Atopic dermatitis is a common, chronic, life-altering disease. With its visibility and debilitating pruritus, atopic dermatitis significantly impacts our patients’ quality of life. For those with resistant and extensive disease, we are happy to have numerous new systemic agents at our disposal, one being tralokinumab, an IL-13 antagonist. We continue our series, Therapeutic Cheat Sheet, with a closer look at tralokinumab, which is newly FDA-approved for the treatment of moderate-to-severe atopic dermatitis that has failed topical therapies.
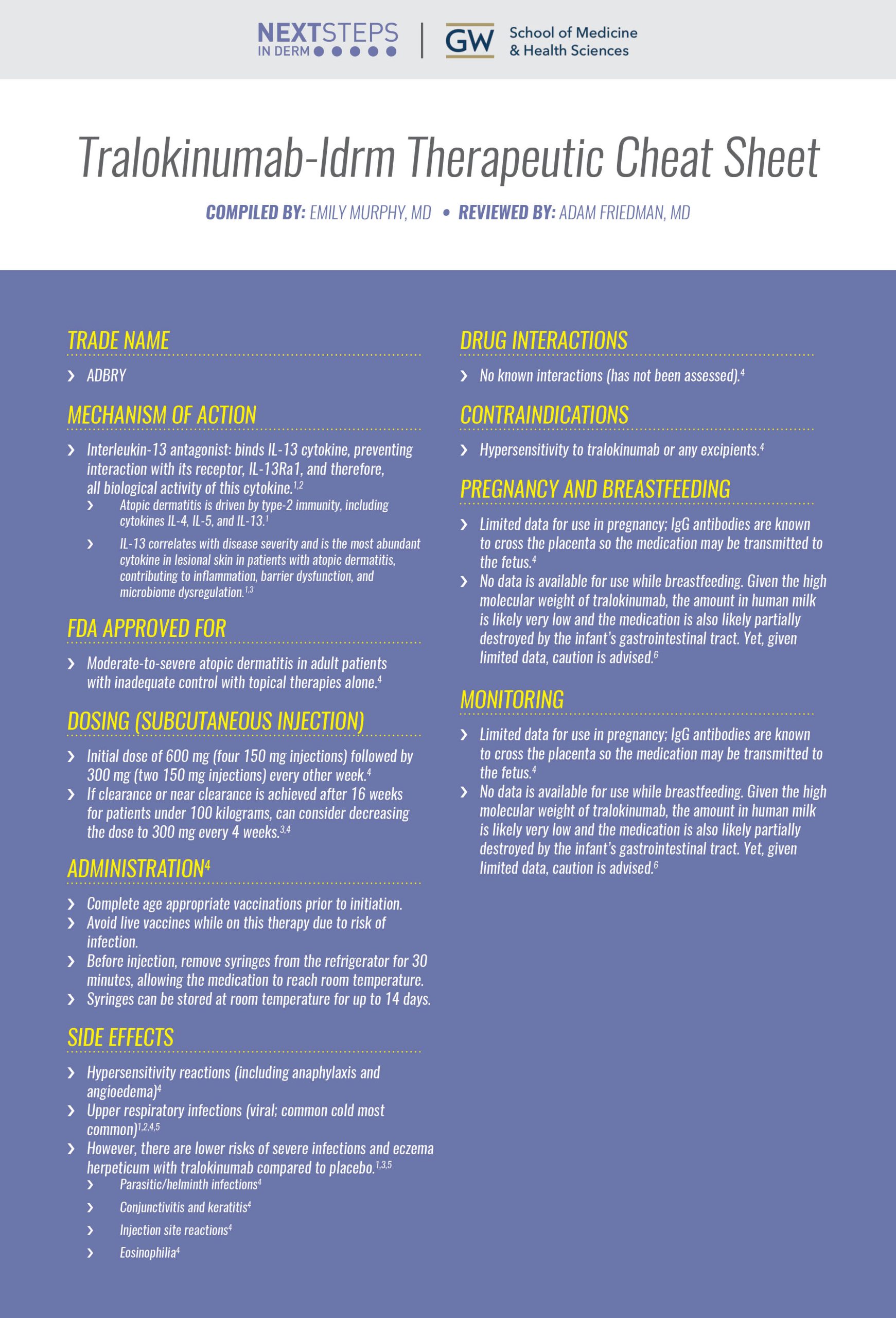
Tralokinumab-ldrm Therapeutic Cheat Sheet
Compiled by: Emily Murphy, MD, Reviewed by: Adam Friedman, MD
TRALOKINUMAB TRADE NAME
-
- ADBRY
MECHANISM OF ACTION
-
- Interleukin-13 antagonist: binds IL-13 cytokine, preventing interaction with its receptor, IL-13Rα1, and therefore, all biological activity of this cytokine.1,2
- Atopic dermatitis is driven by type-2 immunity, including cytokines IL-4, IL-5, and IL-13.1
- IL-13 correlates with disease severity and is the most abundant cytokine in lesional skin in patients with atopic dermatitis, contributing to inflammation, barrier dysfunction, and microbiome dysregulation.1,3
- Interleukin-13 antagonist: binds IL-13 cytokine, preventing interaction with its receptor, IL-13Rα1, and therefore, all biological activity of this cytokine.1,2
FDA APPROVED FOR
-
- Moderate-to-severe atopic dermatitis in adult patients with inadequate control with topical therapies alone.4
TRALOKINUMAB DOSING (SUBCUTANEOUS INJECTION)
-
- Initial dose of 600 mg (four 150 mg injections) followed by 300 mg (two 150 mg injections) every other week.4
- If clearance or near clearance is achieved after 16 weeks for patients under 100 kilograms, can consider decreasing the dose to 300 mg every 4 weeks.3,4
ADMINISTRATION4
-
- Complete age appropriate vaccinations prior to initiation.
- Avoid live vaccines while on this therapy due to risk of infection.
- Before injection, remove syringes from the refrigerator for 30 minutes, allowing the medication to reach room temperature.
- Syringes can be stored at room temperature for up to 14 days.
TRALOKINUMAB SIDE EFFECTS
-
- Hypersensitivity reactions (including anaphylaxis and angioedema)4
- Upper respiratory infections (viral; common cold most common)1,2,4,5
- However, there are lower risks of severe infections and eczema herpeticum with tralokinumab compared to placebo.1,3,5
- Parasitic/helminth infections4
- Conjunctivitis and keratitis4
- Injection site reactions4
- Eosinophilia4
DRUG INTERACTIONS
-
- No known interactions (has not been assessed).4
CONTRAINDICATIONS
-
- Hypersensitivity to tralokinumab or any excipients.4
PREGNANCY AND BREASTFEEDING
-
- Limited data for use in pregnancy; IgG antibodies are known to cross the placenta so the medication may be transmitted to the fetus.4
- No data is available for use while breastfeeding. Given the high molecular weight of tralokinumab, the amount in human milk is likely very low and the medication is also likely partially destroyed by the infant’s gastrointestinal tract. Yet, given limited data, caution is advised.6
MONITORING
-
- No lab monitoring required.
CLICK ON THE IMAGE BELOW TO ENLARGE AND/OR DOWNLOAD YOUR THERAPEUTIC CHEAT SHEET
FURTHER READING
If you would like to learn more about tralokinumab, check out the following articles published in the Journal of Drugs in Dermatology:
The Heterogeneity of Atopic Dermatitis
Abstract:
Background: Recent advances were made in characterizing the clinical heterogeneity of atopic dermatitis (AD).
Objective: To review the clinical domains contributing to AD heterogeneity and describe their importance in clinical practice.
Methods: We conducted a focused review of the published literature, including retrospective, observational, and prospective studies, clinical trials, and consensus guidelines.
Results: AD is associated with heterogeneous skin manifestations, symptoms, lesional severity, lesional extent, longitudinal course, burden of signs and symptoms, and comorbidities. Each of these domains characterizes a different aspect of AD and should be used to guide overall severity assessment and clinical management. Primary focus on any one specific clinical domain of AD is insufficient to describe the full burden of disease.
Conclusion: Heterogeneity should be routinely considered during AD clinical encounters.
J Drugs Dermatol. 2022;21(2):172.
Systemic Therapies for Moderate-to-Severe Atopic Dermatitis: Expert Perspectives in Practice
Abstract:
Atopic dermatitis (AD) is a chronic inflammatory skin disease that affects around 13% of children and 7% of adults in the US. It can have a significant impact on the quality of life (QoL) of affected individuals due to pruritus and the visibility of lesions on the skin. AD is increasingly recognized as a systemic disease, since dysregulation of the adaptive and innate immune systems plays a key role in the underlying disease pathogenesis, which has important implications for how the condition is treated. Patients with moderate-to-severe disease who have failed to achieve disease control may benefit from systemic immunomodulatory treatments. Recently published expert perspectives outlined recommendations for the diagnosis and treatment of moderate-to-severe AD in adults, reflecting evidence-based, practical recommendations to support allergists and dermatologists in selecting appropriate treatment in the era of biologic therapies. To help clinicians understand how these practical recommendations can be implemented into clinical practice, we describe two real life case studies of adult patients with AD. In these case studies, we demonstrate how AD severity, treatment response, and treatment failure can be assessed, and the role of emerging systemic treatments in the management of moderate-to-severe AD.
J Drugs Dermatol. 2019;18(2):122-129.
Catherine Buzney, Alice Gottlieb, David Rosmarin.
Abstract:
Type 2 helper T cell (Th2)-mediated inflammation plays a critical role in the pathogenesis of allergic asthma and atopic dermatitis (AD). Recent research focusing on the suppression of the Th2 axis with targeted inhibitors in atopic disease is showing promising early results. In particular, the simultaneous blockage of interleukin (IL)-4 and IL-13 has successfully mitigated symptoms of allergic asthma and AD in preliminary clinical trials. Given the current therapeutic challenges of treating these chronic and severe diseases, this review brings to light new data demonstrating that agents targeting IL-4 and IL-13 are relatively safe and effective medications in blocking the inflammatory cascade responsible for allergic asthma and atopic dermatitis.
J Drugs Dermatol. 2016;15(2):165-171.
IL-4 and IL-13 Inhibition in Atopic Dermatitis
Abstract:
Atopic dermatitis (AD) is a chronic, prevalent, multi-factorial condition that affects infants, children, and adults. Beyond topical therapy, a variety of systemic agents such as steroids, methotrexate, cyclosporine, azathioprine, mycophenoloic acid, and other agents are utilized to treat moderate to severe AD. However, these agents are associated with potential long term adverse events and organ toxicity. There is an unmet need for a safer, long-term systemic agent to adequately control moderate to severe AD. The role of the Th2 cytokines, IL-4 and IL-13, in AD has led to the development of biologic agents to treat AD. The aim of this article is to review the role of IL-4 and IL-13 in the pathogenesis of AD and discuss some of the clinical trial data that target and inhibit IL-4 and IL-13 in positively altering the course and outcome of AD.
J Drugs Dermatol. 2016;15(8):925-929.
References
-
- Wollenberg A, Weidinger S, Worm M, Bieber T. Tralokinumab in atopic dermatitis. J Dtsch Dermatol Ges. 2021;19(10):1435-1442. doi:10.1111/ddg.14545
- Duggan S. Tralokinumab: First Approval. Drugs. 2021;81(14):1657-1663. doi:10.1007/s40265-021-01583-1
- Silverberg JI, Toth D, Bieber T, et al. Tralokinumab plus topical corticosteroids for the treatment of moderate-to-severe atopic dermatitis: results from the double-blind, randomized, multicentre, placebo-controlled phase III ECZTRA 3 trial. Br J Dermatol. 2021;184(3):450-463. doi:10.1111/bjd.19573
- LEO Pharma Inc. Tralokinumab Package Insert. Published online December 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2022/761180Orig1s000lbl.pdf
- Wollenberg A, Blauvelt A, Guttman-Yassky E, et al. Tralokinumab for moderate-to-severe atopic dermatitis: results from two 52-week, randomized, double-blind, multicentre, placebo-controlled phase III trials (ECZTRA 1 and ECZTRA 2). Br J Dermatol. 2021;184(3):437-449. doi:10.1111/bjd.19574
- Tralokinumab. In: Drugs and Lactation Database (LactMed). National Library of Medicine (US); 2006. Accessed June 29, 2022. http://www.ncbi.nlm.nih.gov/books/NBK576870/
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.