Our new series, “The Many Faces of”, showcases side-by-side images of some of the most commonly seen dermatology conditions in an array of skin tones and briefly highlight nuances in clinical presentation. All images featured in the series are part of The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, a resource developed by co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD, and published by SanovaWorks and Educational Testing & Assessment Systems.
If your patient is enjoying the outdoor summer sun, this could also mean increased melanin or melasma. As you can see from the images, melasma can affect any skin type and tone, though it may be more appreciable in lighter skin tones due to the wider contrast between unaffected background skin and the melasma patches.
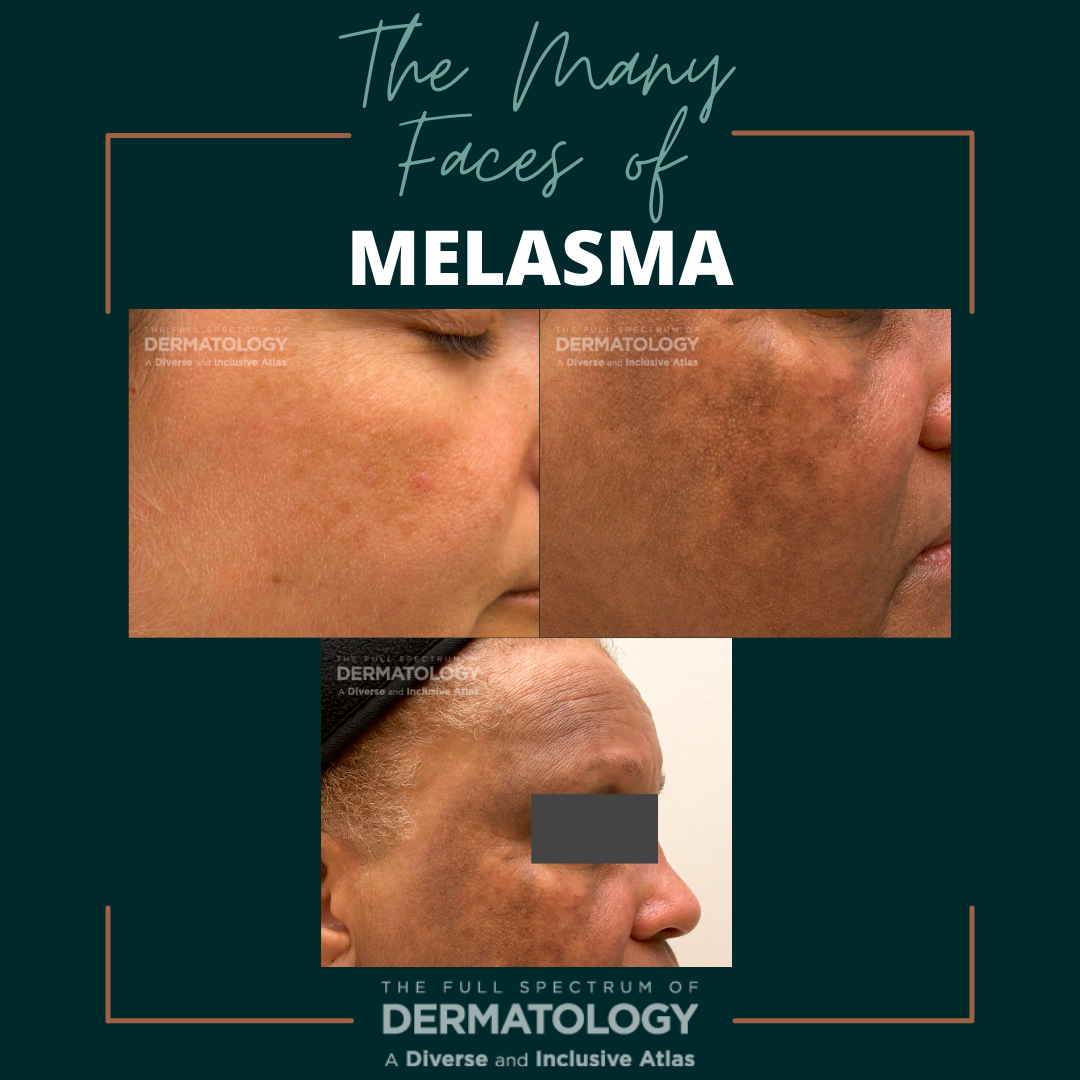
Melasma is an acquired chronic dermatologic condition most often appearing as confluent hyperpigmented macules and patches with the classic “moth-eaten appearing borders” in photo-exposed areas. In those individuals with lightly pigmented skin, you will notice tan to light brown patches in contrast to the dark brown to black patches seen in deeply pigmented skin. Melasma is typically seen on the face (cheeks, forehead, nose, and upper lip), but can also be found on the neck, chest, and upper extremities as these areas are also heavily exposed to the sun. Melasma can occur in all genders and skin tones, though it is often more commonly seen in females with darker skin (e.g. Asian, Hispanic/Latino, Black). Risk factors for the development of melasma include ultraviolet and visible light, high levels of estrogen, and family history. Histopathologic findings can include vacuolization at the basement membrane, increased melanin in the basal and suprabasal layers of the epidermis with increased melanosomes and prominent dendrites. An interesting fact to note is that the total melanocyte number is not increased in melasma, which may be surprising. An increase in mast cells and blood vessels in the affected skin has also been reported.
Treatment includes topical lightening creams that contain hydroquinone, azelaic acid, kojic acid, ascorbic acid and cysteamine. Oral and topically compounded tranexamic acid has also been utilized for the treatment of melasma and hyperpigmentation. Various procedural treatments that have been successful include chemical peels, micro-needling, intradermal injections, and laser therapy.
Practical Pearls
Regardless of the treatment(s) choice for melasma, it is important to educate patients that melasma is a chronic condition that often recurs, especially with re-exposure to UV light. Photoprotection is a vital step with any treatment, with preference for mineral-based sunscreens SPF30+ containing titanium or zinc. Tinted sunscreens with iron oxide are also preferred specifically for melasma as they help to block visible light, which is also a known exacerbating factor of melasma.
Further Reading
If you would like to read about melasma, check out the following articles:
Acknowledgements
We thank co-editors Misty Eleryan, MD, MS, and Adam Friedman, MD for reviewing the content of this article.
Reference
Eleryan, Misty, and Adam Friedman. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. SanovaWorks, 2021.
NOW AVAILABLE! Visit the online image gallery for The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas, where you will find high-quality images that you will be able to use, free of charge, for non-commercial educational purposes. Access the online gallery here.
The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas DIGITAL EDITION is available for purchase here.
Did you enjoy this article? You can find more here.

