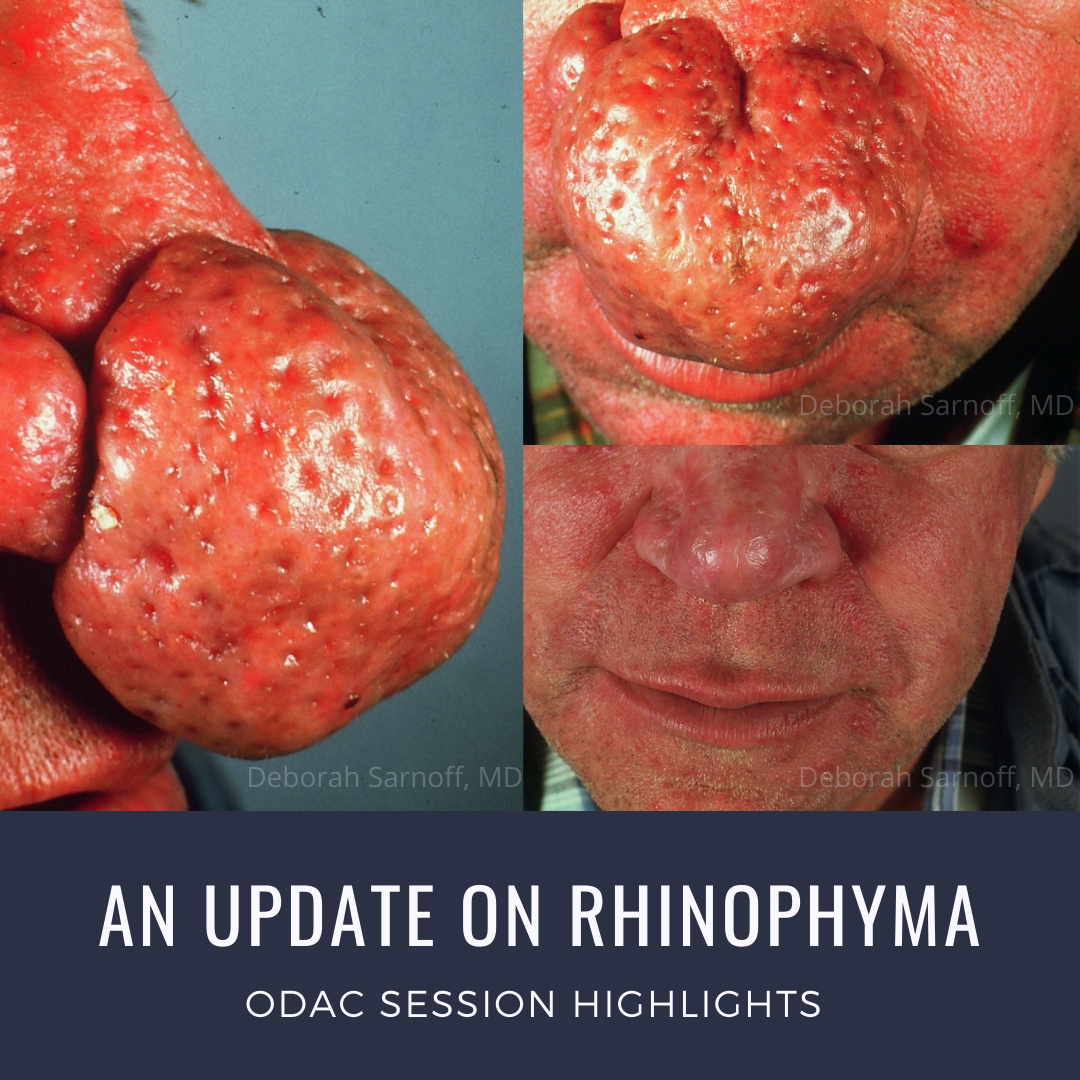
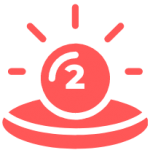
Gin nose. Gin blossom. Rum nose. Rum blossom. Brandy nose. Copper nose. Hammer nose. Potato nose. These are some of the disparaging terms that were once used to describe people suffering from rhinophyma. As can be seen, many imply the use of alcohol by the afflicted, which is sadly yet another example of the victim-shaming we so often observe when someone’s appearance or choices make others uncomfortable.
Why can’t we just be nice to each other?
An interesting historical anecdote that gives color to how psychosocially debilitating rhinophyma can be, involves JP Morgan, one of history’s most well-known financiers who was once described as America’s greatest banker. JP Morgan suffered from severe rhinophyma to the extent that he would not allow anyone to photograph him without his permission. In fact, there is a picture in the Library of Congress that depicts him, in one such scenario, attempting to strike a photographer with his cane. That one of the world’s most powerful and wealthy individuals would feel so self-conscious about having an unflattering image of his nose captured and potentially disseminated, speaks to the devastating effect that rhinophyma can have on how individuals with it are viewed—both by themselves and by everyone else.
At the 2020 ODAC Dermatology, Aesthetic and Surgical Conference, Dr. Deborah Sarnoff, Clinical Professor of Dermatology NYU School Of Medicine and Director of Dermatologic Surgery at Cosmetique Dermatology, Laser & Plastic Surgery, gave a fantastic lecture on Rhinophyma that taught me a lot of new perspectives on how it can negatively impact a patient, as well as what we have in our toolkit to try to treat it. (And if you missed it the first time, check out my previous post on how rosacea can present in skin of color here. Because we don’t just see rhinophyma in white men, and we need to try to catch it early when it develops)!
This post will provide an overview of the following considerations when treating rhinophyma:
-
- Who is at risk of developing it
- Psychosocial impact
- Functional impairment
- Options for treatment…and accompanying PEARLS (you know you love these)
But first, let me share a few of my “Aha!” moments from Dr. Sarnoff’s talk, in the hope that they will entice you to read on…
-
- When surgically reshaping rhinophyma, it is important to send tissue for histopathologic examination. This never occurred to me before. Read on to find out why this is crucial!
- Not sure how much is too much when it comes to sculpting a phymatous nose? Find out how much, and how you should approach this task, to avoid giving patients a potentially poorer outcome than what they started with. Keep reading!
- There are several options for the medical management of rosacea that were never on my radar prior to Dr. Sarnoff’s lecture. Gotta read on if you want to learn!
Who is at risk of developing rhinophyma
Although the archetypal rhinophyma patient is a white man in his 50s–70s, anyone who has rosacea can develop it. As your clinical experience has probably illustrated to you, the condition is much more common in men, with a 12-30:1 ratio. Relatedly, 21% of men with rosacea will develop rhinophyma, compared to only 8% of women (which still seems like a surprisingly high number to me based on what I’ve seen in clinic – how about you)?
Psychosocial implications of rhinophyma
The psychosocial implications of conditions such as psoriasis, atopic dermatitis, and hidradenitis suppurativa are widely discussed in the dermatology community, but I feel as though this is much less the case with rosacea. I know that there is room for me to do a better job of asking my rosacea patients about the impact their disease is having upon their quality of life, as well as how it makes them feel. We need to recognize that many patients may experience anything ranging from social embarrassment to a loss of self-esteem to depression, and more, as a result of their rosacea. These effects are likely worse for those with rhinophyma and other phymatous changes of the face, due to the progressive disfigurement that they cause, and the humiliation that one may feel when subject to the curious glances and reactions of others.
Functional problems associated with rhinophyma
Keep in mind that the disability that rhinophyma may cause is not just psychosocial, but also functional, in nature. Alar thickening may lead to airflow obstruction and consequent difficulty breathing while awake, as well as exacerbation of snoring and sleep apnea, and difficulty sleeping. If the nose is very enlarged, patients may also struggle with drinking from a cup, as well as eating things like ice cream and corn on the cob. Shame may prevent patients from volunteering these issues on their own, so as stated in the previous section, be sure to ask!
Surgical and energy-based treatment options for rhinophyma
Dr. Sarnoff’s preferred surgical modalities for treating rhinophyma include electrosurgery (electrodessication needle, loop cautery) and laser resurfacing with ablative lasers (CO2 and Er:YAG). And while these are her preferred options, they are by no means the only ones that exist. Other options that you might want to consider learning more about include dermabrasion, radiofrequency ablation, cryotherapy, excision with skin grafting. Excisions can be performed with a cold #15 blade (also known as cold steel surgery, decortication, or dermaplaning), or with a heated scalpel.
ASSOCIATED PEARLS
 Ask your patient to bring you a photo that clearly depicts the appearance of the nose before it changed. This will guide your efforts to reshape it.
Ask your patient to bring you a photo that clearly depicts the appearance of the nose before it changed. This will guide your efforts to reshape it.
 Remove slightly less tissue than planned to account for post-procedure fibrosis and contraction.
Remove slightly less tissue than planned to account for post-procedure fibrosis and contraction.
 Don’t go below the depth of the pilosebaceous apparatus! You must stay above this in order to preserve the nose’s normal pore pattern and color. If you go too deep, the nose will appear hypopigmented, shiny, and atrophic.
Don’t go below the depth of the pilosebaceous apparatus! You must stay above this in order to preserve the nose’s normal pore pattern and color. If you go too deep, the nose will appear hypopigmented, shiny, and atrophic.
 Send some tissue for histopathologic evaluation to rule out occult malignancies. Basal cell carcinomas may be observed in 3-10% of cases, and it may also be possible to identify squamous cell carcinoma, sebaceous carcinoma, angiosarcoma, B-cell lymphoma, and metastatic lesions.
Send some tissue for histopathologic evaluation to rule out occult malignancies. Basal cell carcinomas may be observed in 3-10% of cases, and it may also be possible to identify squamous cell carcinoma, sebaceous carcinoma, angiosarcoma, B-cell lymphoma, and metastatic lesions.
 It is safest to perform surgical procedures in stages—better outcomes will be had if you focus on debulking first, then fine-tuning later.
It is safest to perform surgical procedures in stages—better outcomes will be had if you focus on debulking first, then fine-tuning later.
Post-operative care
The aforementioned treatment options are going to expose a lot of dermis that will need to re-epithelialize. For this reason, it is important to perform wound care that is going to keep the treated area clean, as well as moist, but not too moist. Topical antibiotic ointments such as mupirocin and bacitracin can be used in conjunction with white petrolatum or xeroform dressings to provide a clean, moist barrier. In contrast, if there is an excessive amount of serous weepage from the treated area, then Domeboro compresses can be applied thrice daily to help dry things out. Finally, it is important to continue treating the patient’s rosacea during and after any procedural interventions, for all of the quality of life reasons previously mentioned, as well as to maintain your results!
Medical management
One of the most eye-opening parts of Dr. Sarnoff’s talk was focused on some of the more uncommon ways that rosacea can be medically managed. In addition to oral tetracycline antibiotics, and the various topicals that we are all so familiar with, there are several less well-known treatment options that you may want to consider incorporating into your patients’ treatment regimens if you are not able to get them under good control with more traditional approaches. But before I delve into these, let’s give a shout out to low dose isotretinoin, which at 5-10 mg daily for 6 – 12 months, is capable of reducing bulk if started early enough in the disease course. So don’t hesitate to go there, even if navigating iPledge may take more time—it can be in the best interest of the right patients!
Here are some other options to consider when medically managing your rosacea patients:
-
- Aspirin can decrease flushing via inhibition of prostaglandin synthetase.
- Propranolol or clonidine can also decrease flushing, as can histamine receptor blockers such as chlorpheniramine (H1-receptor blocker) and cimetidine (H2-receptor blocker).
- Vitamin B6 deficiencies have been linked to vasodilation in some cases, so supplementation may help.
- Botulinum toxin, by blocking the release of acetylcholine neurotransmission, can also decrease flushing when administered at a very dilute concentration all over the nose.
- Tamoxifen has been used to treat rhinophyma with some moderate success. It has been shown to downregulate the expression of TGF-2, which leads to decreased fibroblast activity. This is important because end-stage rhinophyma is associated with increased fibroblast activity, causing fibrosis via overexpression of TGF-2.
- In a similar vein, there are several antineoplastic drugs that are useful for fibroproliferative disorders, such as 5-FU, MTX, bleomycin, paclitaxel, mitomycin-C, that may hold future promise in the treatment of rhinophyma.
- Finally, there have been some really interesting recent articles that describe the successful use of hyaluronidase injections to improve microstomia caused by scleroderma. Might this have a role in rhinophyma as well? Will you be the one to find out??
How often do you ask your rosacea patients about the psychosocial and functional impacts their disease has upon their lives? Has this post inspired you to start? What is your go-to technique for treating rhinophyma? Have you tried any off the beaten path approaches that were mentioned in this post and, if so, what has your experience been?
Please tell us all about it in the comments at the end of this article and on Instagram @nextstepsinderm!
This information was presented by Dr. Deborah Sarnoff at the 17th Annual ODAC Dermatology, Aesthetic and Surgical Conference held January 17–20, 2020 in Orlando, FL. The above highlights from her lecture were written and compiled by Dr. Kimberly Huerth, Chief Dermatology Resident at Howard University.
Did you enjoy this article? Find more on Medical Dermatology topics here.