Depending on your comfort level with treating scars, you may feel hesitation when taking on treatment for patients with keloids – especially those with skin of color. We all know keloids are more common in skin of color and we have most likely all treated these patients. But how can we improve patient outcomes and limit side effects?
During the 2020 Skin of Color Update, Drs. Maritza Perez and Jared Jagdeo shared their pearls for the treatment of these common but sometimes formidable maladies. In their lectures, Management of Keloids – Beyond the surgical approach (Dr. Perez) and Clinical Pearls and Future Applications (Dr. Jagdeo), they discussed techniques that can help your current treatment strategies, new techniques that you can integrate into your practice, and future directions.
This article will provide an overview of the talk, including:
-
- A brief discussion of keloid pathophysiology
- Conventional treatments including intralesional Kenalog, 1064nm microsecond-pulse multiple-pass treatment, and surgery with post-operative injection or radiation
- Priceless tips on how to make traditional treatments more effective
- Future treatments including – IL-4/IL-13 blockade, Botox, red light LED, and microRNA therapies
Before we get into the full review, here are my “practice barometers” – what I took away from the lecture that may change my practice or confirm my standards:
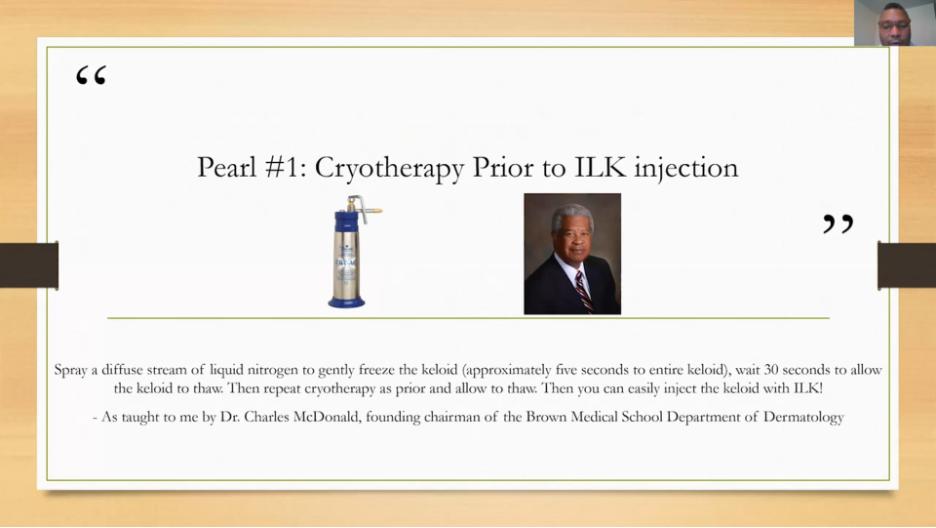
 Start using light cryotherapy prior to injecting keloids to make them more amenable to injection. Want the full details? Keep reading!
Start using light cryotherapy prior to injecting keloids to make them more amenable to injection. Want the full details? Keep reading!
 Try 1064nm microsecond-pulse low-fluence multiple pass treatment as described by Dr. Perez. Want to know the settings? See below!
Try 1064nm microsecond-pulse low-fluence multiple pass treatment as described by Dr. Perez. Want to know the settings? See below!
 Continue fractional ablative laser with laser-assisted drug delivery (LADD), excision with injectables, and excision with post-treatment radiation. Want to know more? Look below!
Continue fractional ablative laser with laser-assisted drug delivery (LADD), excision with injectables, and excision with post-treatment radiation. Want to know more? Look below!
 When treating keloids: set patient expectations and goals, wear PPE, and last but not least – look to the future for emerging treatments. Read on to learn what the future holds!
When treating keloids: set patient expectations and goals, wear PPE, and last but not least – look to the future for emerging treatments. Read on to learn what the future holds!
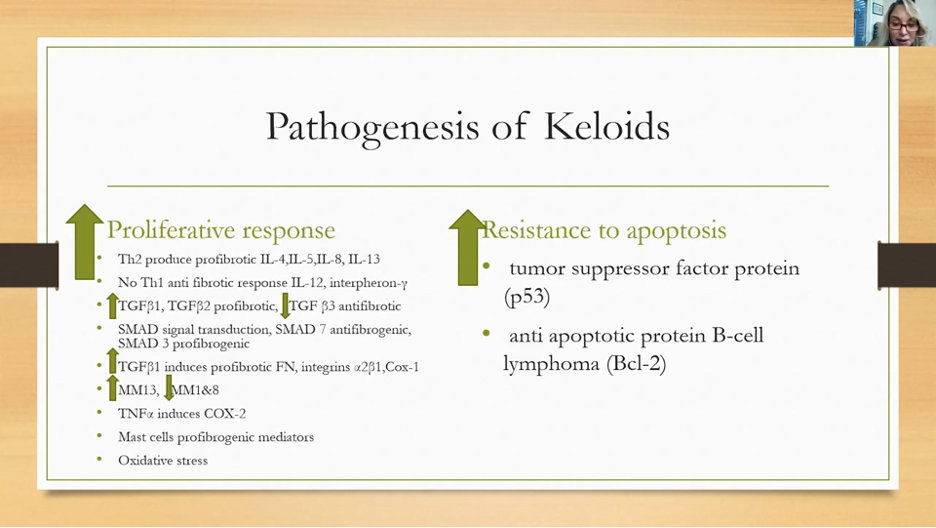
A Quick Review of the Basic Science
During the healing response following tissue injury, there is a concert of actions that occur in phases. Keloids are formed when the healing response is abnormal during the proliferative phase. The pathogenesis of keloids is complex, but it can be broken down simply into excessive proliferative, pro-fibrotic, and anti-apoptotic factors along with decreases in signals that are anti-fibrotic. This leads to increased proliferation and a lack of apoptotic factors that would help to “shutdown” the proliferation of the scar. This is why many see keloids as benign tumors and helps illustrate why recurrence can be a problem. See below for a great summation by Dr. Perez.
Non-surgical Management of Keloids
Below are techniques discussed by both presenters:
-
- Topical approaches: Pressure techniques, silicone sheeting, flavonoids, imiquimod, and topical steroids
- Intralesional: steroids, recombinant TGF-β3, bleomycin, IFNα2b, 5-FU, and dupilumab
- Consider cryotherapy prior to injection of ILK, 5-FU, etc. This allows the scar to be more edematous/softer and allows easier injection. The method is important here and was discussed in the question and answer session – this is a “painting” technique where you are gently freezing the scar while constantly moving for 5 seconds, then wait 30 seconds and freeze again. It was mentioned this is NOT like freezing an AK. If this is the first time you are trying this, start with less freeze time to avoid pigmentary alteration until you become familiar with the treatment and potential side effects.
- 1064nm laser – 5mm spot, 13-18J/cm2 fluence, 0.3ms pulse duration. Also, a “painting” technique with 2000 pulses over the scar. Caution to not dwell in one location and cause bulk heating while performing a procedure like this. Dr. Perez will start with 10mg/ml ILK at first visit then weekly treatments with the above laser treatment for 6 weeks. Some patients require more cycles of this protocol of weeks 1-7, ILK then 6 sessions of 1064nm.
- When injecting keloids consider using a larger needle. Dr. Jagdeo utilizes a 22-gauge needle and injects in a retrograde manner.
- Fractional ablative laser treatment with laser-assisted drug delivery (LADD). Dr. Jagdeo shared a patient example where a mature keloid over the occipital scalp was treated with CO2 fractional ablative treatment supplemented with triamcinolone ointment application with 8 total treatments and a great end result.
Surgical Management of Keloids
-
- When patients are looking for more immediate results or a keloid has been resistant to more conservative approaches – excision can be life-altering.
- This can be very successful for ear keloids and can be combined with adjuncts such as ILK and pressure. These excisions can be performed with secondary intent healing.
- When done for keloids off the ear, consider adjunctive radiation treatment. Dr. Perez discussed multiple types and treatment protocols but mentioned single-fraction electron beam radiation at 8 Gy 24-48 hours after surgery as an emerging option.
- It is helpful to work closely with your radiation oncologist in order to plan the appropriate timing for surgery in relationship to radiation treatment.

Future Directions in the Treatment of Keloids
-
- Clinical trials are on the horizon for IL-4 and/or IL-13 inhibitors in the treatment of keloids given their role in the pathogenesis of skin fibrosis.
- Botox has been shown to also improve keloids. The advantage to this is the low side effect profile; particularly in skin of color patients. The disadvantage being cost.
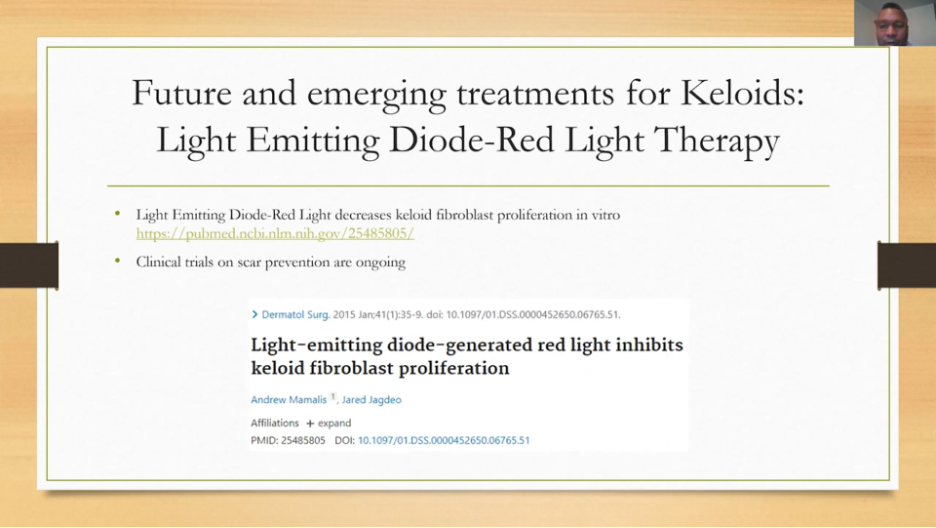
- Dr. Jagdeo has been involved in the development of light-emitting diode (LED) with red-light LED in the treatment of keloids. In vitro studies have shown decreased fibroblast proliferation without altering cell viability.
- Trials for scar prevention with red light LED are currently ongoing.
- MicroRNA is involved in the pro-fibrotic pathway in the formation of keloids and red-light LED has been shown to decrease these pro-fibrotic microRNA and increase the anti-fibrotic microRNA in fibroblasts.
More Tips When Treating Keloids
-
- Ensure you are protecting yourself during procedures on keloids. We have all experienced the difficulty in getting fluids into firm scars – wearing eye protection is a must for safe practice. Also, consider a mask or face shield to protect yourself and your staff.
- If your patient experiences hypopigmentation from treatment consider using Tacrolimus 0.1% ointment twice daily for 6 weeks – this was discussed during the Q&A session immediately following this presentation.
- Set patient expectations. Dr.Jagdeo discusses with patients that keloid treatment is a journey that requires multiple treatments in order to improve the cosmetic and symptomatic aspects of a scar. Treatment should occur every 4-6 weeks for a period of 1-2 years. The aesthetics of a keloid will improve but will still look and feel different from surrounding normal skin. Symptomatic control may never be complete, but major benefit should be expected. Finally, keloids may recur despite treatment, and therefore close follow-up is needed.
Final Thoughts
-
- Partner with your patients to help them on their journey for treatment of their keloids
- There are many treatments that can be employed for patients with keloids but multi-modal approaches typically provide the best results.
This information was presented by Drs. Maritza Perez and Jared Jagdeo during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Dr. James Contestable.
Did you enjoy this article? Find more on Skin of Color here.

