As dermatologists, we understand that hidradenitis suppurativa (HS) can be a devastating disease that affects all aspects of our patients’ lives, influencing their physical health, ability to be active, and ability to be intimate. This disease disproportionately affects patients with skin of color and unfortunately, treatment can be challenging. We are lucky to have experts who dedicate their clinical and research efforts to this complex disease, including Dr. Ginette Okoye, Professor and Chair of Dermatology at Howard University College of Medicine. Channeling her clinical expertise, Dr. Okoye gave a fantastic, pearl-based lecture at the 2021 Skin of Color Update titled, “My Approach to Treating Hidradenitis Suppurativa in Patients with Skin of Color.”
Dr. Okoye started by emphasizing that the lecture is based on her clinical experience rather than data (and we are fortunate to have access to this expertise!). The lecture focused on four subtypes of HS:
-
- Axillary-mammary-inguinal
- Follicular
- Syndromic
- Gluteal
These four subtypes demonstrate the phenotypic heterogeneity of HS, including varying anatomic location and lesion type as well as cytokine profiles and genetic mutations. With this heterogeneity, the pathogenesis and treatment responses vary dramatically among these subtypes. To select the best therapy for your patient, Dr. Okoye asks three questions. First, what is your patient’s subtype? Second, are there triggers for the development of new lesions? And third, what comorbidities does your patient have? With this framework for approaching patients, Dr. Okoye dived into each subtype, focusing on the clinical features, pathogenesis, and treatment approach for each.
Axillary-mammary-inguinal subtype
-
- Clinical features: This subtype is what we think of as “classic” HS, where patients have disease on the breasts, axilla, mons pubis, and inguinal folds. Females are more commonly affected than males, and female patients often report hormonal fluctuations in disease severity. Of all the subtypes, this is the only one where patients may respond to weight loss. Despite this relationship to weight loss, Dr. Okoye emphasized that obesity is not the cause of patients’ disease, which is important for them to understand.
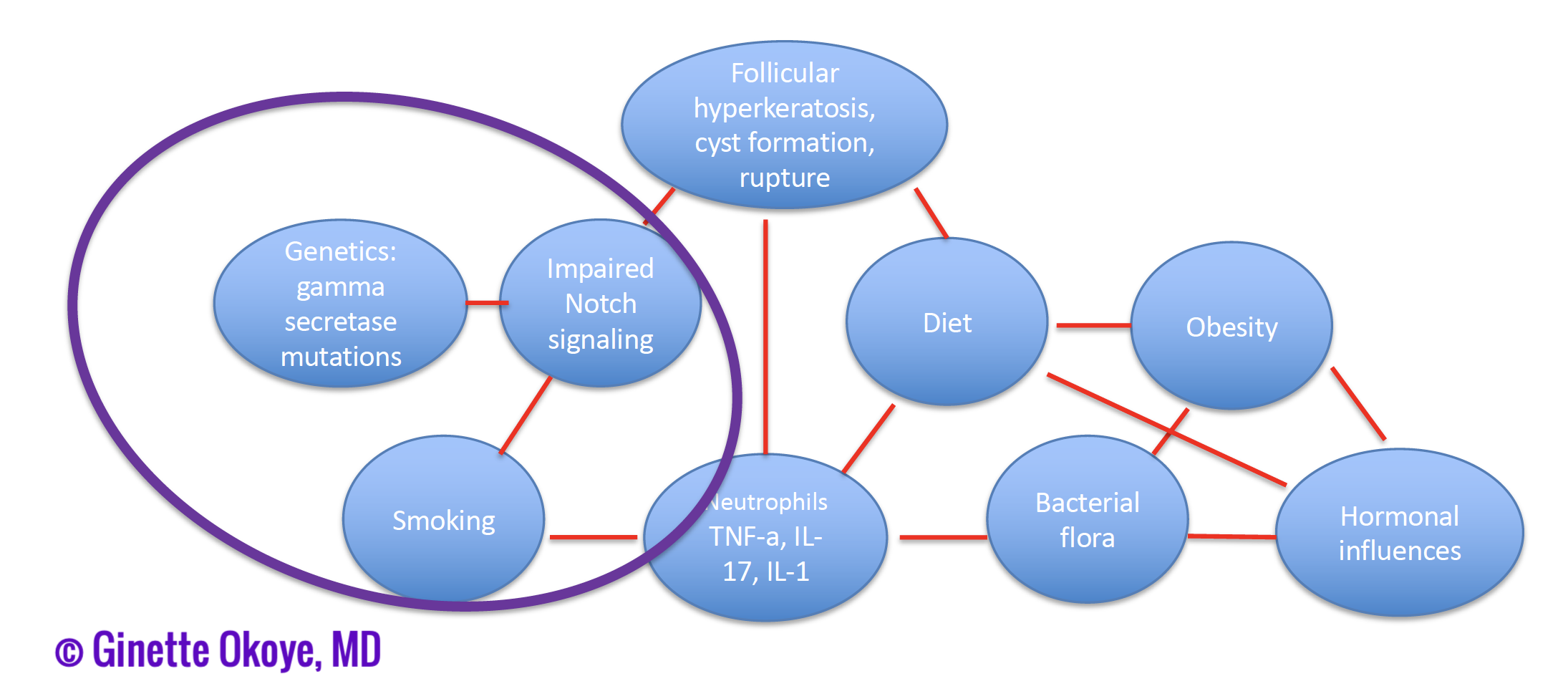
- Pathogenesis: as demonstrated in figure 1, the pathogenesis of this subtype may involve an interplay of hormonal influences, bacterial flora, obesity, and diet.
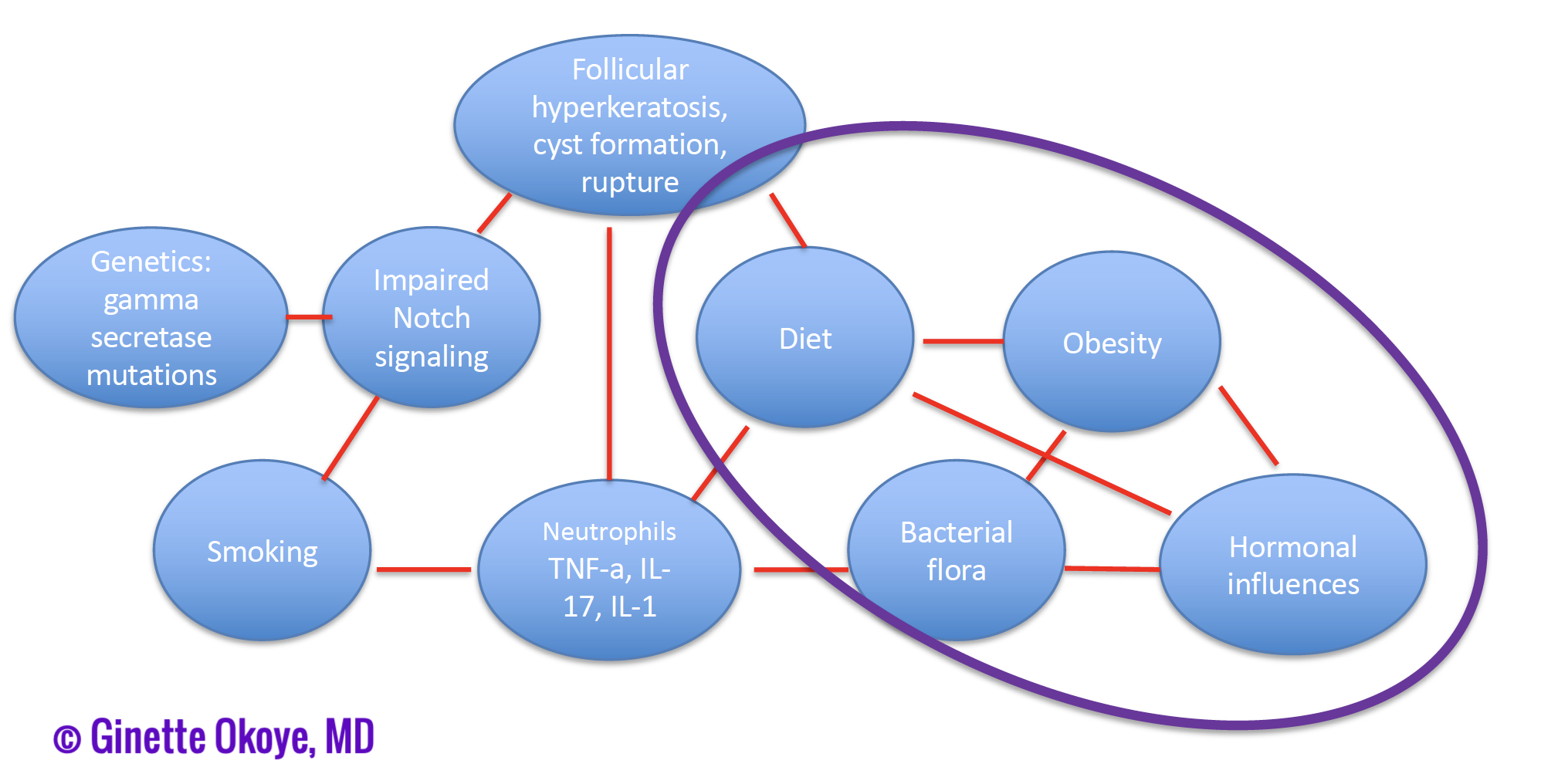
Figure 1. Pathogenesis of axillary-mammary-inguinal subtype of HS. - Treatment approach: given the pathogenesis of this subtype, patients should be treated with layered therapy, including anti-inflammatory therapy, hormonal therapy, and nutritional support/dietary modifications.
- Okoye focused on hormonal options including spironolactone (50 to 200 mg daily) and metformin (up to 2000 mg daily). Of note, for metformin, the extended release is often more tolerable due to fewer gastrointestinal side effects. Dr. Okoye chooses metformin for patients with metabolic syndrome, and spironolactone for patients with polycystic ovarian syndrome or who describe flares with their menstrual cycle. Oral contraceptive pills can also be used for patients who report prior positive experiences with this medication; however, it is critical to use oral contraceptive pills approved for acne, which are less androgenic.
- Laser hair removal can also be utilized to prevent disease recurrences, especially in patients with more mild disease where you may be able to halt disease spread.
- For nutritional support, if desired by patients, Dr. Okoye recommends a low carbohydrate/low glycemic index diet rather than naming specific diets.
- Treatment approach: given the relative lack of inflammation in this subtype, Dr. Okoye utilizes oral and topical retinoids in lieu of anti-inflammatory therapy.
- Retinoids: isotretinoin and acitretin can be used at acne dosing. Patients often require long-term, low-dose isotretinoin, such as 20 mg daily.
- Given smoking influences the pathogenesis, smoking cessation is critical!
- If epidermal inclusion cysts are located in cosmetically sensitive areas, early excision is important. Otherwise, avoiding surgical excision may be preferable to prevent a high scar burden.
Syndromic subtype
-
- Clinical features: patients have inflammatory syndromes, including PAPASH (pyogenic arthritis, pyoderma gangrenosum, acne, HS), PASH (pyogenic arthritis, HS), HS with inflammatory arthritis, and SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome.
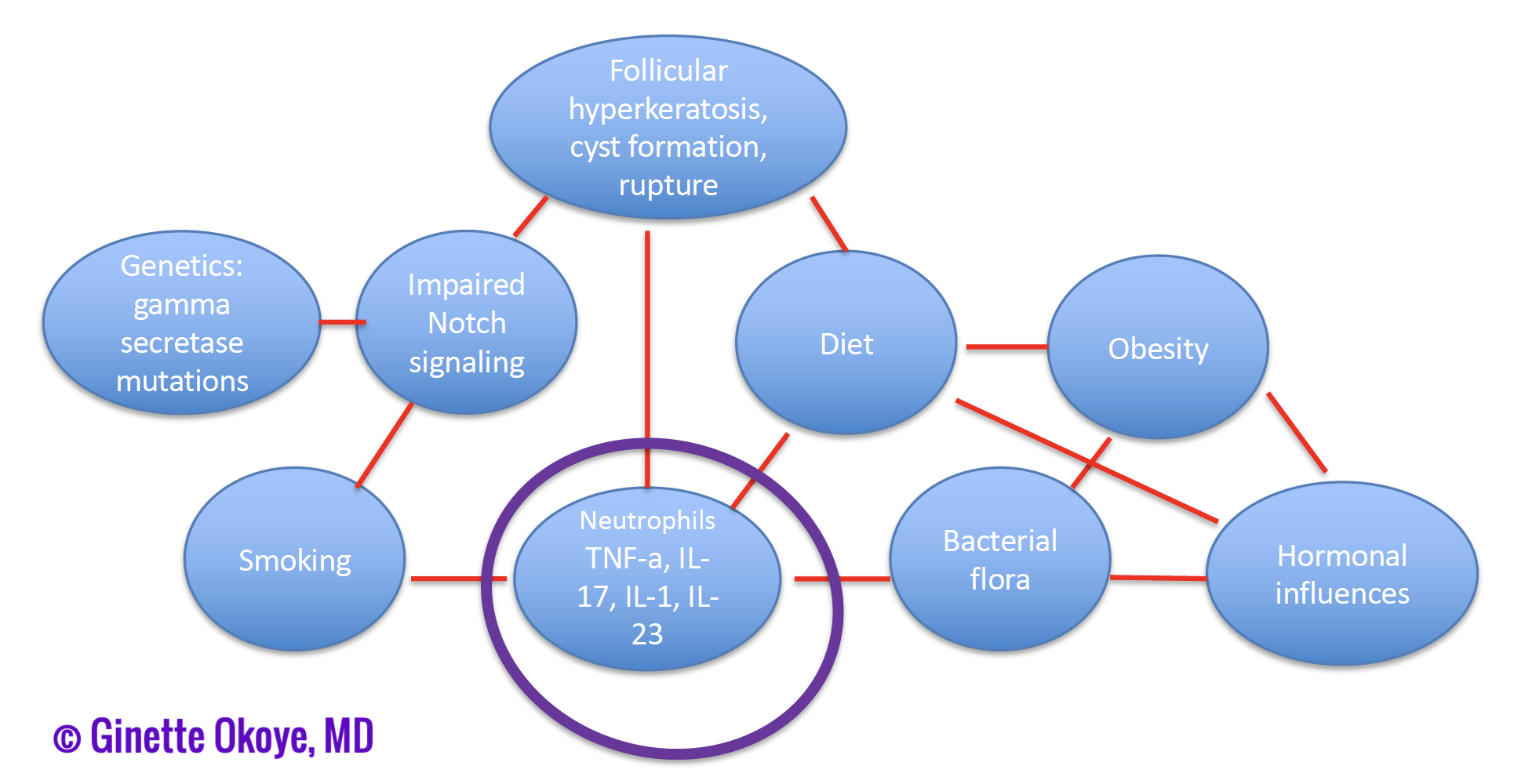
- Pathogenesis: inflammation is key in this subtype (figure 3).
- Treatment approach: given inflammation is central to the pathogenesis, biologic therapy along with prednisone are the mainstay treatments.
- Okoye’s therapeutic ladder for biologics is as follows:
- Adalimumab
- Ustekinumab or guselkumab (useful for ulcerative disease)
- Secukinumab (useful for inflammatory arthritis)
- Anakinra (especially for PASH or PAPASH, where IL-1 is upregulated)
- Prednisone can be used in two ways for severely affected patients, who otherwise could require hospital-based care:
- High dose (80 mg daily) with a prolonged, slow taper for acute control while starting a biologic therapy.
- Maintenance therapy along with a biologic agent: 20 mg once per week or 20 to 40 mg once at the start of a flare.
- Okoye’s therapeutic ladder for biologics is as follows:
Gluteal subtype
-
- Clinical features: as the name implies, this subtype predominantly affects the buttocks with follicular papules and folliculitis. Men are also more commonly affected than women in this subtype, similar to follicular HS. Patients often have a low body mass index and are current or former smokers. Long disease durations are seen, possibly complicated by squamous cell carcinoma (SCC). While Dr. Okoye admits the association between the gluteal subtype and SCC is not reported in the literature, patients with HS who develop SCC are often men who are smokers with prolonged disease in the buttocks, which is essentially the gluteal subtype.
- Pathogenesis: in some patients, Dr. Okoye feels this disease may actually be a severe, uncontrolled pilonidal cyst.
- Treatment approach: patients tend to respond to surgical excision rather than medical therapy, although a biologic therapy can be added after excision. In addition, smoking cessation is critical as well as surveillance for SCC.
In summary, patients with two lesion types will come to your clinic:
-
- Acute, painful, inflammatory nodules, which require anti-inflammatory therapies.
- Chronic sinus tracts, where surgical excision or marsupialization are needed.
With all these pearls, I hope you feel better prepared to tackle all patients with HS, whether it is the more classic, axillary-mammary-inguinal subtype, or the other subtypes, follicular, gluteal, and syndromic. These subtypes vary in presentation and pathogenesis, hence why different therapies are needed to treat patients successfully. By determining your patient’s subtype, triggers, and co-morbidities, you will be able to improve their disease and have a meaningful impact on their quality of lives!
Did you enjoy this article? You can find more on Medical Dermatology here.