During the recent DERM2O22 NP/PA CME conference held July 28-31, 2022, Drs. David Cohen, Brad Glick, and Adam Friedman led a case-based panel discussion on atopic dermatitis (AD) treatment initiation and monitoring. This article provides a summary of their discussion and recommendations.
CASE 1
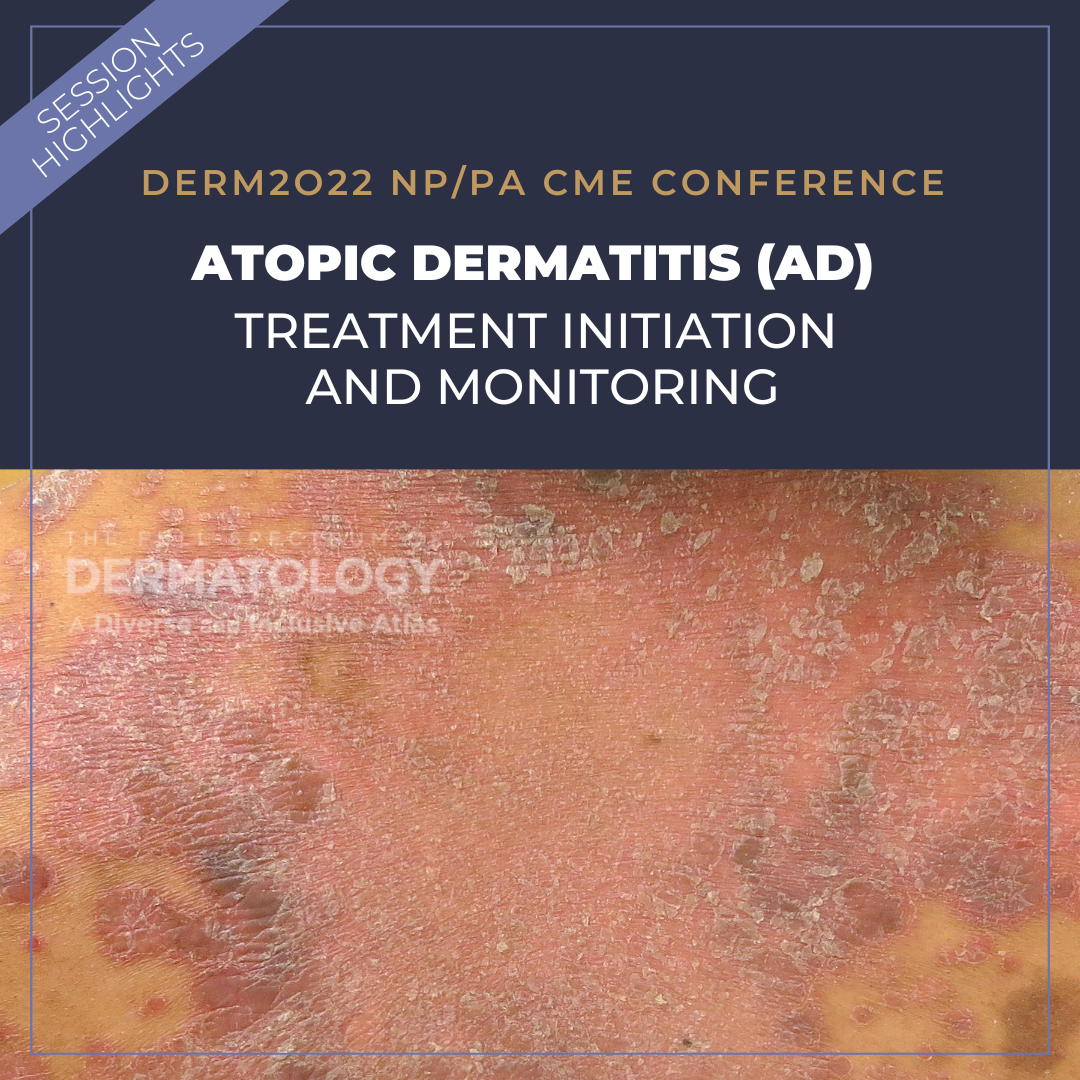
51-year-old male with a 20-year history of AD. The patient was first seen in September 2015 with BSA 25% involvement. He has a positive history for atopy with environmental allergies and allergic rhinitis. Patient reports photosensitivity and lack of sleep due to itching. Initially, the patient requested topical treatment only. Despite a rigorous topical regimen, the patient continued to flare.
Questions to ask:
1. Determine compliance: Is the patient adherent to the regimen?
2. Does the patient understand the nature of atopic dermatitis?
Approach: Try to optimize topical therapy and consider ultra-potent steroids. Still no improvement? Try alternative topical such as topical calcineurin inhibitors and/or crisaborole. After 18 months, the patient was still not at treatment goal.
Pro tip: Give the patient perspective! AD is a systemic disease, and he would benefit from systemic therapy. A band-aid on a gushing wound is not going to cover it.
Make sure the diagnosis is correct: Are we treating the right thing? Is this AD or AD with contact dermatitis? You don’t want to miss cutaneous t-cell lymphoma that is masquerading as AD.
Patch testing was performed and was negative. The patient continued to suffer with recurrent and unpredictable flares as well as uncontrolled itch. At this point, the patient was willing to consider systemic therapy. A short course of systemic steroids was initiated, as well as mycophenolate mofetil (MPM). He stabilized quickly with decreased cutaneous signs/symptoms including improved pruritus. The patient was finally able to sleep! However, after 1.5 years on MPM, he relapsed – Back to Baseline.
Patient agreed to try dupilumab. He reported facial rash, which was treated successfully with topical ruloxitinib. Unfortunately, 6 months into therapy, the patient flared again, and he reported alopecia and itchy, red eyes. He was evaluated by ophthalmology, with confirmed conjunctivitis.
What would you do next?
Consider acute treatments such as intramuscular steroids or cyclosporine. Plan on transitioning to a long-term treatment with quick onset such as JAK inhibitors. The patient was started on upadacitinib 15mg daily. Three months after initiation of upadacitinib, he reported nearly completely clear skin and marked decrease in itch!
CASE 2
A 6-year-old with atopic dermatitis managed primarily with emollients. The patient was started on topical therapies including topical steroids and crisaborole, without relief. For pediatric patients, systemic options include cyclosporine, azathioprine, methotrexate (MTX), and mycophenolate mofetil. The patient failed prednisolone and MTX. Although MTX was helpful, the patient experienced unrelenting GI upset, unresponsive to H2 blockers and other supportive therapies. The patient was started on dupilumab 300mg with improvement noted at week 4. Dose adjusted to 200mg every 2 weeks, once FDA approved, and the patient has remained clear since!
Helpful Tips for AD Treatment initiation and Monitoring
Atopic dermatitis can present with overlapping features of psoriasiform dermatitis. The panel recommends reviewing your differential diagnoses and consider performing multiple biopsies to rule in AD and rule out other concerning diagnoses such as CTCL, which commonly presents on sun protected areas of the skin.
How do you make the diagnosis?
-
- Document major and minor criteria (see below for complete list).
- Evaluate itch and document severity.
When starting therapy, always document start dates and carry it through your note. Obtain baseline labs to be able to switch medications without delaying treatment.
Two oral JAK inhibitors are now commercially available and FDA approved for treatment of atopic dermatitis.
Abrocitinib is a Janus kinase (JAK) inhibitor indicated for the treatment of adults with refractory, moderate-to-severe atopic dermatitis whose disease is not adequately controlled with other systemic drug products, including biologics, or when use of those therapies is inadvisable.
Abrocitinib dosing for patients ≥18yo – 100mg daily.
If an adequate response is not achieved after 12 weeks, consider increasing to 200mg daily.
Upadacitinib is a Janus kinase (JAK) inhibitor indicated for adults and pediatric patients 12 years of age and older with refractory, moderate to severe atopic dermatitis whose disease is not adequately controlled with other systemic drug products, including biologics, or when use of those therapies is inadvisable.
Upadacitinib dosing for patients ≥12yo – 65yo – 15 mg daily.
If an adequate response is not achieved, consider increased to 30mg daily. Use the lowest effective dose needed to maintain response.
JAK Inhibitor Suggested Monitoring Parameters
Baseline CBC & CMP
Fasting lipid panel 12 weeks after therapy initiation
Screening TB and viral hepatitis panel
Screening hCG if warranted
AD Diagnostic Criteria
Major Criteria – Need 3 or more:
-
- Pruritus
- Typical morphology and distribution
- Flexural lichenification in adults
- Facial and extensor involvement in children
- Dermatitis, chronic or chronically relapsing
- Personal or family history of asthma, allergic rhinitis, or atopic dermatitis
Minor Criteria – Need 3 or more:
-
- Xerosis
- Ichthyosis/palmar hyperlinearity, keratosis pilaris
- Immediate (type I) skin test reaction
- Elevated serum IgE
- Early age of onset
- Tendency toward cutaneous infections (especially staph. aureus and herpes simplex), impaired cell-mediated immunity
- Tendency toward non-specific hand or foot dermatitis
- Nipple eczema
- Cheilitis
- Recurrent conjunctivitis
- Dennie-Morgan infraorbital fold
- Keratoconus
- Anterior subcapsular cataracts
- Orbital darkening
- Facial pallor, facial erythema
- Pityriasis alba
- Anterior neck folds
- Itch when sweating
- Intolerance to wool ad lipid solvents
- Perifollicular accentuation
- Food intolerance
- Course influenced by environmental and emotional factors
- White dermographism, delayed blanch
References
Hanifin, J.M. and Rajka, G.: Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh) 1980; 92: 44–47
This information was presented by Drs. David Cohen, Brad Glick, and Adam Friedman at the DERM2O22 NP/PA CME conference held July 28-31, 2022. The above highlights from their lecture were written and compiled by Dr. Mojgan Hosseinipour.
Did you enjoy this article? Find more on Atopic Dermatitis here.