Can you improve your culturally-competent hair loss consultation? Would you like to grow your toolbox for comprehensive alopecia treatment? If so, you are in the right place!
Hair loss is a frequent concern for patients visiting the dermatologist, especially in patients with pigmented skin types. Kinky or coiled hair has an innate fragility that makes African Americans especially prone to hair loss concerns. At the 2020 Skin of Color Virtual Update, Dr. Susan Taylor discussed Conventional Treatment Approaches for Hair & Scalp Disorders in Skin of Color Patients. Dr. Taylor advised how to have a culturally competent hair loss consultation, reviewed common patterns of hair loss, and highlighted comprehensive treatment of multifactorial causes of alopecia.
Before we get into therapeutic strategies for alopecia, let’s highlight important considerations to institute an effective treatment plan:
-
- Understand common ethnic hairstyles and practices
- Recognize the impact of hair and scalp disorders
- Clearly identify the problem and obtain a thorough history, including details regarding hair care practices, products used, and symptoms
- Complete physical examination and consider scalp biopsy
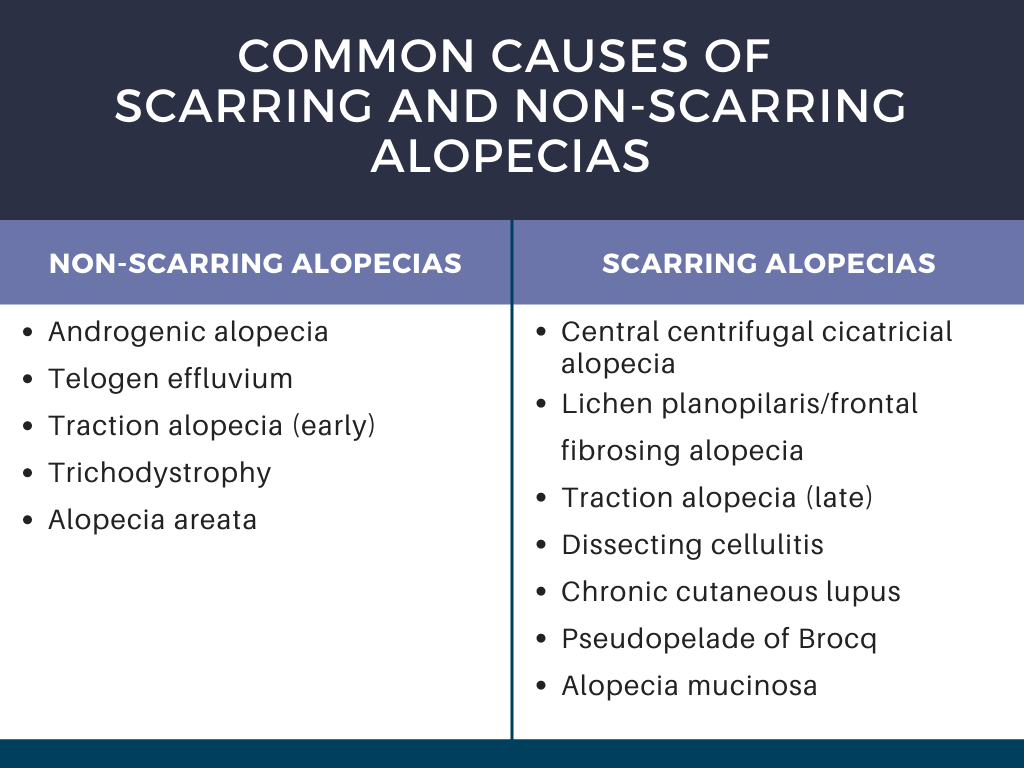
- Accurately diagnose the disease (see Table 1 for common causes of alopecia)
- Effectively and competently partner with the patient to treat the disorder with appropriate therapy
Dr. Taylor stressed the importance of culturally competent questioning during the visit. For example, asking an African American woman if she shampoos daily can reduce the patient’s confidence in the physician’s understanding of her hair type, especially during a race discordant visit. To build confidence, it is critical to understand routine hair practices and to be familiar with common products.
During the hair loss consultation, it is important to understand the problem experienced by the patient. Frequent symptoms noted by the patient that can clue in the underlying alopecia include:
-
- Hair length is not increasing.
- There is hair breakage.
- Hair is falling out at the root.
- There is decreased hair density.
- There is focal or localized hair loss.
Other considerations include the duration of hair loss, any associated symptoms, and presence of family history of hair loss. Further, it is important to ask about their hair care history. The types of hairstyles used by the patient and the hair care routine should be discussed.
The physical exam should be thorough to evaluate the scalp and hair density, a hair pull test, and examination of the eyebrows and eyelashes. The presence of weaves, braids, or wig caps may impede evaluation. If the patient has any of these hairpieces on the scalp that cannot be easily removed during the visit, the patient should return for evaluation after these are removed. History can still be discussed during the visit, however, the co-pay should be refunded, and the patient should be offered an earlier appointment for evaluation of the hair and scalp.
Now that we have discussed how to approach the consultation, let’s get into the alopecias! Dr. Taylor highlighted central centrifugal cicatricial alopecia, traction alopecia, and frontal fibrosing alopecia, as well as tips to minimize breakage, reduce hair tension, and scalp care to treat seborrheic dermatitis.
Central centrifugal cicatricial alopecia (CCCA) is a scarring alopecia seen in about 5.6% of African American women. It frequently starts with increased hair breakage at the vertex, and patients often have associated symptoms of itching, burning, tenderness, and soreness of the scalp. The goals of treatment are to aggressively treat the CCCA in the early stages to prevent progression, relieve symptoms, and possibly have some regrowth in the affected areas. There are no randomized controlled trials for CCCA treatment, thus evidence for treatment comes from case reports and series. The mainstay of treatment is corticosteroids (topical and intralesional), anti-inflammatory antibiotics, antimalarials, and minoxidil (topical and oral formulations). Anti-seborrheic shampoos, hair transplantation, and platelet-rich plasma injections serve as adjuncts to treatment. See Table 2 for detailed treatment options. Frequently multiple agents are used in combination to control the disease.
Two important areas of focus when treating CCCA that Dr. Taylor highlighted are practices to minimize hair breakage and treatment of frequently concurrent seborrheic dermatitis.
Tips to minimize hair breakage:
-
- Use a wide-tooth comb to detangle wet hair
- Start detangling by the distal end while holding the proximal end of the hair
- Avoid brushing to detangle
- Utilize protective hairstyles
Concurrent seborrheic dermatitis can contribute to scalp inflammation that may exacerbate hair loss. Anti-fungal shampoos, such as ketoconazole or ciclopirox, are often drying. This excessive drying can worsen the hair breakage that occurs in ethnic hair. To minimize this, Dr. Taylor recommends 5-10 minute scalp contact time with the medicated shampoo and avoidance of contact with the strands of the hair. Further, Dr. Taylor recommends to follow the anti-seborrheic shampoo with a conditioning shampoo and a conditioner to limit hair breakage. She advises shampooing weekly or every other week. For corticosteroids, Dr. Taylor recommends avoidance of solution formulations in favor of creams, ointments, and oils.
As opposed to hair breakage or thinning at the vertex, another frequent hair loss concern is hair loss at the frontal hairline. Two common causes of frontal hair loss are traction alopecia and frontal fibrosing alopecia. While they both can present with loss of the frontal hairline, they have distinct features to assist with an accurate diagnosis.
Traction alopecia (TA) is a form of hair loss at the anterior hairline, typically in younger patients. TA is caused by prolonged and repetitive tension on the follicles, due to tight hairstyles such as braids, ponytails, buns, and weaves. Early in the disease, perifollicular papule and pustules can be seen. The temporal area is most commonly affected. Early TA is nonscarring, although it can progress to scarring alopecia with repeated traction. The “fringe sign” can be a clinical clue, where a small portion of the anterior hairline is retained.
Frontal fibrosing alopecia (FFA), a form of lichen planopilaris, is a scarring alopecia that affects the frontal hairline as well as eyebrows and eyelashes. The average age of onset is 53-72, and the most commonly affected groups is post-menopausal African American women. The “lonely hair sign” is a frequent clinical feature, where 1-2 terminal follicles remain on the frontal scalp in an area otherwise diffused loss of hairs and follicles.
While there are several different causes of frontal hair loss with different treatment approaches, there are some universal hair care approaches that are recommended:
-
- apply braids loosely to avoid traction
- remove braids/extensions immediately or loosen them if there is pain or irritation
- leave braided styles in the hair no longer than 2 months
- shampoo the scalp regularly (ie weekly)
- loosely sewn-in weaves are preferred to bonding glues
- shoulder length is preferred to long braids and weaves to reduce tension on the hair
- alternate hairstyles when possible and take breaks between wearing breaded and sewn in styles
For traction alopecia, treatment is most effective early in the disease course before the hair follicles are permanently scarred. Dr. Taylor recommends avoidance of high tension hairstyles in addition to treatment strategies to reduce associated inflammation. For patients with associated inflammatory papules and pustules, doxycycline can be helpful.
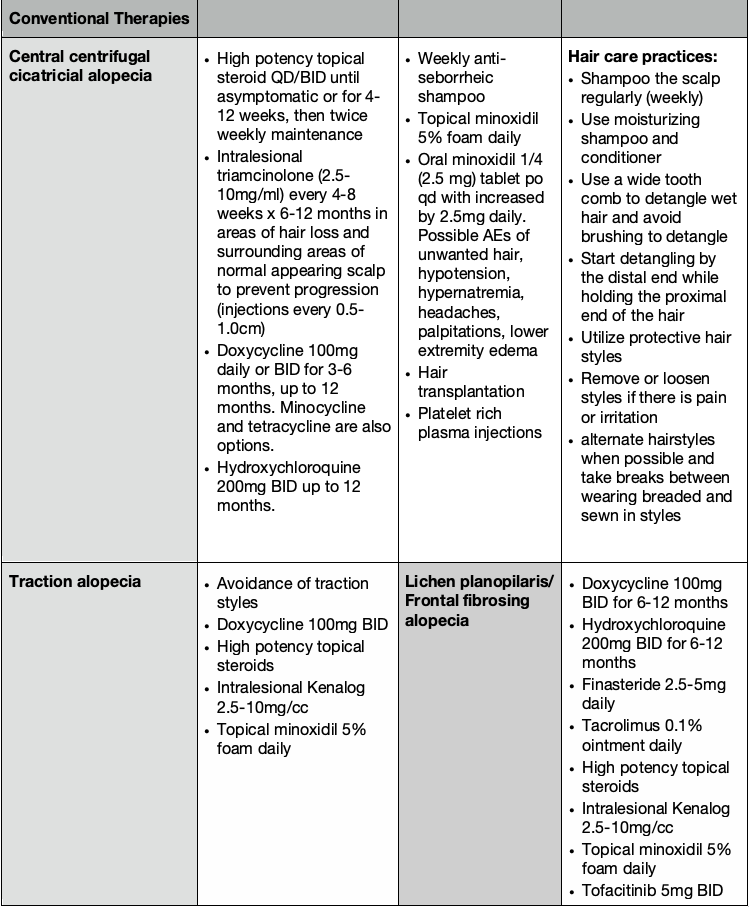
In lichen planopilaris (LPP) and frontal fibrosing alopecia (FFA), Dr. Taylor stresses that the primary goal of treatment is to halt progression of the hair loss, although regrowth can be achieved with optimal response to treatment. A combination of topical and oral agents can be helpful over a long course of treatment, as outlined in Table 2. Dr. Taylor discussed a recent study showing efficacy with oral tofacitinib, used as monotherapy or as adjunctive therapy having efficacy in 80% of patients. The main adverse event observed in the ten patients in this study was weight gain.
In closing, Dr. Taylor highlights that hair loss is frequently multifactorial, and more than pathology can be simultaneously present. In more than 10% of cases, CCCA can be seen with androgenic alopecia. Further, traction alopecia can often be complicated by androgenic alopecia, tinea capitis, or seborrheic dermatitis. This further supports a thorough physical exam with possible biopsy for accurate diagnosis and a comprehensive treatment plan in a culturally competent manner.
This information was presented by Dr. Susan Taylor during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Dr. Edita Newton.
Main image credit: Image courtesy of the Journal of Drugs in Dermatology.
Did you enjoy this article? You can find more here.