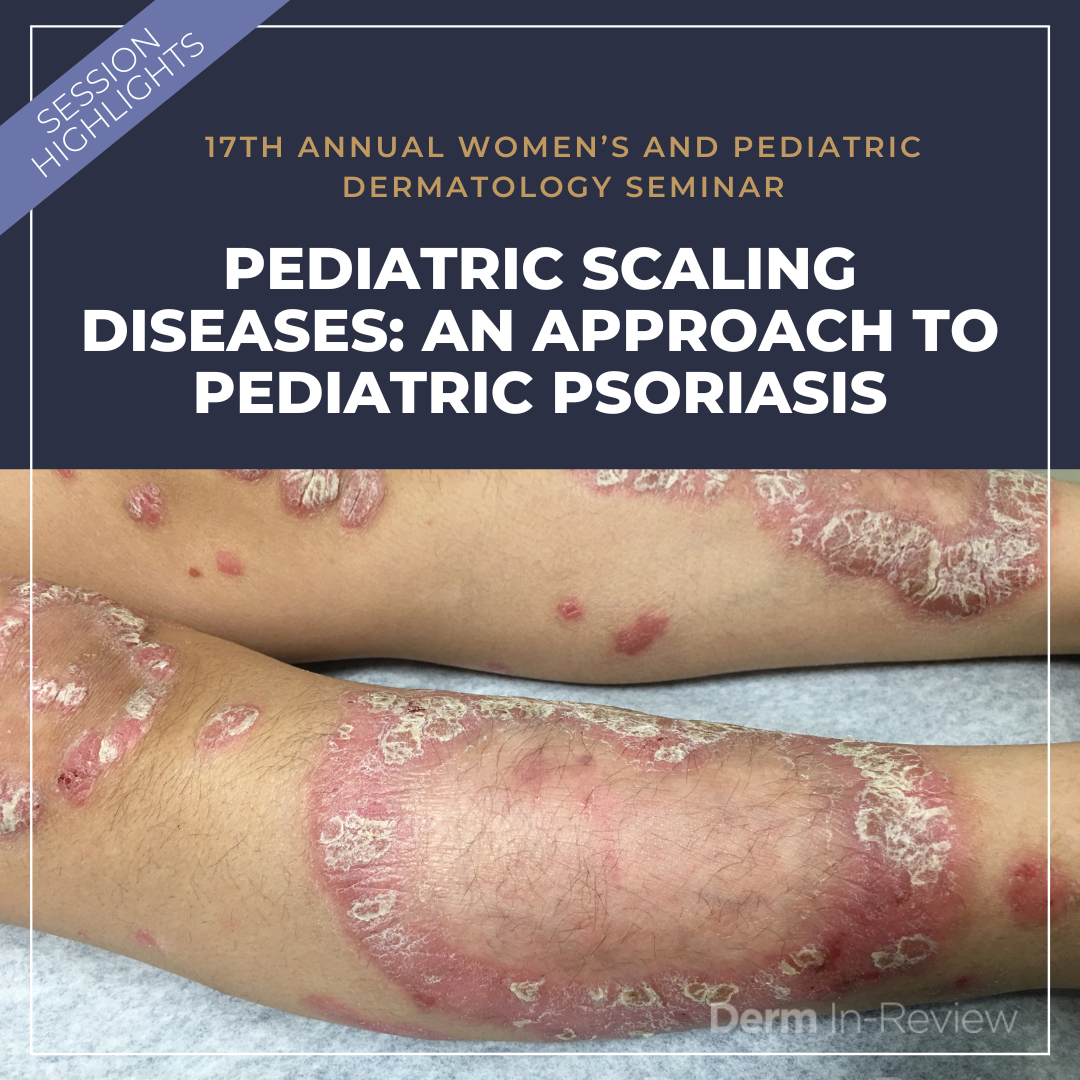
Dr. Lawrence F. Eichenfield, meeting co-chair for the 17th Annual Women’s and Pediatric Dermatology Seminar, kicked off session III with a superb talk titled “Scaling the Heights…and Below, Pediatric Scaling Diseases: Psoriasis and Others”, giving us a bird’s eye view on the old and the new regarding pediatric psoriasis.
Dr. Eichenfield is a complete rock star and served as a valued source for teaching us about pediatric psoriasis. He is the chief of pediatric and adolescent dermatology at Rady Children’s Hospital-San Diego and vice-chair of the Department of Dermatology at UC San Diego School of Medicine. He is board certified in dermatology, pediatric dermatology and pediatrics. Wow!
Let’s start with the basics
Psoriasis is a papulosquamous inflammatory skin disorder that affects 1% of children.
One third of all psoriasis starts in childhood
Of children with psoriasis, 1.2% will have psoriatic arthritis by age 18.
The reported average age of onset is varied (2 months -10 years).
1) Screening for and Diagnosing Pediatric Psoriasis
A. Children with psoriasis may present differently than adults.
Pediatric Psoriasis Presentation:
-
- If psoriasis is early onset (eg. infants) look for “diaper dermatitis”. We often see well-defined pink plaques in the diaper area. Scale may be present.
- 4-5% have facial involvement as the sole manifestation of psoriasis
- About 40% have facial plus body involvement
- 5% have BOTH psoriasis and atopic dermatitis, we call this an eczema/psoriasis overlap
- Scalp involvement is very common, especially in boys
- Look for nail pitting of the fingernails, also more commonly seen in boys. Pitting in the great toenail is common too.
B. Look at family history!
-
- If one parent is affected with psoriasis, the child has a 25% chance of having psoriasis.
- If BOTH parents are affected by psoriasis, the child has a 60-70% chance of having psoriasis.
C. Guttate psoriasis: Consider looking for streptococcal infection
Guttate psoriasis has a higher prevalence in children than adults (30% vs 2% of psoriasis patients).
This may be due to a concomitant group A beta-hemolytic streptococcal infection:
-
- Perform a throat culture if indicated (testing for strep throat)
- Perform a physical exam, including evaluation of the perianal skin (eg. for perianal strep)
Guttate psoriasis may resolve spontaneously, BUT up to 40% progress to plaque psoriasis, in which topical and/or systemic treatment may be indicated.
D. Think about the differential diagnosis for pediatric psoriasis
Below is a limited list of items on the differential diagnosis for pediatric psoriasis
-
- Seborrheic dermatitis: look for waxy scale, less well-defined plaques, may also involve the axillae and groin
- Pityriasis rubra pilaris: look for hyperkeratotic follicular papules, orange-red plaques, and palmoplantar hyperkeratosis. There are both resolving and chronic pediatric forms. Interestingly, there are a subset of patients with CARD14 mutations which can look like mixed PRP/Psoriasis on presentation.
- Tinea corporis/inflammatory tinea with pustules: watch out for guinea pigs carrying the very inflammatory T. Mentagrophytes. Other clues to help diagnose tinea are KOH prep, other involved family members, focal area of involvement, posterior cervical lymphadenopathy, and history of guinea pigs as pets!
- Other diaper dermatitis: irritant contact dermatitis, candida, langerhans cell histiocytosis, etc.
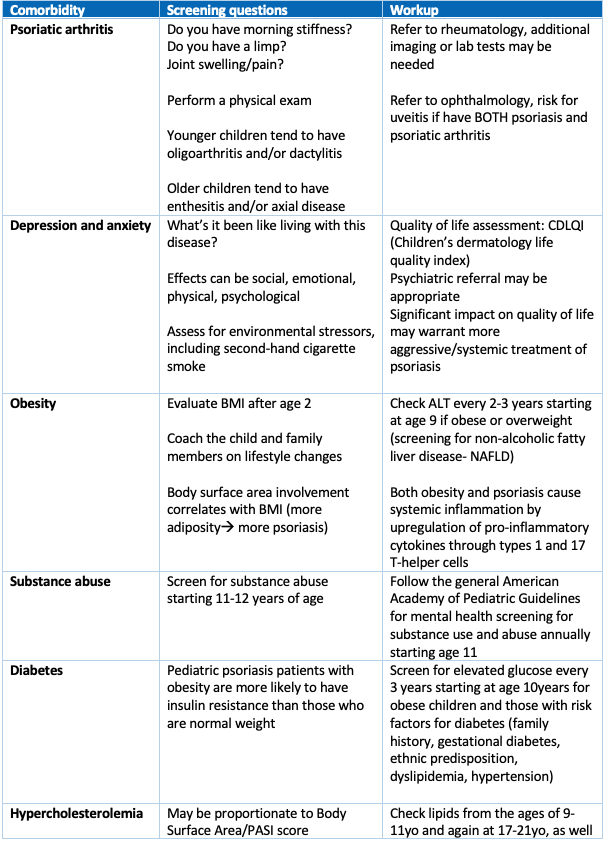
2) A focus on pediatric comorbidities in psoriasis
Pediatric patients are at risk of numerous comorbidities, especially metabolic syndrome, which can be diagnosed by the presence of at least 3 of the following 5 criteria:
-
- Obesity
- 2. Hypertension
- Dyslipidemia
- Insulin resistance
- Diabetes Mellitus
Excess adiposity promotes release of pro-inflammatory cytokines through the TH1 and TH17 T-cell helper pathways. Thus, excess adiposity may be a predisposing factor to psoriasis and exacerbate psoriasis. Psoriatic arthritis is another comorbidity, present in 0.7% of children with psoriasis, which increases to 1.2% by age 18. Arthritis may precede skin disease in up to 80% of cases. See the table below to learn more about screening for comorbidities in pediatric psoriasis.
3) Treating pediatric psoriasis: more than just a stepwise approach
A. Severity of psoriasis is MORE than just a number: it’s time to take an individualized approach
Here’s the latest news: a “stepwise” ladder approach to therapy is OUT and an individualized approach is IN.
-
- Severity of psoriasis is MORE than just a number.
- Classically, severity of psoriasis is dictated by body surface area (BSA)
- <3% mild
- 4-10% moderate
- >10% severe
However, severity of psoriasis absolutely depends on the disease burden, including the impact on quality of life, psychosocial impact, location on the body (eg. may be considered more severe on the face and scalp), and presence of comorbidities.
You do not have to start at the bottom of the “therapeutic ladder.” Topical therapies may not be sufficient for more severe disease, widespread distribution, or cosmetically sensitive areas. Likewise, you do not have to undergo a trial of phototherapy prior to considering systemic agents or biologics.
B. Considerations for treatment:
1) Therapy for pediatric psoriasis used to be considered a “stepwise” approach, but things have changed
Topicals⇒phototherapy⇒systemics⇒biologics
Now, things have changed. We have to take into account the disease burden, including body surface area, social factors regarding feasibility of getting/maintaining treatment, location of psoriasis on the body, psychological impact, and others.
2) Topical therapy for pediatric psoriasis: the old and the new
Topicals are recommended for the treatment of pediatric psoriasis, but they are off-label use.
Dr. Eichenfield tends to think of patients divided by age: Less than 12-years-old and greater than 12-years-old.
Children greater than 12 years old:
-
- ultra-high potency topical corticosteroids are recommended as monotherapy for short term treatment of localized psoriasis
- consider combination of betamethasone + calcipotriene; if using ointment, apply once daily up to 4 weeks; if suspension, it is okay to use for 8 weeks at a time on the scalp of adolescents
Children less than 12 years old:
-
- consider lower potency topical corticosteroids and steroid-sparing alternative agents
For the diaper/groin, axillae, and face:
-
- consider tacrolimus 0.1% ointment for monotherapy
For all patients: consider rotation with steroid sparing alternatives (vitamin D analogues, coal tar derivatives, emollients, topical calcineurin inhibitors). Of note emollient can reduce the irritation of calcipotriene. Other alternative topicals as monotherapy or combination therapy include topical tazarotene (careful—pregnancy category X for those who can become pregnant), and anthralin, which is best when used for greater than 12 weeks and with short contact therapy (<2hrs) prior to rinsing off in order to minimize irritation.
Newer topical treatments under investigation include roflumilast (a topical phosphodiesterase-4 (PDE-4) inhibitor), and tapinarof (a topical aryl hydrocarbon receptor antagonist which is approved for 12 years and older in atopic dermatitis).
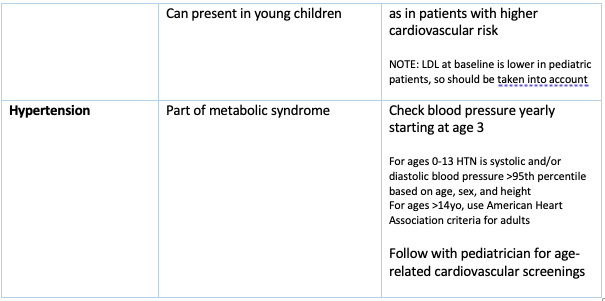
3) Pediatric psoriasis: choosing a systemic agent
Ultimately we choose systemic therapy based on shared decision making, disease burden, and ability to access the medication.
i. Non-biologic agents include:
-
- Methotrexate:
- dihydrofolate reductase inhibitor, inhibits DNA synthesis, repair, and cellular replication
- Slow onset, good for arthritis
- Is trusted and has long term safety and efficacy data
- Cyclosporine:
- calcineurin inhibitor, immunosuppressive
- used (short term) for rapid rescue of erythrodermic/pustular/unstable psoriasis
- Acitretin:
- Non-immunosuppressive vitamin A-based compound
- Pregnancy category X
- Good for pustular, guttate, and palmoplantar psoriasis
- Methotrexate:
ii. Phototherapy:
-
- We do not have to try phototherapy prior to starting a systemic or biologic agent
- Good if feasible for the patient: guttate, small/thin plaques, possibly pustular
iii. Biologics:
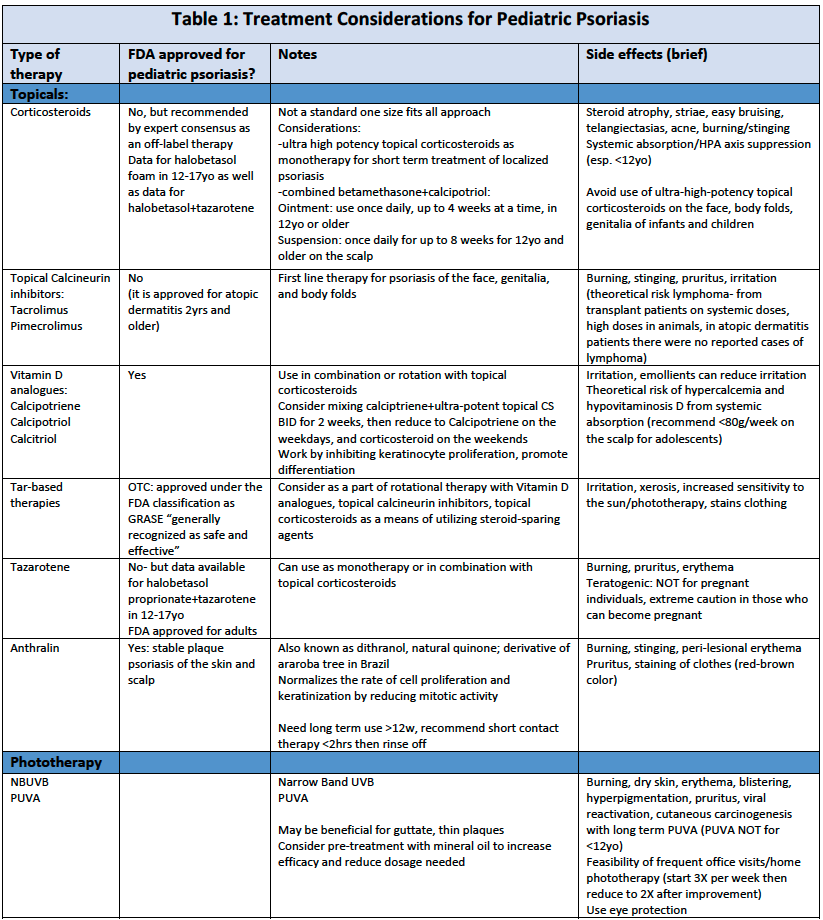
Biologics approved for pediatric plaque psoriasis (PsO) and pediatric psoriatic arthritis (PsA) are:
-
- Etanercept (TNF-α inhibition): approved for PsO 4 years and older, 0.8mg/kg/weekly (max 50mg weekly)
- Uteskinumab (IL12/23 p40 unit inhibition): approved for PsO 6 years and older
- Week 0,4, then every 12 weeks: 0.75mg/kg (<60kg), 45mg (60-100kg), 90mg (>100kg)
- Lowest # of injections for pediatric patients (2starter doses, then 4X a year)
- Of note: higher rates of PASI 90 in IL-17 and 23 inhibitors compared to ustekinumab (~70-78% vs 64%)
- Secukinumab (IL- 17A inhibition): approved for PsO 2 years and older, PsA 6 years and older
- Plaque and PsA psoriasis: dosing weeks 0,1,2,3,4 then every 4 weeks
- 15-50kg, 75mg dose
- >50kg, 150mg dose
- Ixekizumab (IL-17A inhibition): approved for PsO 6 years and older
- weight based dosing
- <25kg: 40mg at week 0, 20mg every 4 weeks
- 25-50kg: 80mg week 0, 40mg every 4 weeks
- >50kg: 160mg week 0, then 80mg every 4 weeks
Of the approved biologics for pediatric psoriasis, ustekinumab has the fewest number of injections (2 starter doses, then 4 times per year). It is important to remember, however, that there is a trade-off in efficacy. The IL-17 inhibitors have a higher number of patients achieving PASI90 by week 12 (~70-78%) than those on ustekinumab (~64%).
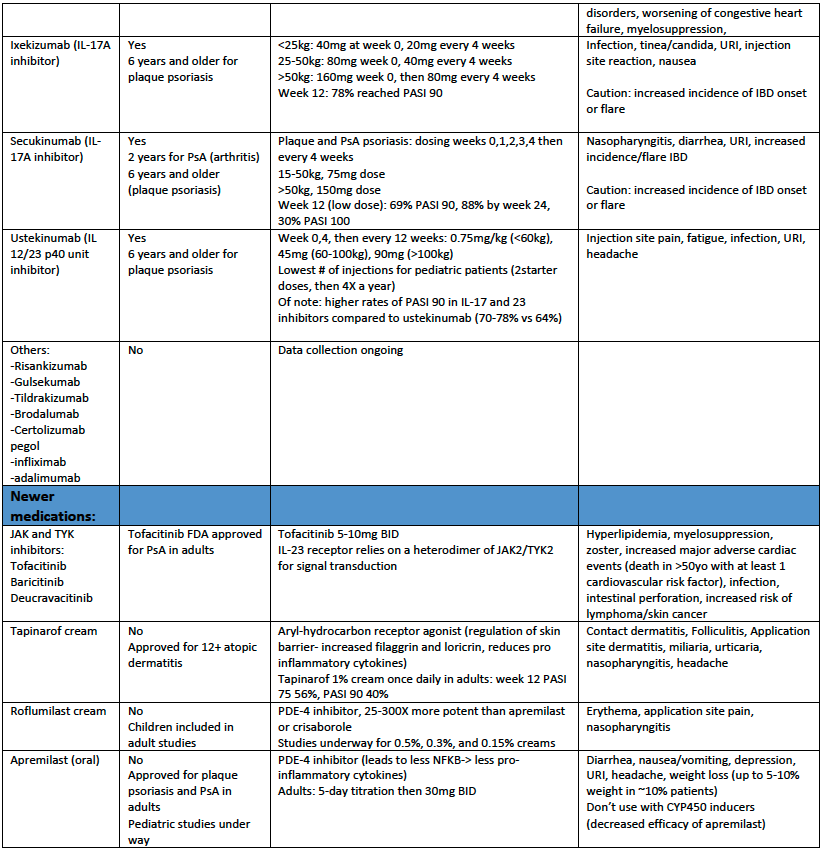
See table 1 for additional information about treatment options for pediatric patients with psoriasis.
Summary
-
- Pediatric psoriasis can present in multiple ways. We should pay particular attention to the diaper area in infants, scalp and facial involvement, nail pitting and joint pain
- Psoriasis can have profound physical, social, emotional, and functional impact on children. This cannot be understated and should play a role in deciding the most appropriate treatment options.
- There are no FDA approved topical medications for pediatric psoriasis, however, topical corticosteroids are recommended for older children for short term treatment of localized plaque psoriasis. We can choose to combine or alternate these with steroid sparing alternatives
- 4 biologics are FDA approved for pediatric psoriasis, with ustekinumab being the least number of injections per year (4)
- Screening for comorbidities in the pediatric psoriasis population is a MUST, taking care to diagnose metabolic syndrome, psychiatric conditions, and psoriatic arthritis, all of which are more common in children with psoriasis compared to those without it
- Other items to consider on the differential diagnosis of psoriasis are PRP, tinea, seborrheic dermatitis, and other diaper dermatitis
Supplemental table 1
Click here to enlarge
References
-
- Menter A, Cordoro KM, Davis DMR, Kroshinsky D, Paller AS, Armstrong AW, Connor C, Elewski BE, Gelfand JM, Gordon KB, Gottlieb AB, Kaplan DH, Kavanaugh A, Kiselica M, Kivelevitch D, Korman NJ, Lebwohl M, Leonardi CL, Lichten J, Lim HW, Mehta NN, Parra SL, Pathy AL, Farley Prater EA, Rupani RN, Siegel M, Stoff B, Strober BE, Wong EB, Wu JJ, Hariharan V, Elmets CA. Joint American Academy of Dermatology-National Psoriasis Foundation guidelines of care for the management and treatment of psoriasis in pediatric patients. J Am Acad Dermatol. 2020 Jan;82(1):161-201. doi: 10.1016/j.jaad.2019.08.049. Epub 2019 Nov 5. Erratum in: J Am Acad Dermatol. 2020 Mar;82(3):574. PMID: 31703821.
-
- Craiglow BG, Boyden LM, Hu R, Virtanen M, Su J, Rodriguez G, McCarthy C, Luna P, Larralde M, Humphrey S, Holland KE, Hogeling M, Hidalgo-Matlock B, Ferrari B, Fernandez-Faith E, Drolet B, Cordoro KM, Bowcock AM, Antaya RJ, Ashack K, Ashack RJ, Lifton RP, Milstone LM, Paller AS, Choate KA. CARD14-associated papulosquamous eruption: A spectrum including features of psoriasis and pityriasis rubra pilaris. J Am Acad Dermatol. 2018 Sep;79(3):487-494. doi: 10.1016/j.jaad.2018.02.034. Epub 2018 Mar 1. PMID: 29477734; PMCID: PMC6098739.
-
- Nogueira M, Paller AS, Torres T. Targeted Therapy for Pediatric Psoriasis. Paediatr Drugs. 2021 May;23(3):203-212. doi: 10.1007/s40272-021-00443-5. Epub 2021 Apr 3. PMID: 33811318.
-
- Bissonnette R, Stein Gold L, Rubenstein DS, Tallman AM, Armstrong A. Tapinarof in the treatment of psoriasis: A review of the unique mechanism of action of a novel therapeutic aryl hydrocarbon receptor-modulating agent. J Am Acad Dermatol. 2021 Apr;84(4):1059-1067. doi: 10.1016/j.jaad.2020.10.085. Epub 2020 Nov 3. PMID: 33157177.
-
- Milakovic M, Gooderham MJ. Phosphodiesterase-4 Inhibition in Psoriasis. Psoriasis (Auckl). 2021 Mar 17;11:21-29. doi: 10.2147/PTT.S303634. PMID: 33763335; PMCID: PMC7982714.
This information was presented by Dr. Lawrence F. Eichenfield at the 17th Annual Women’s and Pediatric Dermatology Seminar held June 3-4, 2022. The above highlights from his lecture were written and compiled by Dr. Jacqueline McKesey.
Did you enjoy this article? You can find more on Medical Dermatology here.