At the ODAC 2021 Sneak Peek Symposium on Inflammatory Skin Diseases, expert faculty presented on the topics of acne, rosacea, atopic dermatitis, hidradenitis suppurativa, and psoriasis. If you missed the live symposium, Next Steps will be sharing highlights and a summary of each lecture over the course of the next few weeks. Today, Dr. Blari Allais shares an excellent recap of Dr. Joslyn Kirby’s session on treating hidradenitis suppurativa in 2021 and beyond.
About Dr. Kirby:
 Dr. Joslyn Kirby is a dermatologist and researcher at Penn State Hershey. She earned her medical degree from the University of Virginia, then completed her Dermatology Residency at the University of Pennsylvania. In her clinical and research work, she is interested in acneiform conditions, especially hidradenitis, and value in healthcare
Dr. Joslyn Kirby is a dermatologist and researcher at Penn State Hershey. She earned her medical degree from the University of Virginia, then completed her Dermatology Residency at the University of Pennsylvania. In her clinical and research work, she is interested in acneiform conditions, especially hidradenitis, and value in healthcare
Dr. Kirby began her lecture by “setting the stage for Hidradenitis Suppurativa (HS)”:
-
- Stage 1: Isolated individual lesions, do not see scarring, tunnels, or fibrotic palpable dumbbell lesions.
- Stage 2: Starting to see more scarring and the presence of tunnels.
- Stage 3: Scarring, approaching complete coalescence of lesions.
Think about the worst area on a patient’s body as the area that drives the decision making!
“The immune system is doing all of the things in HS!”
Patients often come into the office having performed an internet search on Hidradenitis Suppurativa. It is important to educate our patients that this is an inflammatory disease and is not indicative of an infection. We know that HS is a pilosebaceous disease and that the main players are the hair follicle and the sebaceous glands. The complex immune web of HS also includes B cells, T cells, macrophages, keratinocytes, and bacteria which all contribute to the problem. Luckily this means there are many different targets we can take advantage of.
“HS is the rollercoaster from hell”
In caring for these patients it is important to consider what ways we can get acute flares under control and how can we manage this disease chronically.
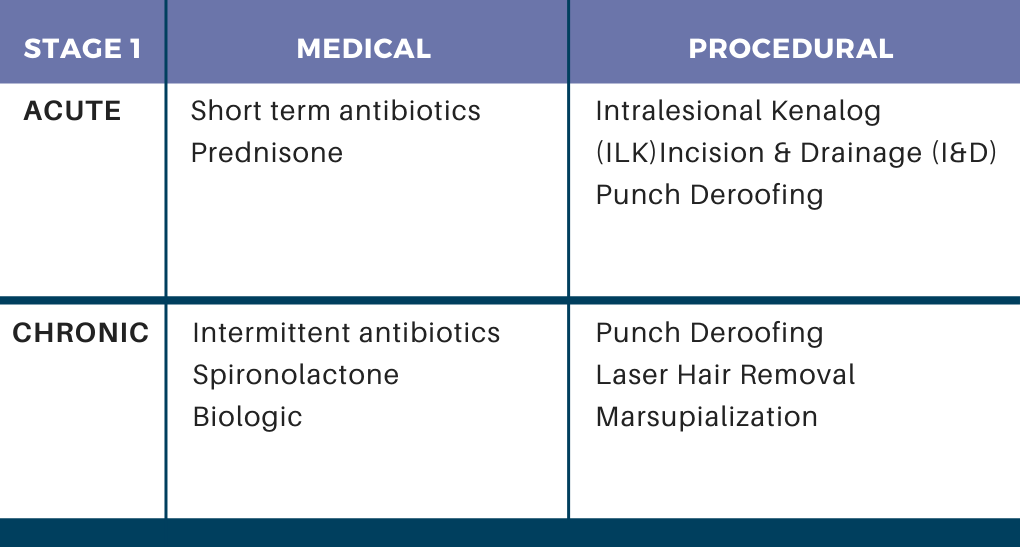
Stage 1 Treatment:
Medical therapy:
-
- Spironolactone can be a fantastic option for female patients.
- For antibiotics, Dr. Kirby likes to use pulses of 12 weeks of therapy and then stop to see how much improvement patients have afterwards.
Don’t forget about procedures!
-
- Laser hair removal can often be effective for people with mild disease.
- For intermittent flares, Incision & Drainage (I&D) or Intralesional Kenalog (ILK) can relieve pain and be helpful in the short term.
- ILK: 10mg /mL, about 0.75 cc into a single lesion
- After injection, studies show relief within 24-48 hours. This is very meaningful for patients.
- Important to counsel on common sequelae including slight indentation and post-inflammatory hyperpigmentation (PIH).
- Punch de-roofing can be of tremendous benefit:
- 4-6 mm punch biopsy over an inflamed nodule or abscess
- Scrape subsequent hole/pouch with a curette
- Apply aluminum chloride, gelfoam, bandaid
- Billing: code as simple Incision & Drainage.
Can also consider topical resorcinol in these patients:
-
- Dr. Kirby discussed one study that evaluated daily use of 15% resorcinol cream daily at the start of a flare.1
- Duration of the flares in these patients decreased from 9 days to 2.7 days.
- Pain on average decreased from 7.1 to 2.6 out of 10.
- Another study examined resorcinol 15% twice daily for 30 days.2
- 84% clinically resolved
- Pain decreased from 4.6 at day 0 to 0.5 at day 30
- Adverse effects included peeing and post-inflammatory pigment alteration
- Kirby orders 15% resorcinol cream from a compounding pharmacy and instructs her patients to apply it twice daily. 30-60g costs about $50-60.
Stage 2 Treatment:
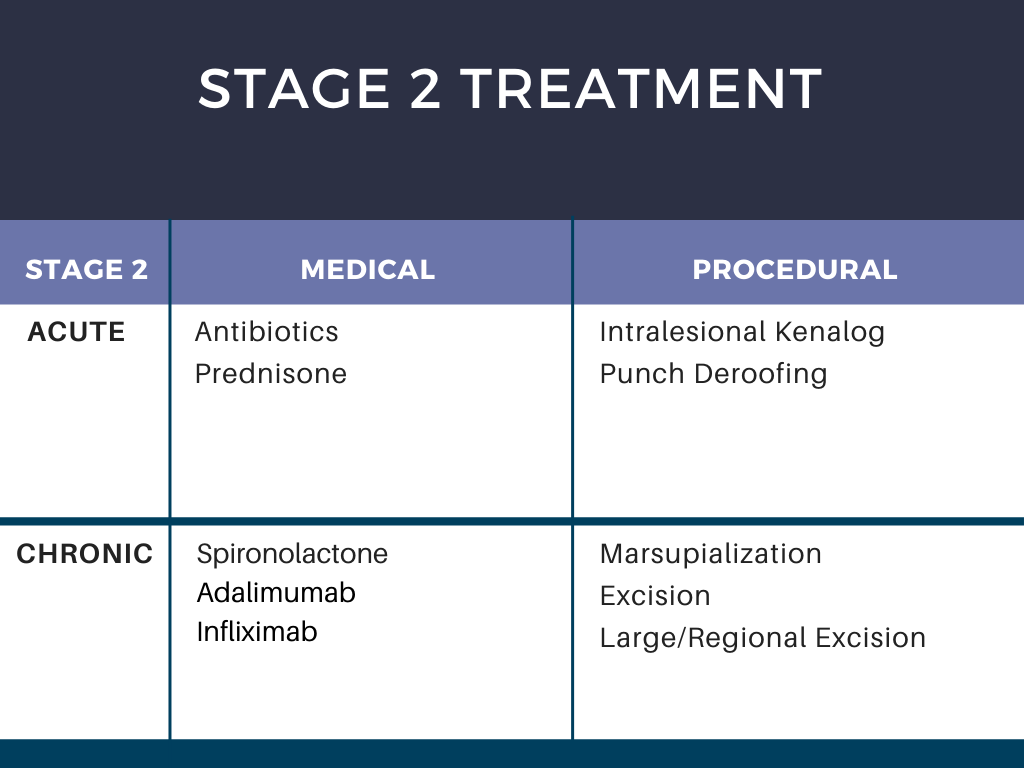
For stage 2, Dr. Kirby is walking into the room and having a conversation with the patient regarding biologics.
* Clinical trials are a great option for patients that have not been exposed to biologics before or have not been on them for 3-6 months.
Stage 3 Treatment:
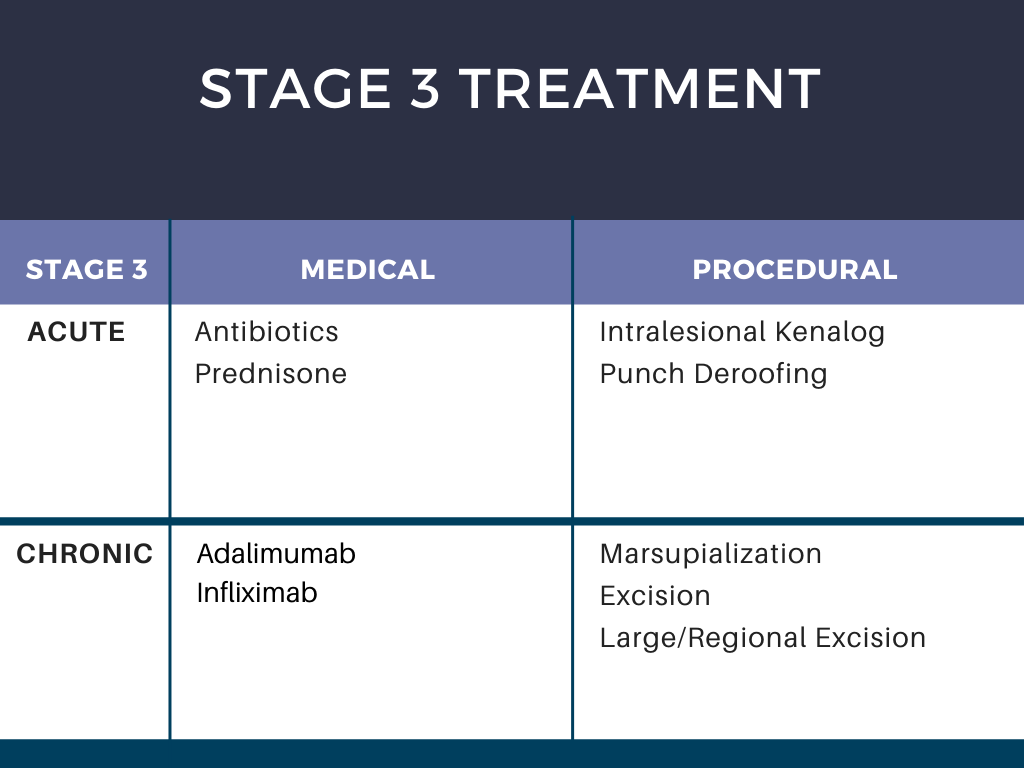
For stage 3, Dr. Kirby sets expectations upfront regarding surgery and that patients should anticipate having surgery either with you or with a plastic surgeon with experience in caring for HS patients.
* Consider clinical trials, as in stage 2 patients
Biologics
Dr. Kirby counsels patients that with biologic therapy, there is a greater chance that they will notice a meaningful reduction in disease. She also sets expectations: “it is a rare day that you will be completely controlled.”
-
- Adalimumab
- 49-59% of people achieve 50% + improvement.3
- Loading dose 160mg then 80mg 2 weeks later, maintenance 40mg weekly.
- Evaluate at 3-6 months
- If you see inflammatory lesions at follow-up –> mix up medicines.
- If you see tunneling –> add procedures.
- Infliximab
- 10mg/kg every 4-6 weeks is dosing that has had the most success.4
- Ask insurance company to cover every 4 weeks.
- Adalimumab
Consider switching a biologic
-
- Wait 4-6 months to assess “typical” response
- Start the new biologic:
- When “old” dose is due.
- As soon as you get it (if disease is bad enough, small enough overlap will not be a safety issue).
Working with insurance companies
-
- Prior Authorization letter: write aggressively
- Utilize the American Academy of Dermatology template letter for Humira (although FDA approved).
- Reiterate death from squamous cell carcinoma, depression/suicide.
- Underscore cost of hospitalizations for depression, IV antibiotics, surgery.
- Make sure to list your references supporting use of the medication.
- When on a peer to peer: be polite and speak earnestly.
- Prior Authorization letter: write aggressively
HS surgery
Marsupialization – Dr. Kirby stresses “you can do it !”
Open up a tunnel by making a small incision. Take a curette and look for the gelatinous material. With scissors, visualize and explore the area further. The goal is to appreciate a pale pink base. Unroof the area in its entirety: Dr. Kirby explains that she would like the area to take as long as it possibly needs to heal. The wound will granulate in and contract.
-
- Important to counsel patients that this will appear as a large defect initially, but eventually the scar will be much smaller as if the area had been sutured.
- Code as a complex Incision & Drainage.
For surgery, keep patients on biologics! Dr. Kirby highlights a soon to be published study that demonstrated no increased risk of postoperative complications while on biologic therapy in HS patients.
Comorbidities in HS
Dr. Kirby emphasizes the importance of thinking of our HS patients globally in terms of their possible comorbidities.
-
- 58% – Depression, anxiety. Perform the PHQ-2 questionnaire.
- 52% – Arthropathy. Ask about past medical history, morning stiffness, pain.
- 34% – Hypertension
- 20% – Diabetes. Ask about past medical and family history, polydipsia, polyuria, check fasting glucose, or Hgb A1c. Make sure patient has a primary care physician.
- 4% – PCOS
- 3% – Inflammatory bowel disease. Ask about diarrhea > 4 weeks, urgency, cramping, pain, blood (stools or rectum)
In summary, Dr. Kirby stresses to “manage HS like a boss”! It is important that we listen, educate, and motivate our patients. Set up a long-term plan with a combination of both acute and chronic treatments AND medicine and surgery. Procedures are key – do not be afraid! Finally, act as a manager and get a team together. Collaborative management with primary care, pain management, psychiatry/psychology, and plastic surgeons who specialize in HS is key.
References:
-
- Boer J, Jemec GME. Resorcinol peels as a possible self-treatment of painful nodules in hidradenitis suppurativa. Clin Exp Dermatol. 2010; 35:36-40.
- Pascual et al. Topical 15% resorcinol for hidradenitis suppurativa: An uncontrolled prospective trial with clinical and ultrasonographic follow-up. Journal of the American Academy of Dermatology. 2017; 77(6): 1175-1178.
- Kimball et al. Two Phase 3 Trials of Adalimumab for Hidradenitis Suppurativa. N Engl J Med. 2016; 375(5): 422-34.
- Oskardmay A et al. Determining the optimal dose of infliximab for treatment of hidradenitis suppurativa.
Images: Courtesy of Dr. Joslyn Kirby, MD
This information was presented by Dr. Joslyn Kirby at the 2021 ODAC Sneak Peek Symposium on Inflammatory Skin Diseases held on December 3rd, 2020. The above session highlights were written and compiled by Dr. Blair Allais.
Did you enjoy this article? Find more here.