Pigmentation is key to photoprotection of the skin, eye color, and enhanced barrier function. With increased pigmentation, photoaging is minimized with a concurrent decrease in frequency of skin cancer. In skin of color, these pigmentary advantages come at a cost. These include an increased risk of hyperpigmentation and/or hypopigmentation, hypertrophic scars, keloids, scarring alopecia, and vitamin D deficiencies.
Hence, individuals with skin of color often develop disorders of hyperpigmentation or hypopigmentation, which can cause significant emotional distress. At the 2020 Skin of Color Virtual Update, Dr. Pearl Grimes highlighted characteristics of disorders of pigmentation with an emphasis on diagnostic considerations. Dr. Grimes emphasized that a detailed history and physical exam are key and offer clues to the appropriate diagnosis. Important parameters to consider include age of onset, family history, location as well as the nature of lesions.
Throughout her lecture, Dr. Grimes highlighted key disorders of hypopigmentation and hyperpigmentation, common to skin of color. Few of them may present a diagnostic challenge. For example, post-inflammatory hyperpigmentation (PIH) may be confused with melasma. This distinction is important because she stated we cannot cure melasma in contrast to PIH. However, it is important to make the distinction as, like melasma and PIH, pigmentation disorders vary in clinical course and treatment.
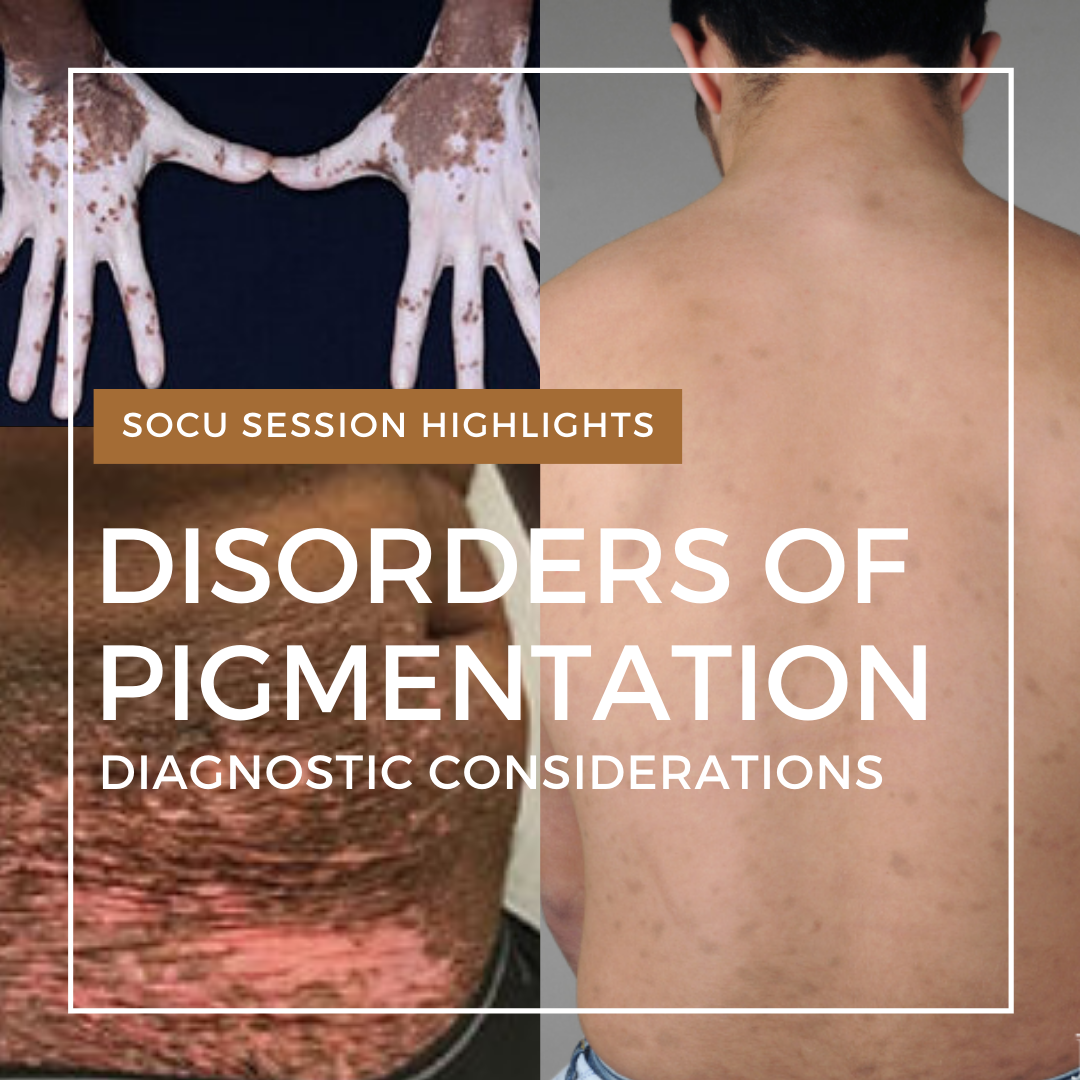
Disorders of hypopigmentation highlights
Vitiligo
-
 Autoimmune disease mediated by aberrations in the interferon-JAK-STAT chemokine pathway.
Autoimmune disease mediated by aberrations in the interferon-JAK-STAT chemokine pathway.- CD8 lymphocytes migrate into the skin where they release interferon-gamma which activates the JAK-STAT pathway. Following activation of the pathway, chemokines 9 and 10 recruit additional CD8 lymphocytes into the skin. These CD8 lymphocytes are key players in mediating the destruction of melanocytes.
- Segmental vitiligo occurs in a unilateral/ or dermatomal distribution. It is more common in childhood. In 90% of the cases, it burns out in a year and does not progress. In the remaining 10%, it may co-exist with the generalized form. Segmental vitiligo is the only type of vitiligo where autologous grafting may be curative.
Nevus depigmentosus
-
- Wood’s lamp examination shows off white appearance.

- Biopsy will show normal melanocyte count as the defect is in the inability to transfer pigment from melanocytes to keratinocytes.
- May expand as the patient gets older.
- Wood’s lamp examination shows off white appearance.
Hypopigmented mycosis fungoides
-
 Disseminated, hypo-pigmented atrophic, and subtle scaly patches.
Disseminated, hypo-pigmented atrophic, and subtle scaly patches.- Affect the trunk, upper and lower extremities.
- Characteristic histology reveals Pautrier microabscesses.
Idiopathic guttate hypomelanosis
-
 Higher incidence in women.
Higher incidence in women.- Classic, hypopigmented punctate macules, usually on lower extremities however other sites may be affected.
- Difficult to treat. Dr. Grimes does not recommend any treatment as none are optimal.
- Cryotherapy, superficial dermabrasion, topical retinoids, tacrolimus, pimecrolimus, non-ablative fractional lasers, 5-Fluorouracil have all been tried to varying success.
Progressive Macular Hypomelanosis
-
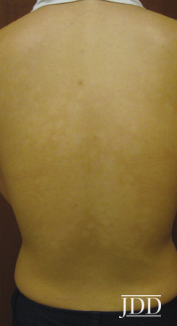 Due to subspecies of Propionibacterium acnes (now Cutibacterium): phylogenetic Type III
Due to subspecies of Propionibacterium acnes (now Cutibacterium): phylogenetic Type III
-
-
- acnes cultured from lesional skin
- C. acnes identified via real-time PCR
-
-
- Lesions demonstrate red follicular fluorescence of lesional skin under Wood’s lamp examination.
- Decreased melanin formation and decreased melanization of melanosomes.
Disorders of Hyperpigmentation highlights
Post-inflammatory hyperpigmentation
-
- Most commonly due to acne; can also be triggered by drug reactions, atopic dermatitis, or psoriasis.
- Histology notable for increase in melanin production, increase in melanocytes, melanin Incontinence, melanophages.
Melasma
-
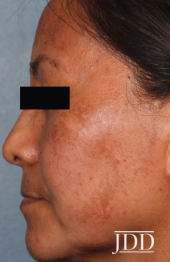 1% of the general population, 9-50% of high-risk population.
1% of the general population, 9-50% of high-risk population.- Age of Onset 30-34.
- Family History 30-64%.
- Precipitating Factors: Sun exposure, a lot of data now on visible light as an exacerbating factor, lack of sunscreen, Pregnancy, BCP’s, Hormone Replacement.
- Malar, centrofacial most common patterns.
- Extra facial melasma most common in post-menopausal women.
- Pathogenesis: most data suggest that it is a phenotype of photodamage.
-
-
- Altered barrier function, expression c-kit, stem cell factor 19.
- Increase in: melanogenesis, solar elastosis, dermal blood vessels, expression of VEGF, mast cells, and lesional α-MSH.
- Altered barrier function Expression c-kit, stem cell factor.
-
Erythema Dyschromicum Perstans
-
 Histology:
Histology:
-
- Vacuolar degeneration of basal cells.
- Dermal melanosis.
- Perivascular lymphohistiocytic infiltrate.
-
- Differential diagnosis is lichen planus pigmentosus.
- 48% of patients have a positive Patch test.
- Possible triggers include nickel sulfate, colophony, potassium dichromate, balsam of Peru, PPD, Fragrance mix, Paraben mix.
- Treatments: topical calcineurin, topical steroids. There is some recent data for Accutane.
Final thoughts
-
- Pigmentation disorders disproportionately affect skin of color.
- A detailed history and physical exam are crucial for appropriate diagnosis and treatment.
This information was presented by Dr. Pearl Grimes during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Cula Dautriche.
All images courtesy of the Journal of Drugs in Dermatology.
Did you enjoy this article? Find more on Skin of Color here.