Dr. Shari Lipner, Associate Professor of Clinical Dermatology and Director of the Nail Division at Weill Cornell Medicine and President of The Dermatologic Society of Greater New York, shared her expertise of nail disorders in patients with skin of color: from nail psoriasis and onychomycosis to subungual melanoma.
Dr. Lipner’s lecture focused on the following key points (spoiler alert!):
Key messages:
-
- Images of common conditions in patients with skin of color are lacking in both patient and physician education.
- Clinical trials are starting to report more ethnicity/race data, but we have a long way to go before accurately reflecting the diversity within the United States.
- Patients with darker skin often go too long before nail psoriasis is diagnosed and treated.
- The first line of treatment for
 limited nail psoriasis is intralesional Kenalog. Consider diluting ILK with lidocaine to get to a concentration of 2.5mg/mL and
limited nail psoriasis is intralesional Kenalog. Consider diluting ILK with lidocaine to get to a concentration of 2.5mg/mL and
using an Ethyl Chloride cooling spray to reduce pain with injections. (See photo) - Consider oral anti-fungal treatment for onychomycosis if: there is distal lateral subungual onychomycosis covering >50% of surface area, nail is 2mm in thickness or greater, and/or there is matrix involvement
- In longitudinal melanonychia, consider a nail matrix biopsy if the width is >40% of the nail and/or there is brown background on dermoscopy with irregular brown lines (regarding lines, thickness and spacing)
LESSON #1: Images of nails in patients with skin of color fail the “google search” test.
According to Dr. Google:
Googling (nearly any) dermatologic condition will reveal a significant lack of images of patients with skin of color ¹¯³. This includes not only Google but also the American Academy of Dermatology’s website for patient education and dermatologic textbooks. Dr. Lipner highlighted a study showing that only 1 of 6 textbooks demonstrated a greater than 1% increase in inclusion of Fitzpatrick skin types V and VI between 2006 and 2020, and 50% of textbooks excluded skin of color images of common conditions². This study was part of a call to action for more diverse images in textbooks. Emerging resources have proved valuable for visualizing skin conditions in all skin types: (visualdx.com, skinofcolorsociety.org are example resources).³
LESSON #2: Nail psoriasis more severely impacts darker-skinned patients
Psoriasis in patients with skin of color is often more severe with a greater impact on quality of life. Unfortunately, patients with darker skin types are diagnosed later, conferring more significant morbidity and quality of life impairment.
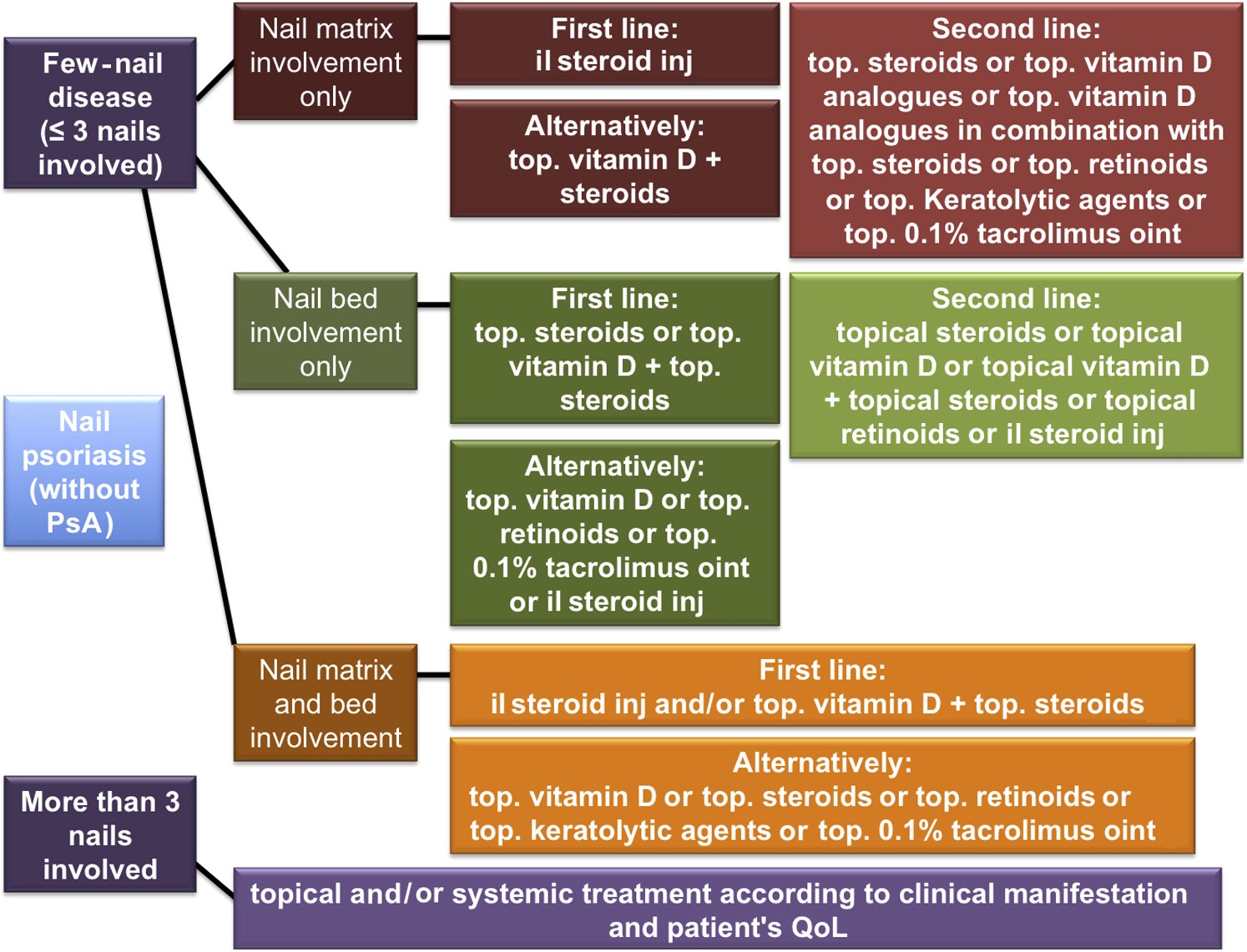
A recent consensus of nail experts evaluated treatments for nail psoriasis4. They recommended the following:
-
- ≤ 3 nails involved: Intralesional Kenalog is first-line treatment (with a focus on the nail matrix)
- >3 nails involved: consider the patient and burden of disease regarding topical vs. systemic therapy
- Nail bed involvement: start with topical steroids and/or vitamin D analogues
Nail Psoriasis algorithm:4
Although more traditional methods for ILK injection involve digital nerve block and concentration of 10mg/mL kenalog, Dr. Lipner and Scher developed an alternate technique:
-
- Inject 2.5mg/mL, dilute in 1% lidocaine
- Use ethyl chloride “cooling” spray for anesthesia
- Use “talkesthesia” while simultaneously injecting 10 fingers in <60 seconds
Other pearls:
-
- Treat nails for at least 6 months prior to determining success or failure
- Biologics may be slightly more effective than methotrexate, cyclosporine, acitretin, and apremilast
LESSON #3: Onychomycosis is the most common nail disorder seen in clinical practice
Onychomycosis may present as a diagnostic dilemma in patients with darker skin tones because the presence of longitudinal melanonychia may muddy the picture. Unfortunately, this means that onychomycosis can get missed, resulting in patients presenting with more severe disease.
Here is an excellent table of FDA approved oral medications for onychomycosis with associated cure rates5:
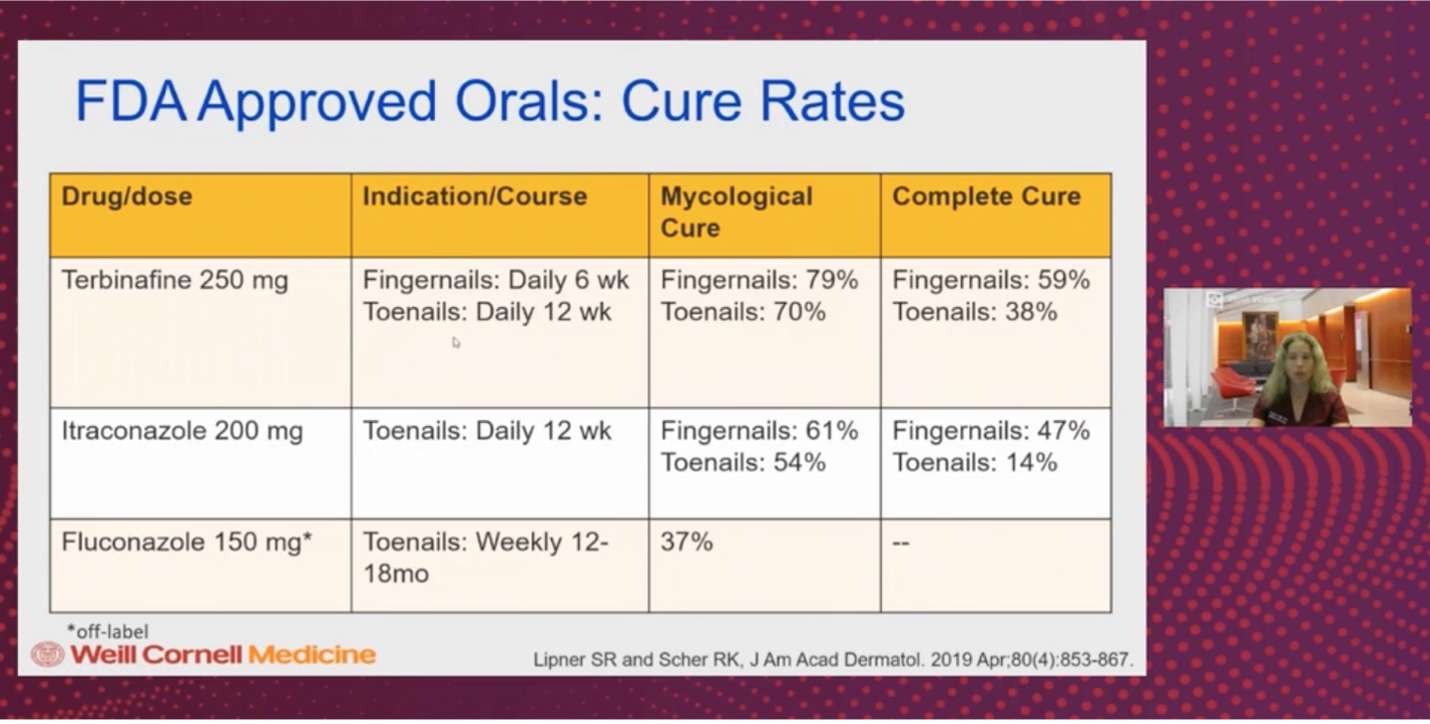
Regarding oral therapy, terbinafine has the highest cure rates. Itraconazole is FDA approved but carries the risks of cardiotoxicity and many drug-drug interactions. Griseofulvin is also FDA-approved but has fallen out of favor due to other more effective alternatives. Oral fluconazole is used off-label and is dosed weekly for > 1 year but can be helpful when candida is present.
Luckily, when prescribing terbinafine, we do not need to trend LFTs and CBCs in healthy patients less than 65 years old while they are on therapy6. This includes healthy pediatric patients7.
FDA approved topical therapies include:
-
- Ciclopirox 8% daily for 1 year—-of note, you have to remove the lacquer every week.
- Efinaconazole 10%— daily for 1 year. It has a higher cure rate and is now FDA approved for pediatric patients
- Tavaborole 5% —daily for 1 year. Also, with a higher cure rate and FDA approved for children.
LESSON #4: use specific parameters when considering oral vs. topical therapy for onychomycosis
Consider oral therapy when:
-
- Distal lateral subungual onychomycosis (DLSO) covers >50% of the surface area of the nail
- Nail thickness of 2mm or greater
- Nail matrix involvement
- 5 or more nails are involved
- Patient has poor prognostic factors such as diabetes mellitus and immunosuppression
- Proximal subungual onychomycosis
Consider topical therapy when:
-
- DLSO <50% surface area
- nail thickness <2mm
- no matrix involvement
- superficial infection
- pediatrics (who have thin/faster-growing nails)
- <5 nails involved
LESSON #5: Consider nail matrix biopsy when longitudinal melanonychia is >40% of nail width
Longitudinal melanonychia (LM) is common in patients with darker skin types. It is defined as longitudinally oriented brown/black band(s) extending the length of the nail plate.
When determining how to evaluate LM, remember that lesions appearing “brown” are not always melanocytic. Non-melanocytic reasons for dark discoloration of the nail include hemorrhage and onychomycosis. Dr. Lipner, however, focused on melanocytic lesions in her talk.
Melanotic Macule is the #1 cause of melanin-derived longitudinal melanonychia in adults
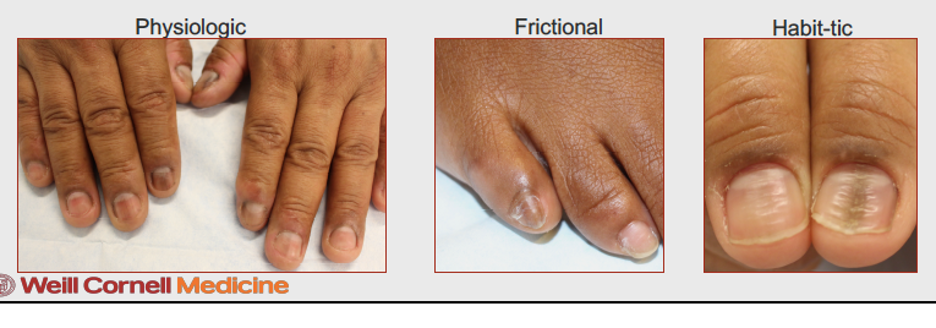
Regarding melanotic macules, our brains should think of these processes:
A. “Melanocytic activation” consisting of a normal number of melanocytes increasing their production of melanin (sometimes due to external trauma).
Causes:
-
- Physiologic – common in skin of color patients
- Frictional (especially 4th and 5th toenails)
- Behavioral: Habit-tic deformities
B. Inflammatory conditions causing longitudinal melanonychia:
In a recent study of Lichen planus patients—Longitudinal melanonychia was the second most common nail plate finding, present in 89% of patients8. #1 was onychorrhexis, seen in 100% of patients. Interestingly, this study featured a majority of patients with Fitzpatrick skin type IV and above, which could have partially accounted for the high incidence of longitudinal melanonychia.
C. Dermoscopy of longitudinal melanonychia:
We need to take longitudinal melanonychia (LM) seriously. It accounts for 0.7-3.5% of melanoma cases, confers a worse prognosis in the nail, and is the most common sign for nail unit melanoma. One of the tools we can use to assess LM is dermoscopy. Benign lesions typically have a gray background or brown background with uniform lines. LM which are wide, taper distally (are wider at the base- a sign of growing melanoma), or involve the nail folds or hyponychia should raise our concern for melanoma9. Under dermoscopy, these lesions of LM often have irregular brown lines in terms of color, thickness, and spacing (see photos below).
Dr. Lipner and colleagues performed a study looking at LM in benign vs. malignant cases. The table below summarizes key findings10.
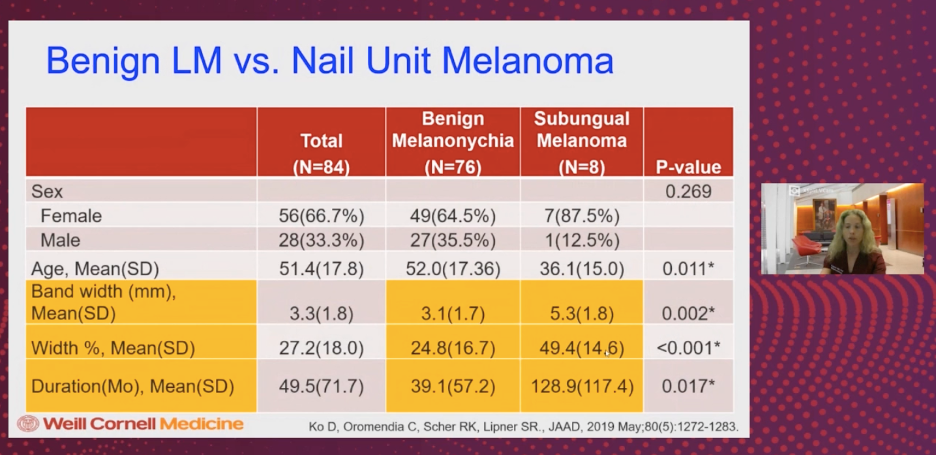
Dr. Lipner emphasized the following:
The % of nail width taken up by LM may be more specific and just as sensitive for picking up cases of nail unit melanoma:
-
- If using an LM width cut off of >3mm: 90% of melanomas were captured, but also 60% of benign LM were captured.
- BUT using a cut off of LM, which involved >40% of nail width, only captured 17% of benign cases and still 90% of nail unit melanomas
Therefore, band width and band width percentage may be important predictors of nail unit melanoma. These factors may guide us in our decision to perform a nail unit biopsy.
Dr. Lipner’s paper also emphasized the use of the “ABCDEF” rule in distinguishing longitudinal melanonychia vs. subungual melanoma11:
ABCDEF rule for distinguishing longitudinal melanonychia vs subungual melanoma:
A – Age- peak incidence in 5th-7th decade
A also stands for: African American, Asian, and Native American
B- Breadth >3mm, Brown to Black discoloration, Borders (variegated)
C- Change
D- Digit most commonly involved (thumb > hallux> index finger > single digit> multiple digits)
E- Extension of pigment onto proximal or lateral nailfold (Hutchinson sign), or free edge of nail plate
F- Family history of melanoma or dysplastic nevi
Lastly, Dr. Lipner’s slides referenced a 2002 cohort study performed by Ronger and colleagues evaluating 148 consecutive cases of LM over a 4-year period in an outpatient clinic12. They described patterns of longitudinal melanonychia and determined the relationship of these patterns with benign LM vs. melanoma. Researchers found that melanoma was significantly associated with brown discoloration of the background and irregular longitudinal lines. Nail apparatus nevus showed brown discoloration of the background but with regular lines.
Nail lentigo, ethnic type pigmentation, and drug-induced pigmentation were significantly associated with homogenous longitudinal thin gray lines and gray discoloration of the background.
Dr. Lipner awed us with her numerous studies in nail disorders (all of which are pure GOLD in my mind). At the end of her lecture, she wanted to emphasize these take-home points:
Take Home Messages
-
- Images for improved nail diagnosis in diverse populations.
- ILTAC is first line treatment for NP nail matrix disease.
- Need for race reporting in NP clinical trials.
- Indications for oral/topical onychomycosis therapy.
- Need for race reporting in onychomycosis clinical trials.
- Concerning features for LM and nail biopsy indications.
How often do you use dermoscopy to evaluate longitudinal melanonychia?
Have you encountered a patient with darker skin whose nail psoriasis was misdiagnosed?
Please share your comments at the end of this post and on Instagram @nextstepsinderm!
References
-
- Fathy R, Lipoff JB. Lack of skin of color in Google image searches may reflect under-representation in all educational resources. J Am Acad Dermatol. 2021 May 8:S0190-9622(21)00981-6. doi: 10.1016/j.jaad.2021.04.097. Epub ahead of print. PMID: 33971257.
-
- Adelekun A, Onyekaba G, Lipoff JB. Skin color in dermatology textbooks: An updated evaluation and analysis. J Am Acad Dermatol. 2021 Jan;84(1):194-196. doi: 10.1016/j.jaad.2020.04.084. Epub 2020 Apr 23. PMID: 32335181.
-
- Chang MJ, Lipner SR. Resources for skin of color images. J Am Acad Dermatol. 2021 Jun;84(6):e275-e277. doi: 10.1016/j.jaad.2021.01.040. Epub 2021 Jan 20. PMID: 33484764.
-
- Rigopoulos D, Baran R, Chiheb S, Daniel CR 3rd, Di Chiacchio N, Gregoriou S, Grover C, Haneke E, Iorizzo M, Pasch M, Piraccini BM, Rich P, Richert B, Rompoti N, Rubin AI, Singal A, Starace M, Tosti A, Triantafyllopoulou I, Zaiac M. Recommendations for the definition, evaluation, and treatment of nail psoriasis in adult patients with no or mild skin psoriasis: A dermatologist and nail expert group consensus. J Am Acad Dermatol. 2019 Jul;81(1):228-240. doi: 10.1016/j.jaad.2019.01.072. Epub 2019 Feb 5. PMID: 30731172.
-
- Lipner SR, Scher RK. Onychomycosis: Treatment and prevention of recurrence. J Am Acad Dermatol. 2019 Apr;80(4):853-867. doi: 10.1016/j.jaad.2018.05.1260. Epub 2018 Jun 28. PMID: 29959962.
-
- Wang Y, Geizhals S, Lipner SR. Retrospective analysis of laboratory abnormalities in patients prescribed terbinafine for onychomycosis. J Am Acad Dermatol. 2021 Feb;84(2):497-499. doi: 10.1016/j.jaad.2020.04.172. Epub 2020 May 7. PMID: 32387655.
-
- Wang Y, Lipner SR. Retrospective analysis of abnormal laboratory test results in pediatric patients prescribed terbinafine for superficial fungal infections. J Am Acad Dermatol. 2021 Oct;85(4):1042-1044. doi: 10.1016/j.jaad.2021.01.073. Epub 2021 Jan 27. PMID: 33515631.
-
- Kharghoria G, Grover C, Bhattacharya SN, Sharma S. Histopathological evaluation of nail lichen planus: A cross-sectional study. J Cutan Pathol. 2021 Jan;48(1):11-17. doi: 10.1111/cup.13783. Epub 2020 Sep 22. PMID: 32578239.
-
- Lipner SR, Scher RK. Evaluation of nail lines: Color and shape hold clues. Cleve Clin J Med. 2016 May;83(5):385-91. doi: 10.3949/ccjm.83a.14187. PMID: 27168515.
-
- Ko D, Oromendia C, Scher R, Lipner SR. Retrospective single-center study evaluating clinical and dermoscopic features of longitudinal melanonychia, ABCDEF criteria, and risk of malignancy. J Am Acad Dermatol. 2019 May;80(5):1272-1283. doi: 10.1016/j.jaad.2018.08.033. Epub 2019 Feb 11. Erratum in: J Am Acad Dermatol. 2020 Jan;82(1):260. PMID: 30765143.
-
- Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol. 2000 Feb;42(2 Pt 1):269-74. doi: 10.1016/S0190-9622(00)90137-3. PMID: 10642684.
-
- Ronger S, Touzet S, Ligeron C, Balme B, Viallard AM, Barrut D, Colin C, Thomas L. Dermoscopic examination of nail pigmentation. Arch Dermatol. 2002 Oct;138(10):1327-33. doi: 10.1001/archderm.138.10.1327. PMID: 12374538.
This information was presented by Dr. Sheri Lipner at the 2021 Skin of Color Update virtual conference held on September 10-12, 2021. The above highlights from her lecture were written and compiled by Dr. Jacqueline McKesey.
Did you enjoy this article? Find more on Medical Dermatology here.

