her poster presentation of an African-American man with long-standing, progressive Morbihan Disease that took 16 years to diagnose. MD in patients of skin of color may be underreported as well as underdiagnosed. Similarly, rosacea in skin of color is often overlooked and this patient’s clinical story may have started with rosacea and then progressed to MD. Therefore, it is extremely important to highlight such cases as this to show disorders not commonly seen in skin of color. In this interview, Dr. Huerth discusses the clinical clues that led to her diagnosis and the treatment and management for this patient.
Poster Title: Not So Red in the Face: A Challenging Case of Morbihan Disease in Skin of Color
-
Your patient had Morbihan Disease (MD) and MS. Have you seen in the literature any associations with Morbihan Disease and autoimmune diseases?
This was my first case of Morbihan disease, so I did not know much about it before I started researching it in an attempt to better manage my patient. I knew going into it that rosacea and acne had been implicated in the pathogenesis of MD, but that was about it. Since MD is an uncommon condition, I don’t think that anyone has examined disease associations with large cohorts of patients. Interestingly though, there was a study published in JAAD in 2015 that identified an association in a large cohort of Danish women between rosacea and certain autoimmune diseases such as multiple sclerosis, celiac disease, rheumatoid arthritis, and type I diabetes.1 So if we assume that MD emerges from longstanding rosacea, then maybe it is possible to stretch the transitive property to say that if rosacea and MS are associated, and MD is engendered by rosacea, then MD and MS may in some way be related. But this is just me going down the rabbit hole—I’ve never seen an association between MD and MS published anywhere.
-
Since MD is a disease of exclusion and considered to be underreported and underdiagnosed especially in skin of color, what were some of the clinical clues that allowed you to make the diagnosis?
Although there are several other conditions that can present with facial swelling, I think the uniform non-pitting edema of the upper 2/3 of the face is very characteristic of MD, so the patient’s striking appearance was the strongest clinical clue that I had to go off of. In fact, as soon as I saw him in the waiting room, his face immediately reminded me of a photograph of a patient with MD that I had come across in a dermatology textbook at some point previously. I hadn’t even stopped to read about Morbihan disease at that time, I just remembered the photograph. In addition to my patient’s clinical appearance, there were several elements of his history that also supported the diagnosis. The swelling had an insidious onset and progressed slowly over the course of 16 years, and it had been preceded by several years of his face feeling intermittently “hot and flushed.” He also reported an occasional grit-like sensation in his right eye while all of this was taking place. Given the patient’s comorbid MS, it is not possible to say with absolute certainly whether these symptoms were MS related, rosacea related, or perhaps a bit of both. But after our work up to investigate other causes of facial swelling did not return any hits, we settled on the assumption that longstanding, undiagnosed and untreated rosacea engendered his MD.
-
What is the mechanism or thought process regarding using antibiotics (ex: doxycycline) and isotretinoin for treatment? Are they thought to be anti-inflammatory?
We don’t really know why drugs like isotretinoin and doxycycline work, since the etiology and pathogenesis of MD is not completely understood. It has been suggested that vasodilation and chronic inflammation in the setting of rosacea and/or acne results in increased vascular permeability and fluid transudation, and ultimately dermal remodeling and fibrosis which obstructs facial lymphatic drainage. It is thought that isotretinoin’s immunomodulatory and anti-inflammatory properties may improve MD in the same way that it has been shown to improve rosacea.2 Additionally, vitamin A and other retinoids have been shown to inhibit fibroblast proliferation and migration, as well as the production of various connective tissue elements, including type I and III collagen, in vitro.3 It may hence be that isotretinoin is able to counteract some of the dermal changes wrought by longstanding rosacea, and restore the ability of the lymphatics to drain the face. But again, this is what we think, not necessarily what we know.
-
Since MD is often considered to be in the setting of rosacea, did the clinical team consider using ivermectin to treat? Or would there be any indication to use ivermectin to treat MD?
I have not seen any reports in the literature of ivermectin being used to treat MD, although it may be a prospect worth considering. Activation of immune-mediated inflammatory pathways is thought to be central to the pathogenesis of rosacea, and Demodex mites have been proven capable of secreting bioactive molecules that affect the immune reactivity of sebocytes, specifically in the realm of TLR signaling and IL-8 secretion.4 It has also been suggested that the waste products of Demodex mites may stimulate the innate immune system and/or contribute to the formation of a delayed hypersensitivity reaction.5 There are also theories that bacteria carried by Demodex mites play a role in the pathogenesis of rosacea. Bacillus oleronius is a gram negative bacterium that has been isolated from Demodex mites. Proteins from B oleronius have been shown to activate neutrophils. It has thus been speculated that B oleronius released from dead Demodex mites into the pilosebaceous unit may leak proteins into the surrounding tissue that cause neutrophil chemotaxis, degranulation, and cytokine production, and ultimately lead at least in part to the inflammatory erythema and pustules observed in some rosacea patients.6 So it may very well be that there is a role for ivermectin, possibly as a therapeutic adjunct, in a subset of MD patients, perhaps those who have or at one time had the lesions of papulopustular rosacea. But if chronic inflammation and vasodilation lead to dermal remodeling which leads to MD, I would think that trying to address the fibrotic changes in the dermis would be a treatment priority.
-
What is the long-term clinical follow up for this patient with MD?
The patient’s history of MS, and the many medications that he has had to take to try to manage it, have made him a bit reluctant to pursue aggressive treatment of his MD, despite the fact that he is greatly bothered by it. After trialing him on doxycycline 100 mg BID for a few months without any improvement, the patient was initiated on isotretinoin 20 mg daily. We have since been limited to this low daily dose as a result of side effects such as mild gastrointestinal upset and fatigue, as well as the patient’s wish to proceed cautiously. Prednisone can be combined with isotretinoin, in some cases with very good effect, but we did not incorporate it into our patient’s regimen because it had not improved his facial swelling when he was taking it for MS, and because he wished to avoid polypharmacy. Despite going low and slow with isotretinoin, the patient believes that his facial edema has improved somewhat as a result of treatment, though progress has been very gradual. The plan for now is to continue with isotretinoin as long as he continues to evince signs of improvement, consider taking a break once we get there, and tailoring his future therapy to what his symptoms, needs, and preferences are at the time.
About the Author:
 Kimberly Huerth, MD, M. Ed is a Chief dermatology resident at Howard University in Washington DC. She received her medical degree from the State University of New York at Buffalo. Dr. Huerth also possesses two Master’s degrees in Education, from the University of Massachusetts and Northeastern University, which she earned prior to medical school while serving as an educator for the Boston Public Schools. Dr. Huerth has presented her work at numerous local and national conferences and has published in several widely read dermatology journals. Her clinical interests include cosmetic dermatology, hair disorders, and dermatologic surgery. She is an active member of the Women’s Dermatological Society and enjoys participating in their community outreach events. Closer to home, she volunteers for the Humane Rescue Alliance in Washington DC (adopt don’t shop!).
Kimberly Huerth, MD, M. Ed is a Chief dermatology resident at Howard University in Washington DC. She received her medical degree from the State University of New York at Buffalo. Dr. Huerth also possesses two Master’s degrees in Education, from the University of Massachusetts and Northeastern University, which she earned prior to medical school while serving as an educator for the Boston Public Schools. Dr. Huerth has presented her work at numerous local and national conferences and has published in several widely read dermatology journals. Her clinical interests include cosmetic dermatology, hair disorders, and dermatologic surgery. She is an active member of the Women’s Dermatological Society and enjoys participating in their community outreach events. Closer to home, she volunteers for the Humane Rescue Alliance in Washington DC (adopt don’t shop!).
References
- Egeberg A, Hansen PR, Gislason GH, Thyssen JP. Clustering of autoimmune diseases in patients with rosacea. J Am Acad Dermatol. 2016;74(4):66-672.e1.
- Plewig G, Nikolowski J, Wolff HH. Action of isotretinoin in acne rosacea and gram-negative folliculitis. J Am Acad Dermatol. 1982;6(4):766-785.
- Hein R, Mensing H, Müller PK, et al. Effect of vitamin A and its derivatives on collagen production and chemotactic response of fibroblasts. Br J Dermatol. 1984;111(1):37-44.
- Lacey N, Russell-Hallinan A, Zouboulis CC, Powell FC. Demodex mites modulate sebocyte immune reaction: Possible role in the pathogenesis of rosacea. Br J Dermatol. 2018;179(2):420-430.
- Bevins CL, Liu F. Rosacea: Skin innate immunity gone awry? Nat Med. 2007;13(8):904-906.
- O’Reilly N, Bergin D, Reeves EP, McElvaney NG, Kavanagh K. Demodex-associated bacterial proteins induce neutrophil activation. Br J Dermatol. 2012;166(4):753-760.
Photo Credits: All images courtesy of Kimberly Huerth, MD
Did you enjoy this post? Find more on Skin of Color topics here.