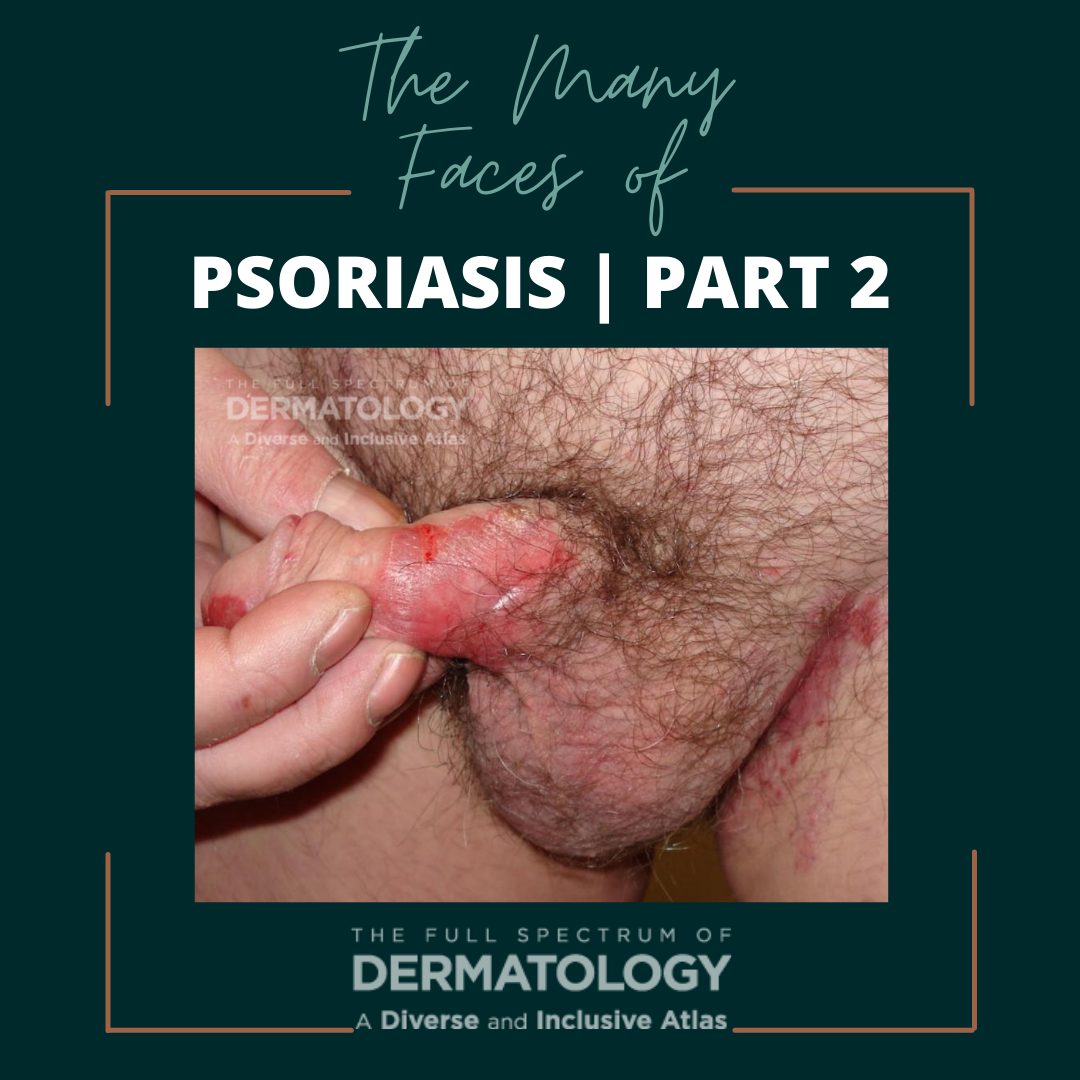
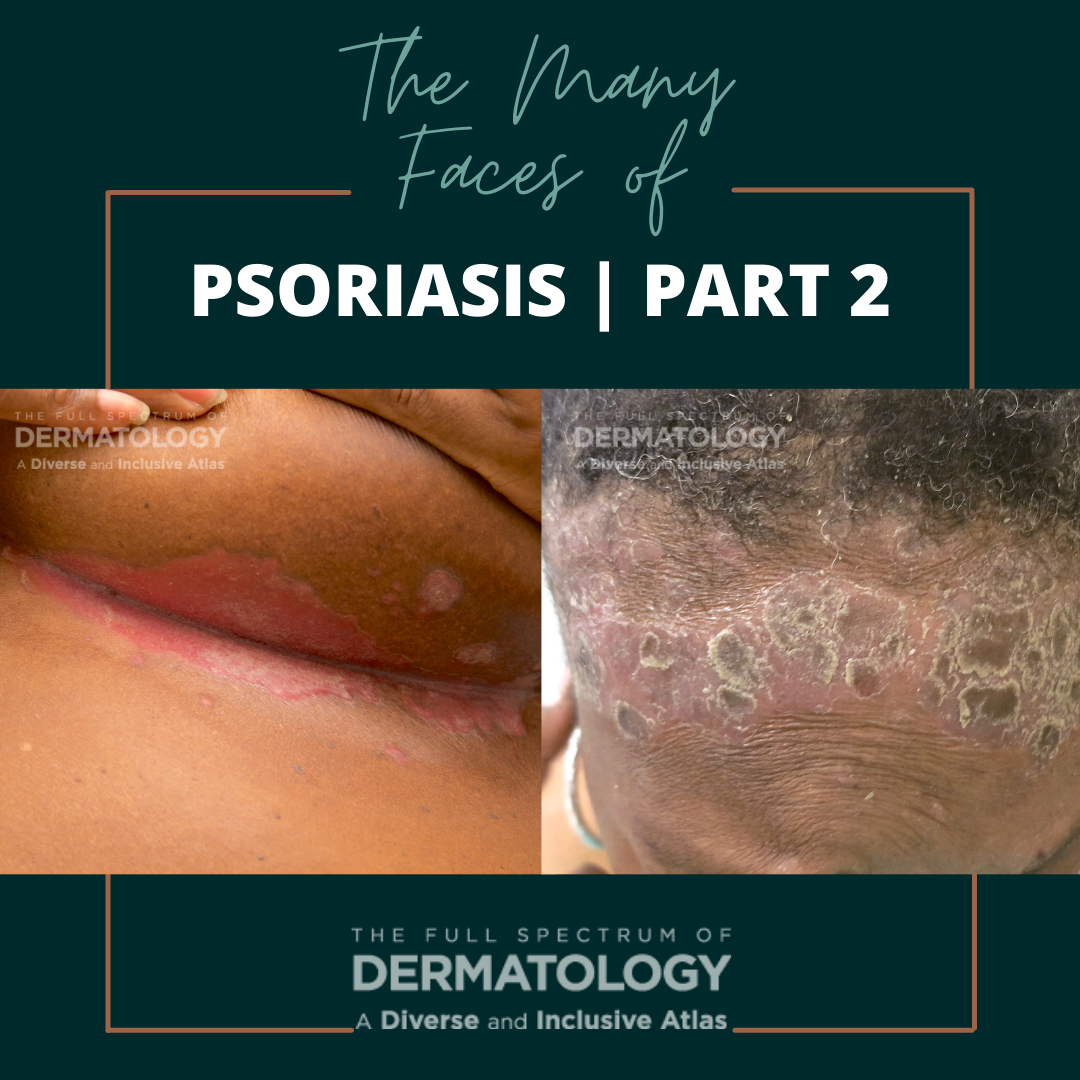
Did you know that psoriasis doesn’t just present on the arms, legs, and trunk? It can also appear in non-conventional locations (aka “special site” psoriasis) including the scalp, face, and body folds (such as the axillary, inframammary, and inguinal fields, and intergluteal clefts). In the skin folds, psoriasis is also referred to as “inverse psoriasis.” In darker skin types, the areas can have a more violaceous hue instead of bright red in appearance.
 Inverse or special site psoriasis has been reported in up to 36% of the population, but the actual prevalence varies widely as there is no specific criteria for diagnosing isolated inverse psoriasis vs special site psoriasis as a component of generalized psoriasis.
Inverse or special site psoriasis has been reported in up to 36% of the population, but the actual prevalence varies widely as there is no specific criteria for diagnosing isolated inverse psoriasis vs special site psoriasis as a component of generalized psoriasis.
Though some believe that inverse or special site psoriasis isn’t as burdensome to patients as the classic plaques on the extremities and trunk because they aren’t visible to the general population; however, this is far from the case. Patients with inverse psoriasis often report of a significant impact on their quality of life, especially as it pertains to sexual life as well as completing day to day activities, given the chronic friction that occurs in those areas with tighter clothing including undergarments.
 Differential diagnosis for inverse psoriasis includes other dermatologic conditions that often affect intertriginous areas, such as irritant or allergic contact dermatitis, erythrasma, acanthosis nigricans, granular parakeratosis, benign familial pemphigus, keratosis follicularis, and pemphigus vegetans. It is important to check other sites of the body (including the scalp, trunk, and extremities) for any additional signs of psoriasis, which would make the diagnosis easier. Though inverse psoriasis is often diagnosed clinically, sometimes, a biopsy might be indicated. In those cases, it will still show the classic histopathologic findings including elongated rete ridges, epidermal hyperplasia, parakeratosis, reduced granular layer, and collections of neutrophils in the stratum corneum and epidermis.
Differential diagnosis for inverse psoriasis includes other dermatologic conditions that often affect intertriginous areas, such as irritant or allergic contact dermatitis, erythrasma, acanthosis nigricans, granular parakeratosis, benign familial pemphigus, keratosis follicularis, and pemphigus vegetans. It is important to check other sites of the body (including the scalp, trunk, and extremities) for any additional signs of psoriasis, which would make the diagnosis easier. Though inverse psoriasis is often diagnosed clinically, sometimes, a biopsy might be indicated. In those cases, it will still show the classic histopathologic findings including elongated rete ridges, epidermal hyperplasia, parakeratosis, reduced granular layer, and collections of neutrophils in the stratum corneum and epidermis.
Treatment of inverse psoriasis typically includes a low/mid potency topical steroid such as desonide or hydrocortisone, calcineurin inhibitors including tacrolimus or pimecrolimus, and/or vitamin D analogs like calcipotriene. Additionally, it is important to keep the areas clean from bacteria, fungus, and yeast, using topical antimicrobials/antiseptic agents due to a higher risk of infection in intertriginous areas. For more extensive or recalcitrant areas, systemic immunosuppressant medications including methotrexate, cyclosporine, or biologics such as adalimumab, ixekinumab, or secukinumab may be warranted. Lastly, excimer laser can also be utilized to target areas of inverse psoriasis with success.
Nuances to Highlight
It’s important to remember that while inverse psoriasis has identical histopathologic findings to classic psoriatic plaques, lesions in intertriginous areas may not present with the classically associated silvery scale. Usually, however, the areas are still well demarcated in an annular pattern which can aid in identifying the diagnosis. Lesions may also appear erosive. Also, because these areas are generally more sensitive and oftentimes, certain psoriasis medications such as salicylic acid and retinoids are only utilized as last resort treatment options due to the irritating nature of these medications. Also, patients with inverse or special site psoriasis are still at risk of psoriatic arthritis, so it is important to ask patients about any joint stiffness or discomfort at each and every visit.
This article is part of Next Steps in Derm series “The Many Faces of” which showcases side-by-side images of some of the most commonly seen dermatology conditions in an array of skin tones and briefly highlight nuances in clinical presentation. All images featured in the series are part of The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, a resource developed by co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD, and published by SanovaWorks and Educational Testing & Assessment Systems.
Acknowledgements
We thank co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD for reviewing the content of this article.
Reference
Eleryan, Misty, and Adam Friedman. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. SanovaWorks, 2021.
NOW AVAILABLE! Visit the online image gallery for The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, where you will find high-quality images that you will be able to use, free of charge, for non-commercial educational purposes. Access the online gallery here.
The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas DIGITAL EDITION is available for purchase here.
If you missed previous articles from this series, you can find them here.
