Broad spectrum tetracyclines are a well-known, widely used, and often successful treatment for use in inflammatory skin pathologies such as acne and rosacea. However, the steady rise of antibiotic resistance and gut dysbiosis associated with broad spectrum tetracyclines emphasizes the importance and responsibility of antibiotic stewardship. Narrow spectrum antibiotics have become increasingly important therapies to slow the progression of resistance as well as decrease negative side effect profiles, particularly those associated with broad spectrum tetracyclines. This case shows the successful treatment of periorificial dermatitis with a novel, narrow spectrum tetracycline, sarecycline, in a patient with underlying Crohn’s.
Introduction
Periorificial dermatitis (POD), also called perioral dermatitis, is described as tiny erythematous papules and pustules on a background of pink dry patches that appear almost eczematous. The eruption often occurs around the orifices of the face such as the mouth, nose, or eyes. Patients often describe pruritus or a burning sensation to the affected areas. While the pathophysiology of POD is not well understood, it is considered a variant of rosacea and its histopathology is similar to rosacea.1 Correlation to topical steroid misuse and changes in facial cosmetics, lotions, and washes have been reported.1,2 An association with fluorinated mouthwashes and toothpastes, as well as with inhaled corticosteroids has been suggested.2
Typical treatment for POD includes discontinuation of the offending agent (if known) as well as discontinuation of all facial topicals.3Mild disease may be treated with topical metronidazole or topical pimecrolimus. More severe disease is often treated with oral doxycycline.1,2,3 Since doxycycline is a broad-spectrum tetracycline, clinicians must take special consideration for patients with inflammatory bowel disease (IBD). Adverse gastrointestinal effects of doxycycline may be more pronounced in patients with IBD.4 Broad spectrum antibiotics may also cause gut flora dysbiosis that can have long lasting consequences – persisting even after stopping doxycycline.5,6 This case reports a significant improvement of POD in a patient with underlying Crohn’s disease using oral sarecycline, a relatively new, narrow-spectrum tetracycline that has not previously been reported for use in POD.
Case Presentation

In effort to decrease the likelihood of causing a Crohn’s flare secondary to broad-spectrum antibiotic use, the patient was prescribed the narrow spectrum antibiotic, sarecycline 100mg PO qday. Sarecycline was chosen because it is also a member of the tetracycline family and therefore, we hoped that it would have a similar effect on POD as doxycycline, yet without the side effects of a broad-spectrum antibiotic.
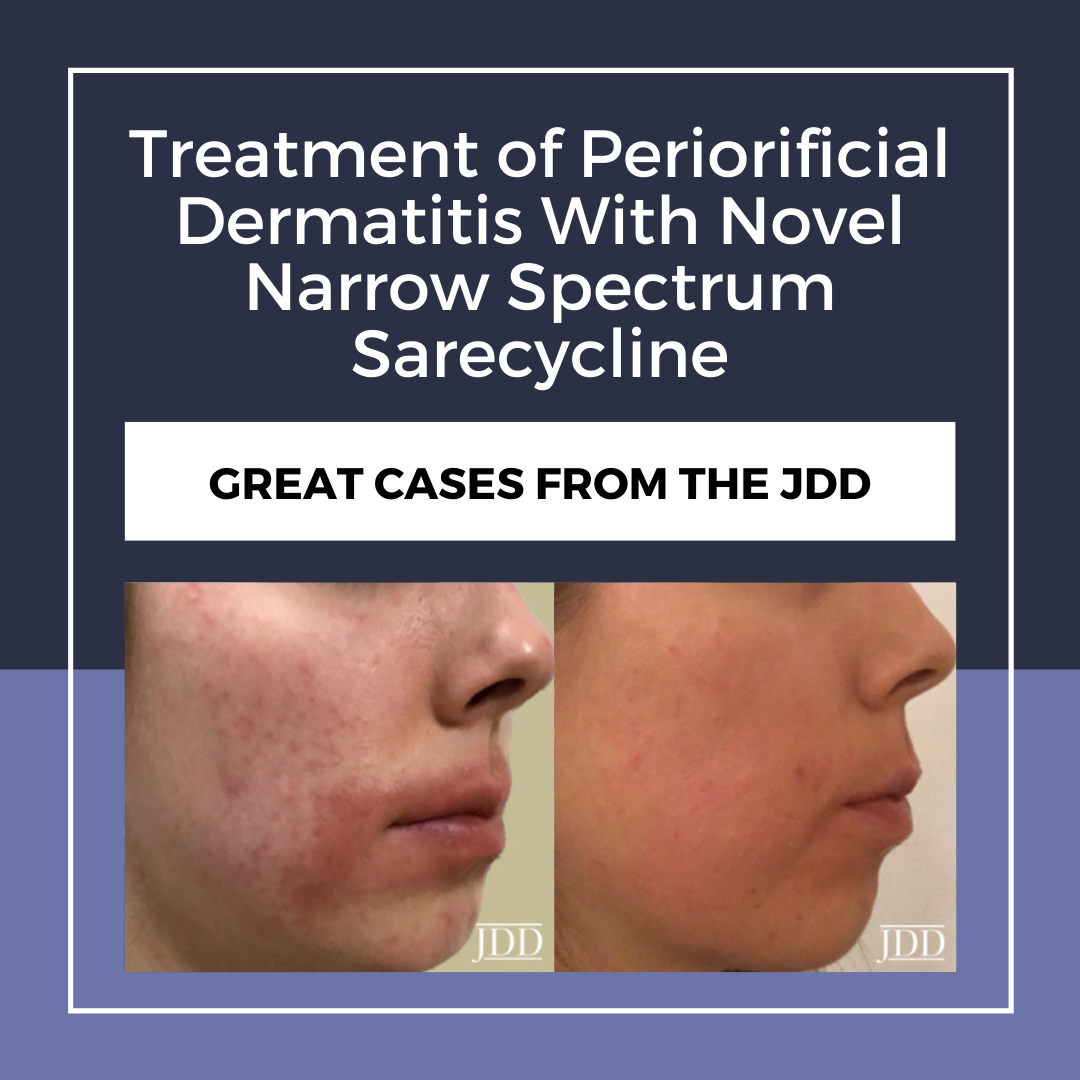
The patient returned to clinic five days after starting sarecycline and already had significant improvement of her POD and resolution of her burning symptoms. The patient denied gastrointestinal upset or any symptoms indicative of a Crohn’s exacerbation. Eight days later, the patient supplied photos demonstrating almost complete resolution of the periorificial dermatitis after only thirteen total days of sarecycline use (Figure 2).

Discussion
Sarecycline is currently only FDA-approved and indicated for moderate to severe acne vulgaris and is the only narrow spectrum antibiotic in the tetracycline family of antibiotics.5,6 As a narrow spectrum oral antibiotic, sarecycline targets grampositive bacteria linked with acne such as Cutibacterium acnes and has little to no effect on gram negative bacteria such as those comprising gut normal flora.5,6,7 Tetracycline, doxycycline, and minocycline have all demonstrated anti-inflammatory properties in addition to their antimicrobial effect.8,9 Although there are no published data about sarecycline’s anti-inflammatory activity, it is presumed that it shares this similar anti-inflammatory action with the other tetracyclines.7 POD is an inflammatory disorder and the standard treatment with doxycycline is presumed to work via its anti-inflammatory mechanisms.
Doxycycline’s anti-inflammatory mechanism of action includes down regulation of cytokines including TNF-α, interleukin-1β, and interleukin-63which decreases chemotaxis and inflammatory neutrophil response.3,8,9 The accepted treatment of the perifollicular and perivascular inflammation seen in POD with doxycycline2 paired with the successful treatment of symptoms using sarecycline, suggest that sarecycline has a similar mechanism of anti-inflammatory properties as doxycycline. More research on the mechanism of anti- inflammatory action of sarecycline may help elucidate the pathophysiology behind POD.
This case study also remarkably demonstrates safe use of sarecycline with no subsequent Crohn’s flare in a patient with known IBD. In contrast, the broad-spectrum tetracyclines have been reported to increase the risk of inflammatory bowel disease.6 Sarecycline’s inactivity towards gram-negative bacilli and anaerobic bacteria that compose the normal gut flora6 make it a narrow spectrum antibiotic that minimally disrupts the gut. Protection of normal gut flora may encourage providers to choose sarecycline treatment of acneiform inflammatory skin conditions in patients with underlying IBD and prompt further investigation. Additionally, sarecycline has shown low gastrointestinal side effects in phase 3 studies reporting nausea in 1.9%, dizziness in 0.4%, vomiting in 0.6%, diarrhea in 1.2%, and esophagitis in 0% of participants.5 Sarecycline may be a consideration as providers choose a therapy that decreases negative side effects and discomfort for patients.
Finally, sarecycline adds an important piece to the ever-growing concern about antibacterial resistance-particularly tetracycline resistant bacteria. Sarecycline showed lower spontaneous mutation frequency in comparison to doxycycline and minocycline.6 The decreased spontaneous mutation frequency paired with gram-positive microbial targeting suggests that sarecycline is an option that supports responsible antibiotic stewardship for inflammatory skin conditions and calls for further investigation into the possible alternative to overuse of broad spectrum tetracyclines. This is the first published case to demonstrate successful use of sarecycline to treat POD. Additionally, we have shown that it was well tolerated, even in a patient with IBD.
Disclosures
References
-
- Lipozencic J, Ljubojevic, S. Periorificial dermatitis. Clin Dermatol. 2011;29(2):157-161. https://doi.org/10.1016/j.clindermatol.2010.09.007.
- Tolymat L, Hall M. Perioral dermatitis. In: StatPearls. Treasure Island (FL): StatsPearls Publishing; 2020. https://www-ncbi-nlm-nih-gov.proxy.pnwu.org/ books/NBK525968/#article-26998.s8. Accessed June 01, 2020.
- Del Rosso J. Management of papulopustular rosacea and perioral dermatitis with emphasis on iatrogenic causation or exacerbation of inflammatory facial dermatoses: Use of docycyline-modified release 40mg capsules once daily in combination with properly selected skin care as an effective therapeutic approach. J Clin Aesthet Dermatol. 2011;4(8):20-30. https://www-ncbi-nlm- nih-gov.proxy.pnwu.org/pmc/articles/PMC3168247/. Accessed June 01, 2020.
- Doxycycline. AccessMedicine. https://accessmedicine-mhmedical-com. proxy.pnwu.org/drugs.aspx?gbosID=426591#monoNumber=426591§i onID=243239068&tab=tab0. Updated 2020. Accessed June 01, 2020.
- Moore AY, Charles JE, Moore S. Sarecycline: a narrow spectrum tetracycline for the treatment of moderate-to-severe acne vulgaris. Future Microbiol. 2019;14(14):1235-1242. https://doi.org/10.2217/fmb-2019-0199.
- Zhanel G, Critchley, Lin L, Alvandi N. (2018). Microbiological profile of sarecycline, a novel targeted spectrum tetracycline for the treatment of acne vulgaris. Antimicrob Agents Chemother. 2018;63(1):1297-18. https:// doi.org/10.1128/AAC.01297-18.
- Kaul G, Saxena D, Dasgupta A, Chopra S. Sarecycline hydrochloride for the treatment of acne vulgaris. Drugs Today. 2019;55(10),615-625. https://doi. org/10.1358/dot.2019.55.10.3045040.
- Di Caprio R, Lembo S, Di Costanzo L, et al. Anti-inflammatory properties of low and high doxycycline doses: An In Vitro Study. Mediators Inflamm. 2015. https://doi.org/10.1155/2015/329418.
- Ishikawa C, Tsuda T, Konishi H, et al. Tetracyclines modulate protease- activated receptor 2-mediated proinflammatory reactions in epidermal keratinocytes.Antimicrob Chemother. 2009;53(5):1760-1765. https://doi. org/10.1128/AAC.01540-08.
Source
Graber, E., & Kay, C. R. Successful Treatment of Periorificial Dermatitis With Novel Narrow Spectrum Sarecycline. Journal of drugs in dermatology: JDD, 20(1), 98-100.
Content and images used with permission from the Journal of Drugs in Dermatology.
Adapted from original article for length and style.
Did you enjoy this case report? Find more here.