With the advent of biologics, patients with moderate-to-severe plaque psoriasis have experienced increased control of disease and improved quality of life. Tumor necrosis factor (TNF) inhibitors are some of the earliest biologics prescribed for psoriasis, psoriatic arthritis and, more recently, hidradenitis suppurativa. In this month’s installment of Therapeutic Cheat Sheets, we discuss TNF inhibitors, their adverse effects, and monitoring recommendations.
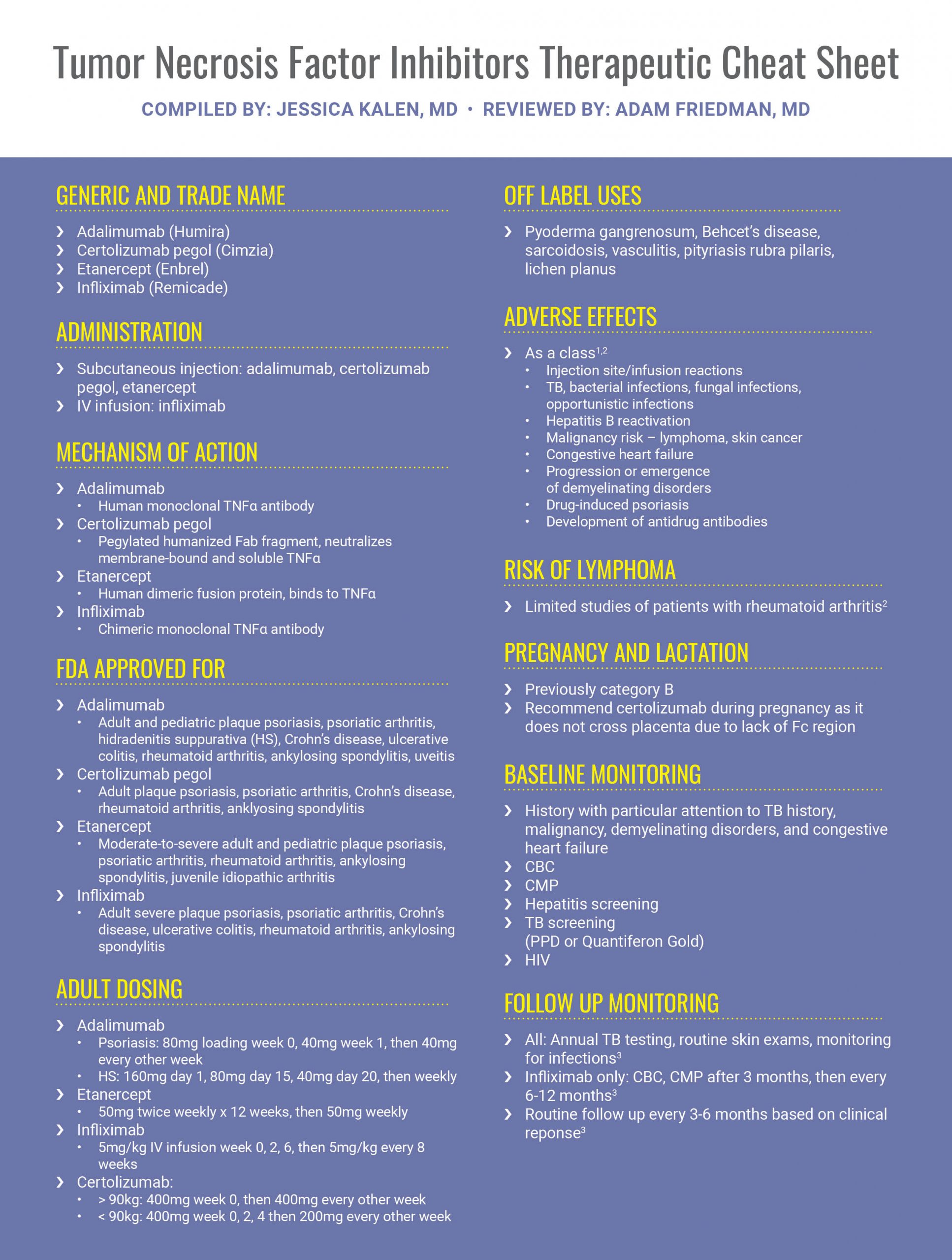
While there is an increasing number of biologics available for the treatment of moderate-to-severe plaque psoriasis, TNF inhibitors should be considered in patients who are pregnant or planning to become pregnant.
Further Reading
If you would like to read more about TNF inhibitors, below are several articles published in the Journal of Drugs in Dermatology.
 Adalimumab versus Rifampicin Plus Clindamycin for the Treatment of Moderate to Severe Hidradenitis Suppurativa: A Retrospective Study
Adalimumab versus Rifampicin Plus Clindamycin for the Treatment of Moderate to Severe Hidradenitis Suppurativa: A Retrospective Study
https://jddonline.com/articles/dermatology/S1545961619P0437X
In the present single-center retrospective study, we investigated our data to evaluate the efficacy of the classic antibiotic combination (rifampicin and clindamycin) compared to adalimumab treatment in patients affected by moderate-to-severe hidradenitis suppurativa. Disease severity and quality of life were registered using the modified Sartorious score and Hidradisk, respectively. Data were collected before starting treatment (T0) and after ten weeks of therapy (T10). The Mann-Whitney test was used to calculate statistical differences between baseline and week 10. P values less than 0.05 were considered to be statistically significant. A spearman test was used to evaluate the correlation among the parameters under study. Thirty patients (20 females, 10 males; mean age, 23.73 ± 4.57) were given the antibiotics: instead of starting the treatment by combining the two antibiotics, we recommend patients to start the therapy taking only rifampicin 300 mg twice a day for 7 days, and after the first week, to add clindamycin at a dose of 300 mg twice a day. The mean modified Sartorius Score before starting treatment was 68.8 while the value at week 10 was 57.8 (P equals 0.0052). The mean Hidradisk value before starting treatment was 74,73 while the value at week 10 was 62 (P equals 0.0095). Ten patients (10/30) achieved the HiSCR. On the other hand, thirty subjects (22 females, 8 males; mean age, 26.2±7.25) were treated with subcutaneous injections of adalimumab (160 mg at baseline, 80 mg at week 2, 40 mg at week 4, and 40 mg weekly thereafter). The mean modified Sartorius Score before starting treatment was 74.93 while the value at week 10 was 39.86 (P less than 0.0001). The mean Hidradisk value before starting treatment was 77.73 while the value at week 10 decreased to 51.86 (P less than 0.0001). Eighteen patients (18/30) achieved the HiSCR.
J Drugs Dermatol. 2019;18(5):437-438.
 Open-Label Study to Evaluate the Efficacy of Etanercept Treatment in Subjects With Moderate to Severe Plaque Psoriasis Who Have Failed Therapy With Apremilast
Open-Label Study to Evaluate the Efficacy of Etanercept Treatment in Subjects With Moderate to Severe Plaque Psoriasis Who Have Failed Therapy With Apremilast
https://jddonline.com/articles/dermatology/S1545961618P1078X
INTRODUCTION: Response to etanercept therapy in patients who have failed apremilast therapy has not been well characterized.
METHODS: In this multicenter, open-label, single-arm, phase 4, estimation study, subjects with moderate to severe plaque psoriasis received etanercept 50 mg SC twice weekly for 12 weeks, followed by etanercept 50 mg SC once weekly for an additional 12 weeks. Subjects had BSA greater than equal to 10%, PASI greater than equal to 10, and sPGA greater than equal to 3 at screening and baseline; and had failed apremilast—because of either failure to achieve or loss of adequate clinical response, or intolerability to apremilast in the opinion of the investigator. Primary endpoint was PASI 75 at week 12. Secondary endpoints included PASI 75 at week 24, PASI 90 at weeks 12 and 24, and patient-reported outcomes: Psoriasis Symptom Inventory (PSI) score (total and individual items) at baseline and weeks 12 and 24, and over time; DLQI responder analysis (5-point improvement in DLQI from baseline or score of 0) at weeks 12 and 24; and patient assessment of treatment satisfaction at baseline and weeks 12 and 24.
RESULTS: Among 80 patients, PASI 75 at weeks 12 and 24 was 41.6% (95% CI, 30.4%-53.4%) and 45.5% (34.1%-57.1%), respectively; PASI 90 was 13.0% (6.4%-22.6%) and 22.1% (13.4%-33.0%), respectively. Mean total PSI score (LOCF) improved from 16.6 (95% CI, 15.1-18.0) at baseline to 8.8 (7.3-10.2) and 9.6 (7.9-11.4) at weeks 12 and 24, respectively; improvements in item PSI scores were similar. The percentage of DLQI responders was 66.2% (95% CI, 54.3%-76.8%) and 57.3% (45.4%-68.7%) at weeks 12 and 24, respectively. The percentage of subjects who were satisfied/very satisfied with their psoriasis treatment improved from 5.0% at baseline to 60.8% and 53.3% at weeks 12 and 24, respectively. During the 24-week study, 23.8% and 2.5% of subjects reported an adverse event and serious adverse event, respectively; there were no new safety signals in this study.
DISCUSSION: In patients who have failed apremilast, etanercept may represent an effective therapeutic option. Trial Registration: ClinicalTrials.gov: NCT02749370 J Drugs Dermatol. 2018;17(10):1078-1082.
References
-
- Wolverton SE. Comprehensive Dermatologic Drug Therapy, 4td Philadelphia. Elsevier.
- Bolognia JK, Scahher JV, Cerroni L. Dermatology. Philadelphia: Elsevier. 2018
- Menter A et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. April 2019;80(4):1029-1072.
Did you enjoy this Therapeutic Cheat Sheet? You can find more here.