Rosacea is defined by facial erythema and telangiectasias, two features that are more difficult to appreciate in patients with skin of color. To refine our ability to diagnose rosacea in all skin types, on day two of the 2021 Skin of Color Update virtual conference, we had an informative, evidence-based lecture, “Recognizing, Diagnosing, and Treating Rosacea in Patients with Skin of Color,” by Dr. Hiliary Baldwin, medical director of the Acne Treatment & Research Center and clinical associate professor at Rutgers Robert Wood Johnson Medical Center. Dr. Baldwin emphasized the theme that while rosacea is not common in patients with skin of color, it is not rare, so we must keep this disease in mind for all patients.
Rosacea Statistics
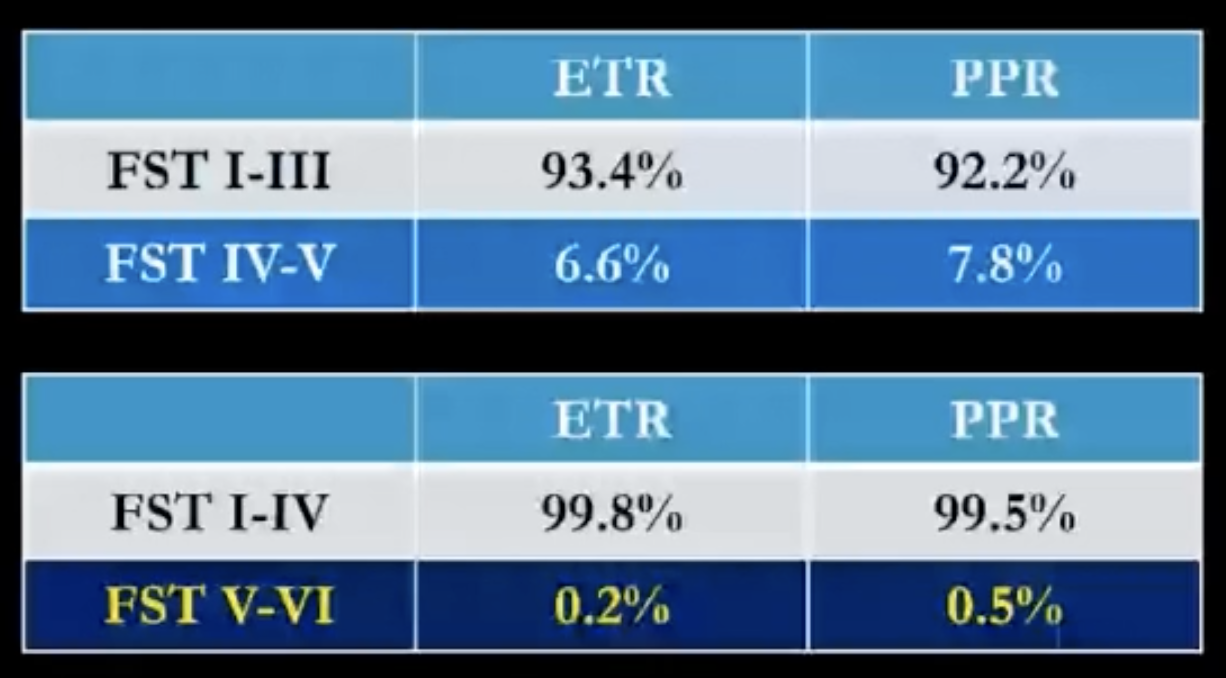
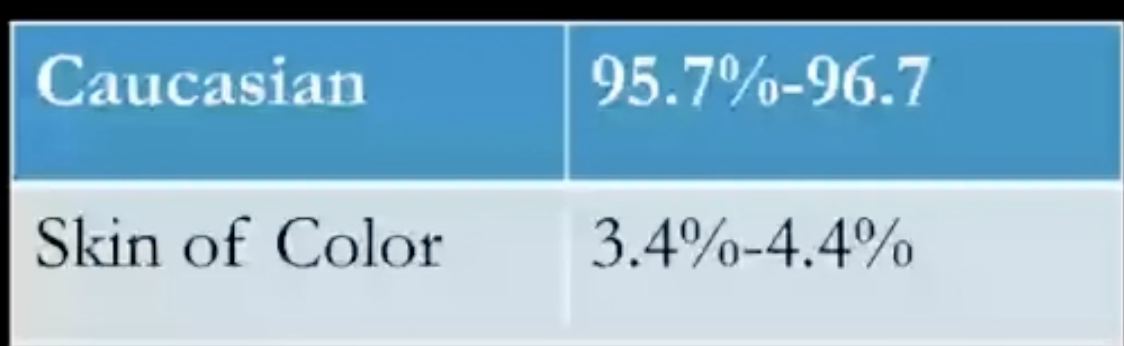
Dr. Baldwin started by reviewing data on the prevalence of rosacea in patients with skin of color. She shared data from personal communication with Dr. Fran Cook-Bolden showing that rosacea occurs in 6-8% of patients with Fitzpatrick skin type (FST) IV-V skin. When you restrict the grouping to FST V-VI skin, the percentage falls to 0.2-0.5%, possibly because the cardinal features of rosacea, erythema and telangiectasia, are harder to visualize in the darker skin types (figure 1a). Examining the data by race/ethnicity, rosacea occurs in 3-4% of patients with skin of color (figure 1b). Overall, this data shows that rosacea is not rare in skin of color, so we must consider this disease for patients all skin types. As Dr. Baldwin summarized, “A diagnosis not considered is a diagnosis not made.”
If we fail to consider rosacea in patients with skin of color, this will lead to misdiagnosis or delayed diagnosis. Delayed diagnosis of rosacea is especially troubling as it increases the risk of more advanced, often irreversible, outcomes including sight-threatening ocular disease, disfiguring phymas, or worsening telangiectasias. Dr. Baldwin highlighted the danger of ocular rosacea with a study of three black men who developed severe ocular rosacea with corneal abrasions, ulcers, and perforation after delays in diagnosis of cutaneous disease, despite the presence of phymas and papules.1 The author of this study erroneously concluded that this was the case because ocular rosacea is a “disease only of whites.”1 Dr. Baldwin emphasized our desperate need for new data so this fallacy is not further perpetuated.
Pathogenesis of Rosacea
While the pathogenesis of rosacea is poorly understood, monozygotic twin studies attest to its genetic predisposition. Based on a study of 233 monozygotic twins and 42 dizygotic twins, Aldrich et al showed that the genetic contribution to rosacea is about 46%.2 Environmental triggers also play a role, such as ultraviolet light exposure, alcohol use, smoking, age, and cardiac comorbidities.
Signs and Symptoms of Rosacea in Patients with Skin of Color
Cardinal features of rosacea include erythema and telangiectasias, which may be easier to appreciate on dermoscopy, as well as papules and pustules. Phymas can be seen but are less common in skin of color. Unlike acne, post-inflammatory changes do not occur from the skin disease.
Reported symptoms include stinging or burning, pruritus, and sensations of warmth. These sensations of warmth are episodic and may be akin to flushing. For ocular disease, patients report painful eyes, gritty sensations, and rheum or eye discharge. Sun exposure will worsen these symptoms. Patients also report sensitivity to skin products and medications.
Additionally, assessment of co-morbidities that can occur with rosacea is critical, including cardiac and gastrointestinal disease. The presence of gastrointestinal co-morbidities is especially compelling, with rosacea patients being 13 times per likely to have small intestinal bacterial overgrowth (SIBO).3 This association may be due to cross talk between the gut and skin. Dr. Baldwin prefers to have patients fill out an intake form with questions about medical problems rather than asking about these many co-morbidities, which can be unnerving to patients.
Rosacea Differential Diagnosis
Dr. Baldwin highlighted clinical pearls for distinguishing diseases that should also be in your differential diagnosis for patients with rosacea:
-
- Acne: look for comedones, which are essential to acne but should not be seen in rosacea.
- Steroid acne: this monomorphic eruption is commonly seen in patients with rosacea who will use topical steroids in attempts to reduce inflammation.
- Rosacea dermatitis: some feel this entity is an overlap between seborrheic dermatitis and rosacea, while others believe it is a type of rosacea. Based on Dr. Baldwin’s clinical experiences, she thinks rosacea dermatitis is a subtype of rosacea given it typically resolves with rosacea treatment alone.
- Periorificial dermatitis: differs from rosacea by the presence of monomorphic papules and the location, occurring around the mouth, nose, and eyes.
- Lupus erythematosus: the malar rash of lupus can mimic rosacea.
- Sarcoidosis: papules of sarcoidosis are shiny and translucent, unlike papules and pustules seen in rosacea.
Rosacea Treatment
Dr. Baldwin then shared her expertise for formulating a treatment plan. The first and most important step is listening to your patient’s symptoms. It may be easier to hear about symptoms of warmth, flushing, or stinging than to appreciate erythema and telangiectasias. Next, she evaluates signs of disease while patients hold a mirror, inquiring about which features are most important to them. After discussing treatment options, she manages expectations by explaining that rosacea is a chronic illness requiring long-term treatment.
In patients with skin of color especially, the treatment goal is clear skin to reduce the risk of recurrence, using tolerable therapies to reduce the risk of post-inflammatory hyperpigmentation from medication side effects. The two topical therapies with the best tolerability data are ivermectin 1% cream and minocycline 1.5% foam.4,5 When using vasoconstrictors, limit the amount applied to reduce irritation. In addition, Dr. Baldwin recommends application of moisturizer before therapy and considering a dedicated period of barrier repair before therapy. The utility of barrier repair is demonstrated by a study where patients applied vehicle cream daily for one month followed by azelaic acid 15% gel.5 With this order of application, skin pain occurred in only 5% of patients who used azelaic acid, compared to around 20% in the original study on azelaic acid.5
Given SIBO is more likely in patients with rosacea, another interesting therapy is rifaximin. In a small study of 28 patients with rosacea and SIBO, rosacea cleared in 20 of 28 patients in the rifaximin group.6 In the placebo group, 18 of 20 remained unchanged and the other 2 patients experienced worsening of disease.6
Further, an emerging therapy with promising results is microencapsulated benzoyl peroxide (BP), where the BP crystal is encased in a silica shell. Lipids and phospholipids migrate through the shell and dissolve BP slowly. With this slow degradation, the skin is exposed to smaller, less irritating amounts of BP.
In addition to the above therapies, Dr. Baldwin also reviews gentle skin care routines and cosmetic application techniques, which she calls “fard” (definition: apply cosmetics in order to conceal facial blemishes). She instructs patient to wash with a gentle cleanser only nightly, apply silicone-based moisturizers daily, and use physical sunblock with zinc oxide. For cosmetic application, avoid heavy cosmetics that require scrubbing for removal and use products with a matte finish rather than shiny finish, which can cause pruritus. Patients can also add a green tint to their foundation to hide erythema.
In summary, Dr. Baldwin emphasized the importance of keeping a high index of suspicion for rosacea in patients with skin of color. By keeping this diagnosis in mind, you can avoid delays in treatment and reduce the progression of disease! When creating a treatment plan, remember to listen to your patients’ concerns, focus on moisturization in addition to treatment, and review skin care and cosmetic routines. With these tips, you will reduce the risk of irritation with therapy, which can lead to unwanted, difficult to treat pigmentary changes.
References
-
- Browning DJ, Rosenwasser G, Lugo M. Ocular Rosacea in Blacks. American Journal of Ophthalmology. 1986;101(4):441-444. doi:10.1016/0002-9394(86)90644-6
- Aldrich N, Gerstenblith M, Fu P, et al. Genetic vs Environmental Factors That Correlate With Rosacea: A Cohort-Based Survey of Twins. JAMA Dermatol. 2015;151(11):1213-1219. doi:10.1001/jamadermatol.2015.2230
- Parodi A, Paolino S, Greco A, et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008;6(7):759-764. doi:10.1016/j.cgh.2008.02.054
- Stein Gold L, Del Rosso JQ, Kircik L, et al. Minocycline 1.5% foam for the topical treatment of moderate to severe papulopustular rosacea: Results of 2 phase 3, randomized, clinical trials. J Am Acad Dermatol. 2020;82(5):1166-1173. doi:10.1016/j.jaad.2020.01.043
- Stein Gold L, Kircik L, Fowler J, et al. Efficacy and safety of ivermectin 1% cream in treatment of papulopustular rosacea: results of two randomized, double-blind, vehicle-controlled pivotal studies. J Drugs Dermatol. 2014;13(3):316-323.
- Weinstock LB. Rosacea in Crohn’s Disease: Effect of Rifaximin. J Clin Gastroenterol. 2011;45(3):295-296. doi:10.1097/MCG.0b013e3182040eb2
This information was presented by Dr. Hilary Baldwin at the 2021 Skin of Color Update virtual conference held on September 10-12, 2021. The above highlights from her lecture were written and compiled by Dr. Emily Murphy.
Patient image used with permission from the Journal of Drugs in Dermatology.
Did you enjoy this article? You can find more on Medical Dermatology topics here.