Hair is part of our identity and hair loss is therefore particularly distressing to patients. With so many potential causes of hair loss, our expertise as dermatologists is desperately needed, especially among pediatric patients where hair loss can be even more concerning to patients and their parents. To help us examine, diagnose, and counsel pediatric patients with hair loss, we were lucky to have a lecture by Dr. Candrice Heath at the 2021 Skin of Color Update, titled “Hair Loss in Pediatric Patients with Skin of Color.” Dr. Heath, Assistant Professor and Director of Pediatric Dermatology at Lewis Katz School of Medicine at Temple University and active participant on social media @DrCandriceHeath, channeled her triple board certification (pediatrics, dermatology, and pediatric dermatology) to give us a wonderful lecture with many clinical pearls about how to identity common hair/scalp disorders in children with skin of color and approach counseling with cultural humility.
Dr. Heath started with a slide stating, “No lean in exam!”1 This means that we must get right in there and thoroughly examine our patient’s scalp and hair. Importantly, we also need to perform the exam with culture humility.1 To do this, Dr. Heath first asks parents to remove any hair ties or bows, which allows her to see how the hair is handled and the relationship between the parents and child. She then examines the patient along with the parents, pointing out exam findings contributing to her diagnosis.
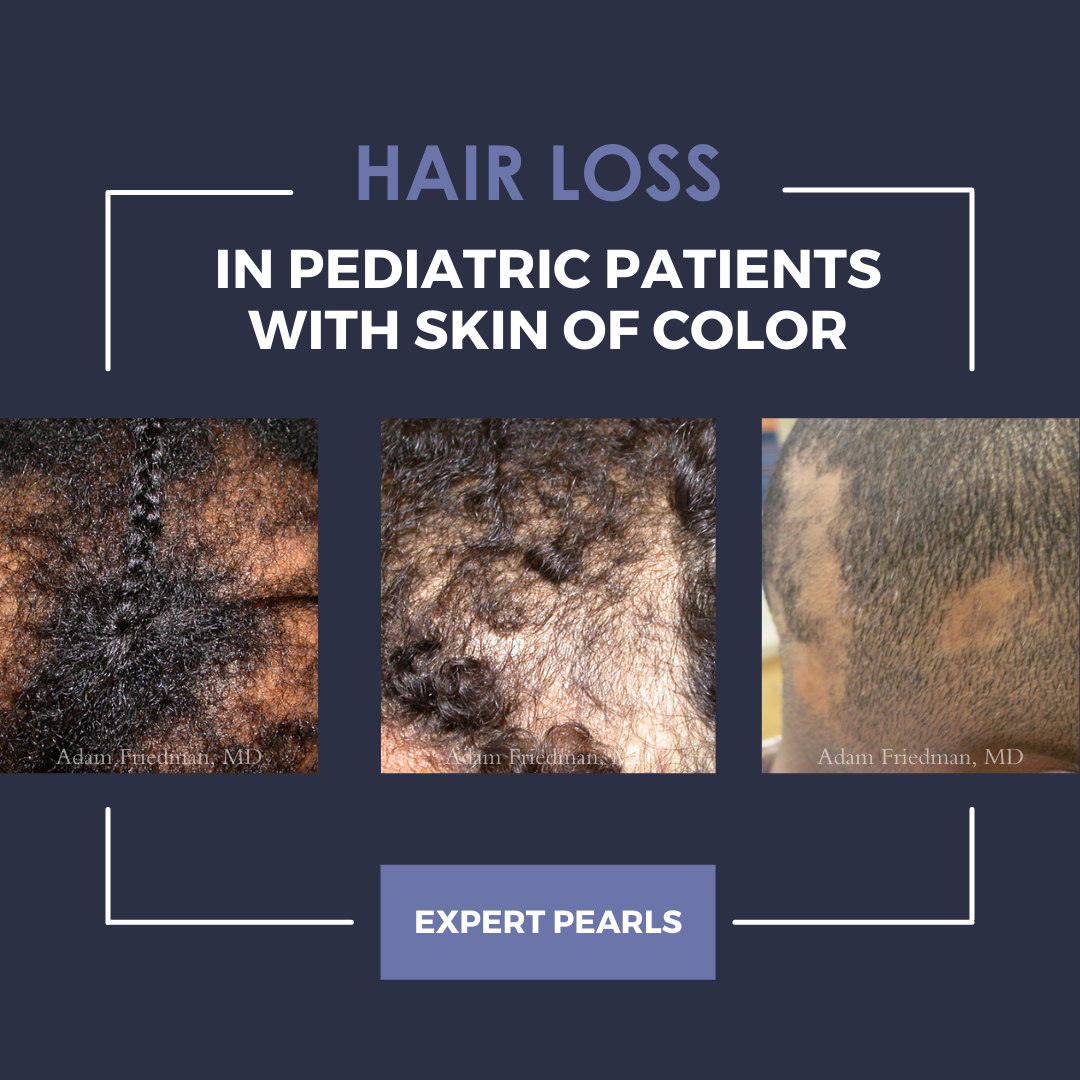
After describing how to approach pediatric patients, we dived into three common causes of hair loss along with their presentation and treatment options: traction alopecia, tinea capitis, and central centrifugal cicatricial alopecia (CCCA).
Traction alopecia
Traction alopecia is a common condition in pediatric patients presenting with pustules in high tension areas and the hair fringe sign, or retained hairs along the frontal scalp.2 While “baby hairs” can be normal in pediatric patients, it is important to at least consider traction alopecia when you see these hairs.2 Adult patients with traction alopecia will often present complaining of “thinning edges,” hair loss at scalp borders, or hair breakage, however, this may not be the case in children. 2 Pediatric patients may be in your clinic for other reasons when you notice signs of traction alopecia. Dr. Heath challenges you to still address this disease, especially because of the biphasic nature, where early disease is reversible with alteration of hair care practices but late disease can progress to permanent scarring.
After you make this diagnosis, similar to your exam, it is critical to counsel patients with humility using Dr. Heath’s three step method:3
-
- Compliment your patients’ hair. For instance say that you like the color of their barrettes or their pony tail.
- With parents at the bedside, discuss the exam findings together – show them the pustules, tension, or hair fringe sign, indicating that the hair may be pulled too tight.
- Suggest loosening the style, making it look 1-2 weeks old. You can also recommend removing hair adornments at night.
If you see teenagers with traction alopecia who have entered the scarring phase, topical and intralesional steroids are also helpful. For topical steroids, Dr. Heath typically starts with a Monday through Friday regimen and then spaces out use. Additionally, there are reports of topical minoxidil having increased absorption in children, so Dr. Heath uses this medication in select teen patients, but only at the low concentration (2% rather than 5%) and after discussion that the use is off-label.
Tinea capitis
Tinea capitis, or fungal infection of the scalp, can present in numerous ways. It can be seen with diffuse scale – this can be tricky as it resembles seborrheic dermatitis, but this disease does not occur in pre-pubertal children. An inflammatory variant can be seen in patients who will also complain of scalp pain and itching. Black dot tinea capitis indicates the broken hairs that occur with this infection. Finally, patients can present with annular plaques, which is the more classic variant. If you are suspicious of tinea capitis, the next step is to examine for occipital lymphadenopathy.
When you see clinical signs consistent with tinea capitis, the big question that comes to mind is should we treat or wait for a culture? Dr. Heath challenges you to trust your exam and treat! To convince you further, she shared a study of 100 children showing that in those with alopecia and occipital lymphadenopathy, 100% of cases had a positive culture.4 In patients with scaling and occipital lymphadenopathy, 96.7% of cases returned with a positive culture.4 Treatment options to choose from include:5–7
-
- Terbinafine for 4-6 weeks:
- 10-20 kilogram (kg): 62.5 milligrams (mg) /day
- 20-40 kg: 125 mg/day
- >40 kg: 250 mg/day
- Griseofulvin microsize for 8-12 weeks:
- 20-25 mg/kg/day
- Terbinafine for 4-6 weeks:
Both anti-fungal agents cover the most common organism, trichophyton tonsurans, as well as microsporum canis. The benefit of griseofulvin is its availability as a liquid, but because of resistance in the community, longer treatment duration is needed compared to terbinafine.
Central centrifugal cicatricial alopecia8,9
This scarring alopecia can begin in teenage years with simply hair breakage at the top of the scalp. Given more scarring (with permanent loss of hair follicles) occurs as time progresses with CCCA, we can save our patients’ hair by catching this early breakage!8 Treatment is similar to adults with CCCA, including anti-inflammatory agents such as doxycycline, topical steroids, and intralesional steroids.
In summary, to best care for pediatric patients with skin color, perform a thorough exam with cultural humility.1 Even if a patient is not presenting for hair loss, if you see signs of traction alopecia, have a conversation with the family before this disease progresses to the scarring phase. For tinea capitis, trust your exam and treat without confirmation when you see characteristic scalp disease with occipital lymphadenopathy. Finally, keep CCCA on your radar for teenage patients, especially when they mention early hair breakage of the vertex scalp. With this helpful differential diagnosis and clinical pearls for the most common causes of hair loss in pediatric patients, I hope you all feel more comfortable tackling difficult hair loss cases!
References
-
- Grayson C, Heath C. An Approach to Examining Tightly Coiled Hair Among Patients With Hair Loss in Race-Discordant Patient-Physician Interactions. JAMA Dermatol. 2021;157(5):505-506. doi:10.1001/jamadermatol.2021.0338
- Grayson C, Heath C. Tips for addressing common conditions affecting pediatric and adolescent patients with skin of color. Pediatr Dermatol. Published online March 2, 2021. doi:10.1111/pde.14525
- Grayson C, Heath CR. Counseling About Traction Alopecia: A “Compliment, Discuss, and Suggest” Method. Cutis. 2021;108(1):20-22. doi:10.12788/cutis.0297
- Hubbard TW. The predictive value of symptoms in diagnosing childhood tinea capitis. Arch Pediatr Adolesc Med. 1999;153(11):1150-1153. doi:10.1001/archpedi.153.11.1150
- Kakourou T, Uksal U, European Society for Pediatric Dermatology. Guidelines for the management of tinea capitis in children. Pediatr Dermatol. 2010;27(3):226-228. doi:10.1111/j.1525-1470.2010.01137.x
- Gupta AK, Drummond-Main C. Meta-analysis of randomized, controlled trials comparing particular doses of griseofulvin and terbinafine for the treatment of tinea capitis. Pediatr Dermatol. 2013;30(1):1-6. doi:10.1111/j.1525-1470.2012.01866.x
- Chen X, Jiang X, Yang M, et al. Systemic antifungal therapy for tinea capitis in children. Cochrane Database Syst Rev. 2016;(5):CD004685. doi:10.1002/14651858.CD004685.pub3
- Callender VD, Wright DR, Davis EC, Sperling LC. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148(9):1047-1052. doi:10.1001/archdermatol.2011.3428
- Eginli AN, Dlova NC, McMichael A. Central Centrifugal Cicatricial Alopecia in Children: A Case Series and Review of the Literature. Pediatr Dermatol. 2017;34(2):133-137. doi:10.1111/pde.13046
Patient images courtesy of Dr. Adam Friedman.
This information was presented by Dr. Candrice Heath at the 2021 Skin of Color Update virtual conference held on September 10-12, 2021. The above highlights from her lecture were written and compiled by Dr. Emily Murphy.
Did you enjoy this article? Find more on Skin of Color Dermatology here.