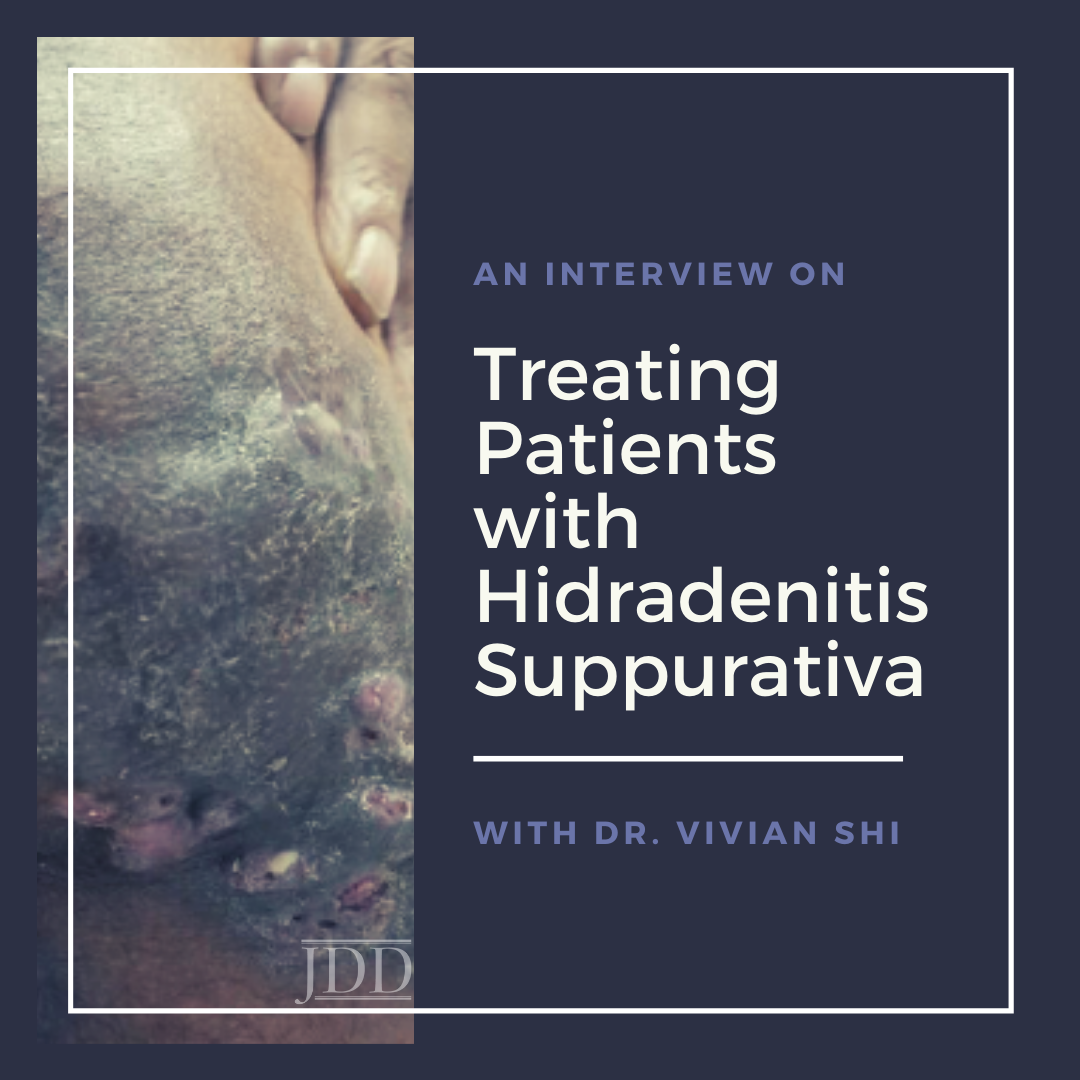
In this interview with Dr. Vivian Shi, Associate Professor of Dermatology at the University of Arkansas for Medical Sciences, I share her words of wisdom and practical pearls for treating patients with hidradenitis suppurativa (HS), a chronic inflammatory disease with recurrent painful nodules affecting intertriginous skin. Dr. Shi has published over 150 peer-reviewed articles and is the editor for two reference dermatology textbooks on atopic dermatitis and hidradenitis suppurativa. Dr. Shi has started the first Hidradenitis Suppurativa Specialty Clinic in Arkansas and is on the Board of Directors for the Hidradenitis Suppurativa Foundation.
Dr. Newton: We are so excited to have you joining the Department of Dermatology at UAMS because of the expertise and research passion you bring to these areas of dermatology. Today I would like to pick your brain specifically about practical tips and insights in the treatment of hidradenitis suppurativa. But first, what drew you to this area of Dermatology?”
Dr. Shi: For me, it’s really the interest in complex chronic inflammatory diseases. Taking care of atopic dermatitis patients was my initial entry into Dermatology, and now we have really good medications for atopic dermatitis. My involvement in HS came later; caring for HS fell on my shoulders when I was at the University of Arizona. These patients lack principal providers and have really fragmented care. They bounce between providers. A lot of patients live with very burdensome symptoms for decades without ever hearing the words “hidradenitis suppurativa”. Compared to atopic dermatitis and psoriasis, I think the world of HS is still in its infancy, and there is a lot of work to do. That is what really sparked my interest — the desire to serve an unmet need. After moving to Little Rock, I realized the unmet need is even bigger here in the South. So hopefully together with our residents, colleagues, and nursing staff, we can do some good work!
Dr. Newton: What are some of your preferred therapies, from topicals to short term systemic agents for your Hurley stage I patients?
Dr. Shi: For mild patients, they may not need a systemic prescription. I emphasize lifestyle modification, such as stress reduction, smoking cessation, choosing the right underwear to prevent friction and occlusion, finding the right diet with low glycemic index and less dairy, and weight loss for some individuals. Not all hidradenitis suppurativa patients are overweight, but for those who are, it can help to decrease their inflammatory burden. I also like to do nonprescription trace minerals and vitamins, such as zinc and nicotinamide. Those are the gateway complementary treatments prior to/in conjunction with prescription medications.
Dr. Newton: Can you walk me through your treatment algorithm for the more severe HS patients?
Dr. Shi: Not all of the severe patients that come to us are actually treatment-naive. It is important to find out what they have tried, to see what has worked and what didn’t work. I have mentioned fragmented care. Many of them tried things in serial order, but really haven’t tried things in combination, like a “toolbox”. There is no one-size-fits-all treatment plan. At very minimum, we start with topical antibiotics, systemic antibiotics- sometimes combination antibiotics. I rotate systemic antibiotics to prevent bacterial resistance. Women are candidates for hormonal modulation (i.e., if a hormonal component is suspected), combined contraception pills and spironolactone can block androgen effects associated with HS. I discuss the options for systemic treatment with an immunomodulator such as adalimumab, early on with HS patients so they are aware of all the treatment options. Medical treatment has to go in parallel with surgical treatment because medical therapy has limited efficacy in patients with severe anatomical changes (i.e., extensive scarring, sinus tracts, and fistulas). Recent studies have shown tunnels, sinus tracts, and fistulas are very much immunologically active and are actually a source of cytokines. So making a referral to surgery colleagues early on and pursuing collaborative management is really important.
Dr. Newton: What treatment options exist for pregnant women with moderate to severe HS?
Dr. Shi: HS occurs in people of reproductive age and is more common in women, so they are a population that needs special consideration. There are no clinical trials targeted for pregnant women with HS, but what we do know comes from the registries and case reports. Topical antibiotics, such as clindamycin and erythromycin, are generally safe. Some antibiotics are contraindicated during pregnancy and breastfeeding, like the tetracycline family. With antibiotics, I would go for the penicillin and cephalosporin families, such as cephalexin. Hormonal modulation is also not an option during pregnancy. Localized surgery is reasonable if indicated. Intralesional steroid injection is also an option. In terms of biologics, adalimumab has the most data, not surprisingly, as it has been approved for use the longest. Adalimumab is an IgG antibody that can cross the placenta, and a majority of the crossing occurs in the third trimester. So, in theory, it is safer in the first and second trimesters. I would recommend treating up until the third trimester with adalimumab and then discontinuing. Other nonsystematic options include laser treatment and photodynamic therapy. It is important we treat the pregnant HS patient in conjunction with their obstetrician, and it is imperative to have a line of communication with their provider.
Dr. Newton: Men can also be severely affected by HS. What unique treatment options are available to this patient group?
Dr. Shi: Men typically are less likely to seek treatment than women, so they usually present with a more severe disease state by the time they come in for evaluation. They also tend to present with more dorsal or posterior involvement of their bodies, as opposed to women that are affected more on the anterior side. An active area of research interest in the HS community is to identify potential gender differences in presentation and pathophysiology.
Dr. Newton: When is the right time to pursue surgical excision (i.e., wide local excision)?
Dr. Shi: I prefer to get the inflammatory burden down with medications first before having extensive surgery. We can think of active HS disease like a wildfire; surgery and post-operation healing can add gasoline to the fire. However, referring the patient to surgery early on in the disease is also important so they can be connected and educated. It is about finding the balance. Before surgery, my goal is to reduce the inflammatory burden by about a quarter to optimize the procedure results. By inflammatory burden, I am often referring to drainage and pain, which can be quantifiable by the patient based on how much gauze or pads they use per day on the affected areas. Any time you have tunnels, fistulas, and contracted scars, the patient is going to eventually need surgery.
Dr. Newton: How do you address the pain component of this disease?
Dr. Shi: Recently pain in HS has been at the forefront of attention. The first step in management is decreasing the inflammatory burden and targeting the disease itself. Targeting the pain alone has not been successful in HS. In addition to the HS treatment paradigm, we have a toolbox of treatments to mitigate pain. Epson salt baths and warm compresses have shown to be helpful in patient-reported surveys. These make up the foundation tier treatments, along with over the counter NSAIDs and acetaminophen. The next step is prescription medications- which include gabapentin, SNRIs, SSRIs, and tramadol. Surprisingly, opioids do not seem to help HS that much, and often patients experience nausea with associated opioid use. Early studies are showing acupuncture to be effective for chronic pain associated with HS. There are also ongoing studies examining cannabinoids for HS- both topical and systemic. Those are up and coming options that will increase the size of our toolbox.
Dr. Newton: What non-pharmacologic therapies have evidence in treating HS?
Dr. Shi: We talked about lifestyle modification including smoking cessation and weight loss. For patients with BMI >35 and specific obesity-related co-morbidities or BMI >40, I have a low threshold to refer patients for bariatric surgery evaluation if they have been unsuccessful at weight loss. There is also promising data for zinc and nicotinamide supplementation. Bleach bath is something we do not necessarily use for antimicrobial effects since the dilute baths are not strong enough to kill bacteria, but bleach in vitro can reduce neurosensory transmission by reducing calcium release. This can decrease neuronal transmission of itch and pain. Dilute bleach can also reduce inflammation by inhibiting the NFkB pathway. Epson salt bath can also be helpful. Magnesium supplementation— under close supervision— has shown to reduce post-delivery pain in women after childbirth so it can potentially be helpful in HS pain.
Dr. Newton: I think sometimes when providers see they have a severe HS patient on the schedule, they almost feel defeated because they don’t often feel like they leave the patient in a better state in terms of their disease. What are some tips you have for managing HS patients in your practice?
Dr. Shi: That’s the million-dollar question! I think one of the biggest challenges in HS is for one, we do not have really effective monotherapy. And two, social circumstances with patients, often complicated by lower health literacy make treatment adherence challenging. It’s not just on the patient side- we, the providers, carry the responsibility to understand the barriers and determine what is culturally and socioeconomically feasible for the patient before we can have a successful relationship.
When you first meet the patient, you need to take time to discover what hasn’t worked and why. Commonly it is due to mistrust of the system. By the time patients come through our HS clinic, we may be the fifth or sixth person they have seen. They have heard about clindamycin and doxycycline, but no one has given them the full picture to understand what the journey of an HS patient is like. One thing we have to determine is what are the short term and long term goals for them when working with an HS specialty clinic. We want to break the barrier and comprehensively design an individualized plan for them. Seeing these HS patients regularly is important and getting educators involved- not necessarily a physician, but also nurses and even research educators that are available to metamorphically hold their hand through the process.
It is important not to feel defeated. You can’t climb Mount Everest in a day. Seeing HS patients frequently and having small achievable goals is vital. I don’t throw everything at them during the first or second visit. I try to limit it to about 3-4 things per visit and slowly add on. I am very honest with patients that we cannot cure HS, but the goal is to design a toolbox so the flares are less frequent and smaller in amplitude until new effective treatments become available.
Dr. Newton: Any last tip to share that we haven’t addressed?
Dr. Shi: Patients are wound care experts; they are the true experts in their own skin. They live with hidradenitis suppurativa every day. We have a lot to learn from patients in how they manage their skin. It is also important to cultivate opportunities and interest in students and trainees to foster enthusiasm, or at a minimum reduce aversion, about caring for HS patients. Hopefully, with the help of non-profit organizations and industry partners, we can find funding and support to bring early education and awareness about this condition to the medical field.
About Dr. Vivina Shi
Dr. Vivian Shi is a board-certified dermatologist and associate professor of dermatology at the University of Arkansas for Medical Sciences. Her clinical and research interests include inflammatory skin diseases such as atopic dermatitis, hidradenitis suppurativa, skin barrier repair, and integrative dermatology. She directs the Eczema as well as Hidradenitis Suppurativa Specialty Clinics at her institutions and has served as the principal investigators for numerous clinical and translational studies.
Did you enjoy this article? Find more on Medical Dermatology here.