Partnering Medical Therapies and Procedural Interventions to Treat the Whole Patient
Over the last decade, tremendous advances have revolutionized the treatment of chronic inflammatory skin conditions such as atopic dermatitis and psoriasis. These dermatological victories have shed light on skin diseases that need more attention. Hidradenitis suppurativa (HS), which disproportionately affects patients with skin of color, has gained national attention in the dermatology community as an orphaned disease. HS poses a therapeutic challenge as no effective monotherapy currently exists, requiring providers to be savvy and tenacious to help the patients impacted by this disease.
At the 2020 Skin of Color Virtual Update, Dr. Ginette Okoye discussed Managing Hidradenitis Suppurativa in the Skin of Color Patient. Dr. Okoye provided a review of important clinical factors of this chronic inflammatory disease and practical tips in its treatment, sharing her holistic approach to the HS patient.
First, let’s review a few highlights about HS:
 Hidradenitis suppurativa is a chronic inflammatory disease of the hair follicle affecting the intertriginous areas of the skin. HS can also present as part of the follicular occlusion tetrad, which includes dissecting cellulitis, acne conglobata, and pilonidal cysts.
Hidradenitis suppurativa is a chronic inflammatory disease of the hair follicle affecting the intertriginous areas of the skin. HS can also present as part of the follicular occlusion tetrad, which includes dissecting cellulitis, acne conglobata, and pilonidal cysts.
 Due to the high inflammatory burden, patients with hidradenitis suppurativa are at high risk of developing other diseases, such as pyoderma gangrenosum, inflammatory bowel disease, cardiovascular disease, metabolic syndrome, depression, and squamous cell carcinoma.
Due to the high inflammatory burden, patients with hidradenitis suppurativa are at high risk of developing other diseases, such as pyoderma gangrenosum, inflammatory bowel disease, cardiovascular disease, metabolic syndrome, depression, and squamous cell carcinoma.
 Quality of life scores among patients with HS are lower than those with psoriasis.
Quality of life scores among patients with HS are lower than those with psoriasis.
 The overall prevalence is estimated at 0.1% of the population, noted for a 2:1 female predominance, with African Americans 2-3 times more likely to be affected.
The overall prevalence is estimated at 0.1% of the population, noted for a 2:1 female predominance, with African Americans 2-3 times more likely to be affected.
 HS is associated with low socioeconomic status (SES), smoking, and obesity. Dr. Okoye proposed low SES results in limited access to care, differences in diet, obesity, and an altered microbiome, increasing the risk of HS. Further, patients with HS are more likely to have low SES due to loss of educational opportunities and employment due to their chronic skin disease and the associated co-morbidities.
HS is associated with low socioeconomic status (SES), smoking, and obesity. Dr. Okoye proposed low SES results in limited access to care, differences in diet, obesity, and an altered microbiome, increasing the risk of HS. Further, patients with HS are more likely to have low SES due to loss of educational opportunities and employment due to their chronic skin disease and the associated co-morbidities.
So how do we go about treating HS?
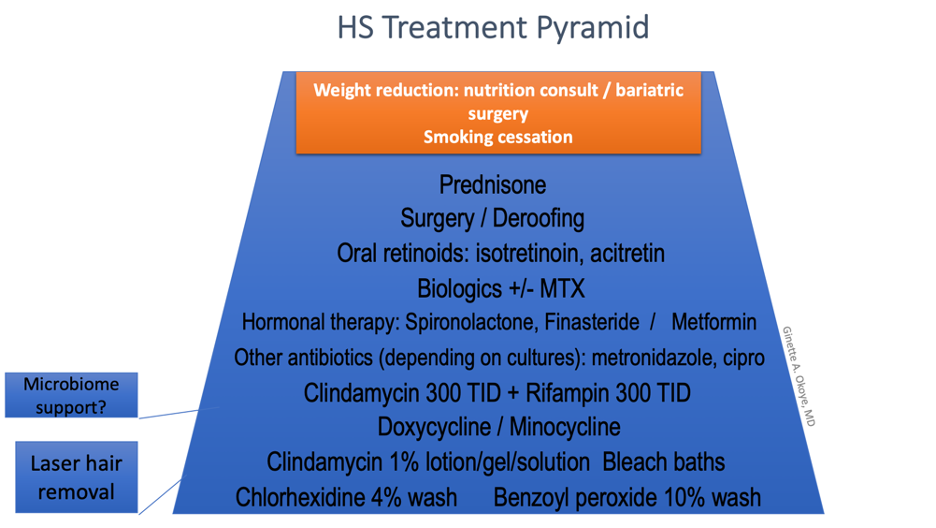
The current targets of therapy lie within the multifactorial model of hidradenitis suppurativa pathogenesis. At the root, hyperkeratinization of the follicular infundibulum leads to follicular occlusion. This causes subsequent rupture of the dilated follicle, spilling keratin, bacteria, and yeast into the dermis, resulting in inflammation. Further, there are alterations in the host immunity resulting in an inappropriate immune response to these follicular contents and commensal flora. Additional factors that contribute to this pathogenesis are bacterial colonization, genetic predisposition, obesity, diet, hormonal signaling, and smoking. To tackle this complex pathogenesis, treatment strategies go after individual pieces of this complex puzzle: the microbiome, the hair follicle itself, hormones, inflammation, etc. By layering therapies targeting these areas, clinical improvement can be achieved in the skin disease experienced by the patient.
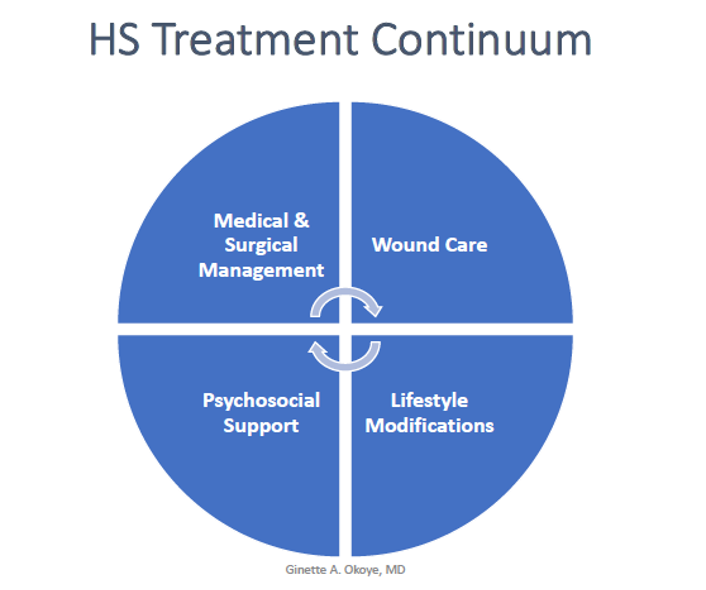
Dr. Okoye revealed a shift in her treatment strategy from a “stepwise ladder” focusing on medical and surgical treatment options to a more holistic approach to the patients, incorporating wound care, lifestyle modification, and psychosocial support in addition to the medical and surgical management. She emphasized a “layer and rotate” approach to the medical treatment.
To determine an individual treatment plan, Dr. Okoye recommended some key tips:
-
- Take into account the severity experienced by the patient, the psychosocial impact, and the family planning of the patient.
- Set expectations for improvement. This has to be defined with the patient so treatment efficacy is interpreted under the same understanding, whether that is less drainage, fewer active nodules, fewer flares, or shorter duration of flares.
- Consider co-morbidities and assessing the patients for hypertension, diabetes, obesity, polycystic ovarian syndrome (PCOS), and inflammatory bowel disease. Dr. Okoye recommended getting basic blood work (CBC, CMP, lipid panel, HgA1C) and vitals during visits because many patients may not have a primary care provider.
- Consider cost of the treatments, both in terms of financial cost and the cost of lost opportunity to their lifestyle, such as infusions causing missed days of work.
- Involve caregivers and parents in the treatment plan. Involve the PCP.
- Refer for psychosocial support, nutrition, wound care, surgery.
- Layer and rotate therapy.
In addition to these helpful considerations, Dr. Okoye highlighted three treatment modalities in greater detail: the benefits of laser hair removal and other minimally invasive procedures that can be done in the clinic, and highlighted the use of metformin in HS patients.
Laser hair removal with the Nd:YAG:
Because hyperkeratinization of the follicular infundibulum lies at the root of hidradenitis suppurativa pathogenesis, epilation removes this nidus of inflammation. Further, the thermal injury of laser hair removal kills microbes such as Candida albicans, Enterococcus faecalis, and Porphyromonas gingivalis. Dr. Okoye referred to a randomized controlled trial that demonstrated a 50-75% reduction in disease severity in Hurley II and II HS, with emphasis of greater efficacy in early disease. Here are a few of Dr. Okoye’s practical tips:
-
- Topical anesthesia can be used prior to treatment
- Recommended settings: 18-30 J/cm2, 20-40ms, 10mm spot size
- Unlike routine laser hair removal, for HS it is advised to pulse stack over nodules and to treat the skin surrounding the nodules in a rosette pattern with 20-30% overlap. The goal is to heat up the nodule to harness thermal injury for an antimicrobial effect.
- Insurance coverage for laser hair removal for HS is a major barrier for patients – please consider discounting this treatment for HS patients!
Surgical management
Although incision and drainage (I&D) procedures are common practice in the ED for inflamed, draining nodules, this strategy is not usually effective for HS patients. Dr. Okoye discouraged the use of I&D for HS due to the high risk of recurrence. She rather recommends intralesional steroids (e.g. Kenalog 20mg/cc) or deroofing procedures. It is important for HS patients to know that they can have an urgent appointment in the clinic and do not have to go to the ED!
Deroofing, also called marsupialization, refers to the surgical removal of the roof of a sinus tract or HS nodule. This strategy has a much lower risk of recurrence (approximately 15%) than with I&D and can be done under local anesthesia. Dr. Okoye advised healing time is approximately 6-8 weeks, and most patients report an improvement in their pain after deroofing despite the wound created. Deroofing also has lower morbidity and cost compared to radical excision. The main disadvantage is that this procedure is only an option for relatively small nodules and sinuses, and it is not always possible to tell how big a sinus tract is until it is unroofed.
Here is a step-by-step guide to deroofing:
-
- Mark the extent of the lesion
- Prep the area with chlorhexidine and perform a ring block with lidocaine with epinephrine. Numb wide!
- Make a defect in the top using a scalpel or punch tool.
- Introduce a probe to define the length of the sinus tract.
- Cut alongside the probe and remove the roof. Always send for pathology! It is important to rule out SCC and Crohn’s disease.
- Curette the gelatinous material at the base and rinse with sterile saline.
- Inspect the walls of the defect for branching points. Repeat the process if branching sinuses are identified.
- Apply petrolatum, gauze, and a transparent bandage for 2-3 days.
- Use CPT codes 10060 (simple) and 10061 (complicated or multiple) for this procedure.
Metformin
While the main indication for treatment is diabetes, metformin has demonstrated efficacy to reduce inflammation and fibrosis. In addition to its effect on insulin resistance, metformin helps decrease ovarian estrogen production. Dr. Okoye highlighted this therapy for its utility in HS patients.
Here are the main points:
-
- Consider metformin as an adjunct therapy for any patient with diabetes, PCOS, or any clinical signs of insulin resistance (e.g. acanthosis nigricans, skin tags, central obesity, hypertension).
- The extended-release formula makes for convenient once-daily dosing. Dr. Okoye recommends to start with metformin 500mg ER with the evening meal and increase by 500mg every 2-4 weeks until goal dose is reached (1500-2000mg daily)
- The main side effects are gastrointestinal (diarrhea, nausea, vomiting) while lactic acidosis is exceedingly rare. Patients should be advised to discontinue metformin prior to contrast imaging studies. Metformin is contraindicated in renal disease (GFR <45 ml/min) and hepatic impairment.
- Be advised metformin is not an option for a patient on the combination of rifampin and clindamycin because of the interaction with rifampin. Concurrent rifampin therapy increases metformin serum concentration.
- Metformin is Category B during pregnancy.
This information was presented by Dr. Ginette Okoye during the 2020 Skin of Color Update Virtual conference held on September 12-13, 2020. The above highlights were written and compiled by Dr. Edita Newton.
Did you enjoy this article? Find more on Skin of Color topics here.

